Characteristics Of The Population
Socio-demographic and clinical characteristics are summarized in . The study included 100 PD and 100 SCZ patients . There was no difference between the two groups in regards to anxiolytics, antidepressant drug or sedative-hypnotic drug ratios.
Table 1 Sociodemographic and medical details of Parkinsons disease and schizophrenia patients .
What Treatments Are Available For Parkinsons Psychosis
Your doctor may first reduce or change the PD medication youre taking to see whether that reduces psychosis symptoms. This is about finding a balance.
People with PD may need higher doses of dopamine medication to help manage motor symptoms. But dopamine activity shouldnt be increased so much that it results in hallucinations and delusions. Your doctor will work with you to find that balance.
Medications To Help Treat Parkinsons Disease Psychosis
Your doctor might consider prescribing an antipsychotic drug if reducing your PD medication doesnt help manage this side effect.
Antipsychotic drugs should be used with extreme caution in people with PD. They may cause serious side effects and can even make hallucinations and delusions worse.
Common antipsychotic drugs like olanzapine might improve hallucinations, but they often result in worsening PD motor symptoms.
Clozapine and quetiapine are two other antipsychotic drugs that doctors often prescribe at low doses to treat PD psychosis. However, there are concerns about their safety and effectiveness.
In 2016, the approved the first medication specifically for use in PD psychosis: pimavanserin .
In clinical studies , pimavanserin was shown to decrease the frequency and severity of hallucinations and delusions without worsening the primary motor symptoms of PD.
The medication shouldnt be used in people with dementia-related psychosis due to an increased risk of death.
Psychosis symptoms caused by delirium may improve once the underlying condition is treated.
There are several reasons someone with PD might experience delusions or hallucinations.
Read Also: Parkinson’s Foods To Eat
Risk Factors For Psychosis
Not everyone with Parkinsons will develop hallucinations or delusions, but there are several things can increase your risk:
- Dementia or impaired memory
- Depression: Individuals suffering from depression and PD are at a greater risk. In addition, severe depression alone can cause psychosis.
- Sleep disorders, such as vivid dreaming. Individuals commonly report vivid dreaming prior to the onset of psychosis. Other associated sleep disturbances include REM sleep disorder and general insomnia.
- Impaired vision
- Use of PD medications
Risk Factors For Parkinsons Hallucinations
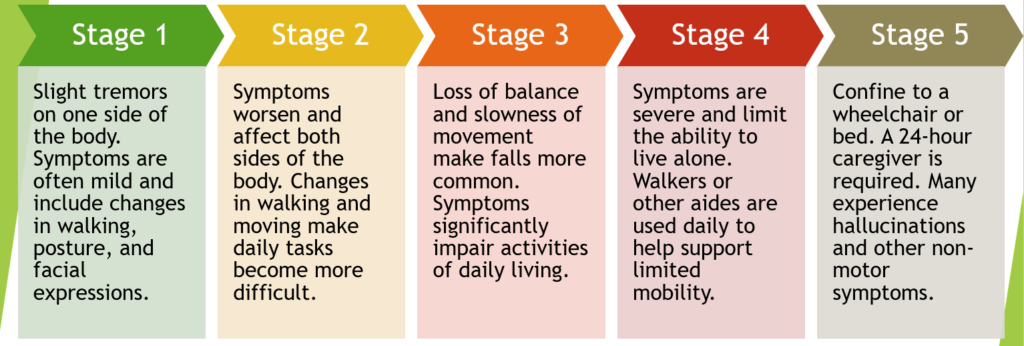
Not much is known about what causes hallucinations with Parkinsons disease. Because people living with Parkinsons disease also are at risk of vision impairment, these problems may contribute to the occurrence of hallucinations. Older people and those with advanced stages of Parkinsons also tend to have a higher risk of hallucinations.
Hallucinations can be a side effect of a medication or caused by an infection. In these cases, the hallucinations are related to Parkinsons but not caused by the disease itself.
Also Check: Communicating With Parkinson’s Patients
The Cause Of Parkinsons Delusions And Hallucinations
Some risk factors associated with the development of psychosis in Parkinsons disease include:
- Age: Parkinsons disease usually occurs in people over age 60.
- Duration and severity of Parkinsons disease: Psychosis is more common in advanced or late-stage Parkinsons disease.
