Parkinsons Management: How To Manage And Reduce Stress
Continued stress is not good for any of us, but as you probably know, stress can severely affect Parkinsons Disease sufferers. Evidence has suggested that stress can in fact make symptoms more prominent, leaving suffers at a loss. Although it is yet to be proven, those sufferers who do experience high levels of stress can find themselves trying to deal with everyday life, the event thats caused them undue stress, and of course come to terms with the effects of their Parkinsons all at once.
With that in mind, weve put together some tips to help those with Parkinsons Disease deal with stress.
When Should I See My Healthcare Provider Or When Should I Seek Care
You should see your healthcare provider as recommended, or if you notice changes in your symptoms or the effectiveness of your medication. Adjustments to medications and dosages can make a huge difference in how Parkinsons affects your life.
When should I go to ER?
Your healthcare provider can give you guidance and information on signs or symptoms that mean you should go to the hospital or seek medical care. In general, you should seek care if you fall, especially when you lose consciousness or might have an injury to your head, neck, chest, back or abdomen.
What Are The Implications
According to this research, levodopa is unlikely to affect the progression of Parkinsons disease in the first year and a half following diagnosis.
Symptoms had improved to the same extent by 80 weeks and side effects were similar, suggesting people can start treatment as early as they need to for symptomatic relief.
This supports current practice in giving levodopa when clinically needed. There is no cure for Parkinsons disease, and further research is in progress to develop disease-modifying agents.
Also Check: When To Start Medication For Parkinson’s
Can Parkinson’s Disease Be Cured
No, Parkinson’s disease is not curable. However, it is treatable, and many treatments are highly effective. It might also be possible to delay the progress and more severe symptoms of the disease.
A note from Cleveland Clinic
Parkinson’s disease is a very common condition, and it is more likely to happen to people as they get older. While Parkinson’s isn’t curable, there are many different ways to treat this condition. They include several different classes of medications, surgery to implant brain-stimulation devices and more. Thanks to advances in treatment and care, many can live for years or even decades with this condition and can adapt to or receive treatment for the effects and symptoms.
What Causes The Condition

Although there are several recognized risk factors for Parkinsons disease, such as exposure to pesticides, for now, the only confirmed causes of Parkinsons disease are genetic. When Parkinsons disease isnt genetic, experts classify it as idiopathic . That means they dont know exactly why it happens.
Many conditions look like Parkinson’s disease but are instead parkinsonism from a specific cause like some psychiatric medications.
Familial Parkinsons disease
Parkinsons disease can have a familial cause, which means you can inherit it from one or both of your parents. However, this only makes up about 10% of all cases.
Experts have linked at least seven different genes to Parkinson’s disease. They’ve linked three of those to early-onset of the condition . Some genetic mutations also cause unique, distinguishing features.
Idiopathic Parkinsons disease
Experts believe idiopathic Parkinsons disease happens because of problems with how your body uses a protein called -synuclein . Proteins are chemical molecules that have a very specific shape. When some proteins dont have the correct shape a problem known as protein misfolding your body cant use them and can’t break them down.
With nowhere to go, the proteins build up in various places or in certain cells . The buildup of these Lewy bodies causes toxic effects and cell damage.
Induced Parkinsonism
The possible causes are:
You May Like: Last Stages Of Parkinson’s Disease
Protocol Considerations For Emg
-
Real-world walking. Investigating gait during real-world activity is desirable to understand motor strategies in a natural environment although current technological limitations make long term recordings challenging.
-
Sample size. Greater numbers of participants and more stride cycles are necessary.
-
Muscle selection. Muscles representing all major muscle groups acting on the ankle, knee and hip joints in the sagittal and coronal planes should ideally be recorded to permit analyses of multi-muscle activation patterns and underlying neural control systems to be undertaken.
-
Electrode placement. A clear statement must be included regarding methods used to identify electrode placement and established guidelines followed.
-
Longitudinal studies. This will inform us how motor patterns change with age and disease progression and help establish EMG characteristics as biomarkers.
-
Additional gait and cortical parameters. Parameters such as joint kinematics and kinetics as well as cortical activity measured with mobile, wireless systems such as functional near infrared spectroscopy or electroencephalography will enable us to relate EMG to gait impairment and cortical processes.
Physical And Mental Changes To Expect
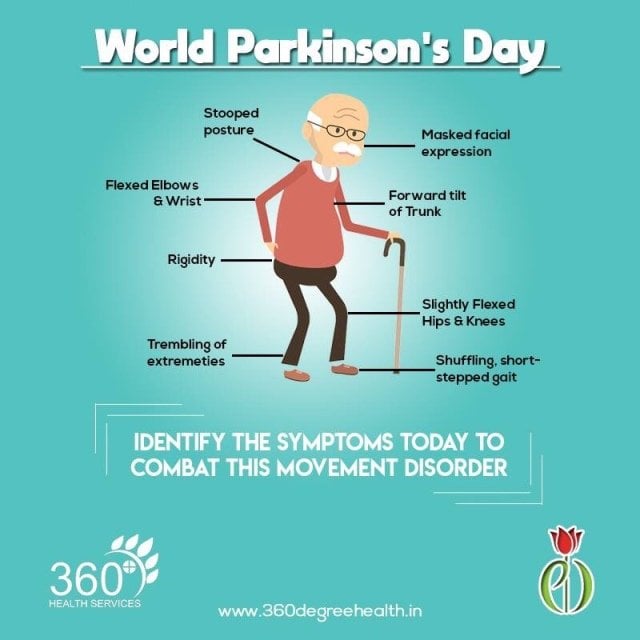
- Physical changes may include: Tremor slowness of movement stiffness of the arms, legs or trunk balance problems freezing of gait small, cramped handwriting reduced arm swing loss of facial expression softness of voice tendency to fall backwards walking with a series of quick, small steps constipation erectile dysfunction