- Later onset: Occurring later in life
- Hyposmia: A decreased sense of smell
- Cognitive impairment: Problems with thinking, including trouble remembering, difficulty learning new things, difficulty concentrating, problems making decisions that affect everyday life
- Depression: People who have both depression and Parkinsons disease are at a greater risk of developing psychosis.
- Diurnal somnolence: Daytime sleepiness
- REM sleep behavior disorder: A sleep disorder in which you physically act out dreams involves making vocal sounds and sudden, often extreme, arm and leg movements during REM sleep
- Visual disorders: Impaired vision
- Severe axial impairment: Speech, swallowing, balance, freezing of gait
- Autonomic dysfunction: Impairment of the autonomic nervous system , which controls involuntary or unconscious actions such as heart rate, breathing, body temperature, blood pressure, digestion, and sexual function
- High medical comorbidity: The existence of more than one condition or illness in the same person at the same time with Parkinsons disease, may include conditions such as dementia, depression, and sleep disorders
What Causes Parkinsons Disease Psychosis
Parkinsons is a brain disorder associated with a loss of dopamine-producing nerve cells deep inside the brain. Dopamine is a neurotransmitter that helps regulate the bodys movement, and it also allows us to think clearly and regulate our emotions. When you try to replace the dopamine thats been lost in a person with Parkinsons, it can cause the system to get out of whack which can impact thinking, how visual things are processed and more. Parkinsons disease psychosis is therefore typically a side effect of the disease itself or the medications used to manage it.
As a result, its an ongoing balancing act for Parkinsons doctors to prescribe enough dopamine to control a person with Parkinsons motor symptoms, but not so much that the person experiences hallucinations and/or delusions.
Read Also: Moringa And Parkinson’s Disease
Network Changes And Thalamic Drivers
Visual hallucinations have fascinated neurologists and neuroscientists for many years, with their tantalisingly rich and often narrative detail. Due to their transient nature, they have been challenging to investigate, with no clear mechanism found, but many theories have been proposed. Previous models for visual hallucinations considered them as cortical release phenomena, where spontaneous activity occurs in the absence of visual stimuli. Alternative models suggested that hallucinations arise due to incorrect binding of objects into visual scenes.
Advances in computational modelling and network neuroscience have opened up approaches to understanding the brain in new ways. Recent models suggest that Parkinsons hallucinations could arise due to a shift in dominance of difference networks. Specifically, there is thought to be a breakdown in those networks directed to attention and perception, and overactivity of the default mode network ,, a large-scale network that becomes activated during rest, and in day dreaming and mind-wandering. Indeed abnormal levels of default mode network activation are seen in patients with Parkinsons hallucinations.
Adapted from Zarkali A, Adams RA, Psarras S, Leyland LA, Rees G, Weil RS. Increased weighting on prior knowledge in Lewy body-associated visual hallucinations. Brain Commun. 2019 1:fcz007. doi:10.1093/braincomms/fcz007
What Are The Symptoms Of Psychosis
Two of the most prominent symptoms are hallucinations and delusions.7 Hallucinations involve seeing, hearing, experiencing or sensing things that are not really there. Delusions are false beliefs that are not based in reality. In describing symptoms of Parkinsons disease psychosis, patients may use such common terms as: seeing things, paranoia, flashbacks, nightmares, false beliefs, or not being in touch with reality.8
Read Also: What Is The Life Expectancy Of A Person With Parkinson’s
Parkinsons Disease Psychosis: Hallucinations Delusions And Paranoia
As part of Parkinsons Disease and its treatment, hallucinations, illusions, delusions, suspiciousness and paranoid behaviors occur in over 50% of patients. In this 1-hour webinar Dr. Christopher Goetz suggests lifestyle changes, medication adjustments and a recently FDA approved drug to specifically treat psychosis in Parkinsons Disease.
What Are Hallucinations
Hallucinations are when someone sees, hears or feels something that is not actually there. They are best described as deceptions or tricks played by the brain that involve the bodys senses. Hallucinations are not dreams or nightmares. They happen when the person is awake and can occur at any time of day or night.
Recommended Reading: Do Tremors Come And Go With Parkinson’s
Thanks For Signing Up
We are proud to have you as a part of our community. To ensure you receive the latest Parkinsons news, research updates and more, please check your email for a message from us. If you do not see our email, it may be in your spam folder. Just mark as not spam and you should receive our emails as expected.
Practical Tips For Caregivers Of People With Parkinson’s Psychosis
This 2-page tip sheet has bullet point suggestions for what to do if the person you care for experiences hallucination, delusions or confusion, or becomes agitated or aggressive. In addition, there are tips for how to best be prepared for a doctors appointment when you bring this behavior to the attention of your medical team.
Don’t Miss: What Is The Prognosis For Parkinson’s Disease
Changing Up Meds Can Help
If psychosis in PD does require treatment, the first thing your doctor will do is to consider altering your Parkinsons medication regimen, since some drugs can make psychosis symptoms worse. The first step is to evaluate how much medication the patient is on. And, if they’re on high doses of medication, to reduce the medication burden and see if we can reach a happy medium between having them take enough medication to help their motor symptoms and still reduce the psychosis as a complication, explains Dr. Pan.
Demystifying Hallucinations Night Terrors And Dementia In Parkinsons
This two-hour webinar includes extensive discussion about hallucinations, delusions, illusions and other examples of Parkinsons psychosis in Parkinson’s. Presenters: Rohit Dhall, MD, MSPH and Vergilio Gerald H. Evidente, Director, Movement Disorders Center of Arizona in Scottsdale. Pay particular attention to Dr. Rohit Dhalls description of the causes of PD psychosis as well as treatment options and what to discuss with your movement disorder specialist. Dr. Evidente gives a clear description on differences in PD dementia, Alzheimer’s and other dementias.
Don’t Miss: Multiple System Atrophy Vs Parkinson’s
What Should I Do Once The Hallucination Passes
After the hallucination passes, you can try to talk through the experience together. If the person has insight, it may be easier for them to understand and talk about what just happened.
Write down what happened during the hallucination. Note the time of day and what the person was doing when it started.
Taking notes each time it happens can help you identify the triggers. It could be related to the timing of medication, and your loved one might feel a sense of relief and control in knowing that pattern.
Ask what you can do to stop it from happening again. This might include adjusting their medication dosage or adding an atypical antipsychotic drug to their medication regimen.
Hallucinations And Delusions In Parkinsons Disease
It might be surprising to learn that 20 to 30 percent of people with Parkinsons disease will experience visual hallucinations. While typically not a symptom of PD itself, they can develop as a result to a change in PD medication or as a symptom of an unrelated infection or illness. It is important to know the signs of hallucinations and how to manage them.
Hallucinations and other more severe perceptual changes can be distressing to family often more so than to the person experiencing them. For the well-being of people with PD and caregivers, it is important to identify hallucinations as early as possible and take steps to reduce them.
The following article is based on the latest research and a Parkinsons Foundation Expert Briefings about hallucinations and delusions in Parkinsons hosted by Christopher G. Goetz, MD, Professor of Neurological Sciences, Professor of Pharmacology at Rush University Medical Center, a Parkinsons Foundation Center of Excellence.
Also Check: Best Books On Parkinson’s Disease
Whats The Treatment For Parkinsons Disease Psychosis
The single most important thing to do when it comes to Parkinsons disease psychosis is to tell your care providers and partners the minute you notice changes in your vision, hearing, thinking and behavior. The earlier they know whats going on, the sooner they can begin interventions to help you feel better.
Once you bring your concerns up to your doctor, they will typically do a clinical evaluation, review your medications and dosage, assess your lifestyle and determine the severity of your symptoms. Depending upon what they find, they may refer you to counseling or therapy, adjust your medication, change your medication, eliminate medication or do all of the above. If none of those strategies work, they may try antipsychotic drug therapy to see if they can adjust chemical levels in the brain. This can bring with it an entirely different set of problems so its important to be invested every step along the way and be sure youre well-informed before you move in that direction.
How Are They Treated
Your medical team should be aware of non-motor issues, just like your physical symptoms. Internists, neurologists, and psychiatrists together can help determine the right course for each person.
There are antipsychotic medications that are safe and can help to reduce the symptoms of Parkinson’s disease psychosis, but there are even more antipsychotics that are contraindicated for PD.
Let a medical provider know you have Parkinson’s when seeking emergency care or treatment for something by doctors who are not a part of your regular medical team.
There is only one drug, pimavanserin, approved in 2016 by the FDA specifically for PD. It has a mechanism of action that doesn’t block dopamine. This has made it a safer drug for people with Parkinson’s.2
Two other medications, quetiapine and clozapine, that have been used for a longer time, are also considered safe for treating hallucinations and delusions in people with PD.2
Recommended Reading: What Is Treatment For Parkinson’s Disease
How To Talk To Someone With Hallucinations Or Delusions
- It is usually not helpful to argue with someone who is experiencing a hallucination or delusion. Avoid trying to reason. Keep calm and be reassuring.
- You can say you do not see what your loved one is seeing, but some people find it more calming to acknowledge what the person is seeing to reduce stress. For example, if the person sees a cat in the room, it may be best to say, “I will take the cat out” rather than argue that there is no cat.
Page reviewed by Dr. Chauncey Spears, Movement Disorders Fellow at the University of Florida, a Parkinsons Foundation Center of Excellence.
Examples Of Delusions In Pd
- Jealousy
- Belief: Your partner is being unfaithful.
- Behavior: Paranoia, agitation, suspiciousness, aggression.
Also Check: Parkinson’s Disease And Driving
Talk About Your Hallucinations And Delusions
Your hallucinations or delusions can be distressing for those around you. They may be unsure how to react so let them know what you are going through and how best they can help you. They will be more able to support you if you share your experiences with them, particularly if you know what the most common triggers are and what can be done to make the hallucinations or delusions go away.
Counselling can sometimes be helpful, particularly if the hallucinations or delusions strain relationships. Your doctor will be able to advise on the available types of counselling.
Or Parkinsons Itself May Lead To Psychosis
In other cases, the disease’s progression, rather than its treatments, is likely at the root of psychosis, says Ling Pan, M.D., clinical assistant professor of neurology and neurosurgery at NYU Langone Health in New York City. Psychosis can be symptom of Parkinsons itself, so patients, for example, who have not been on medications you track the natural course of their disease may develop psychosis as part of the disease pathology. However, it appears PD medications do increase the risk, she adds.
Also Check: Parkinson’s Disease And Weight Loss
Bringing Light To Darker Side Of Parkinsons
Often the hardest part of Parkinsons disease psychosis is the fear of the unknown. As a person with Parkinsons, you may worry about having hallucinations and/or delusions and not being able to do anything about it. As a care partner, you may worry that you wont be able to help your person with Parkinsons feel safe if something does happen.
The good news is you now have information on what Parkinsons disease psychosis is the risk factors to look out for biological and environmental triggers that can bring them on and how to manage them if they show up.
But what about the emotional toll these types of symptoms can place on you over the long-term as the person with Parkinsons or as a care partner?
The diagnosis of a chronic illness in and of itself requires a lot of adjustments. When you add something like Parkinsons disease psychosis into the mix, its important that you also add another level of self-care to your everyday life.
Treatment Not A Must Early On
Typically, people with PD who develop psychosis dont do so until five to 10 years into their disease course, Dr. Hui says. For some, particularly early on, mild psychosis symptoms may be manageable without treatment. If the hallucinations are very mild and fleeting, we may not treat it if the patient is aware it is not real and can pretty much ignore them, she explains. We start treating when hallucinations become more severe or scary, like seeing attackers, or thinking someone is breaking in, and it interferes with activities of daily living or is emotionally distressing.
Also Check: Golf Therapy For Parkinson’s
The Bottom Line On Pd Psychosis
While it can be tricky to balance treating your motor symptoms of Parkinsons disease with treating symptoms like psychosis, working closely with your health care team can help you find the right combination of medications and lifestyle management skills for you. And remember: As with many aspects of this disease, early intervention is best. Psychosis in Parkinsons disease is something that, as providers and family members, important to screen for early on so we can monitor it, says Dr. Pan.
-
Parkinsons Information: National Institute of Health. Parkinsons Disease.
-
Psychosis in Parkinsons Information: The Michael J. Fox Foundation for Parkinsons Research. Ask the MD: Parkinsons Disease Psychosis.
-
Hallucinations and Delusions in Parkinsons: Parkinsons Foundation. Hallucinations/Delusions.
-
2017 Psychosis in Parkinsons Study:Parkinsons Disease. Management of Psychosis in Parkinsons Disease: Emphasizing Clinical Subtypes and Pathophysiological Mechanisms of the Condition.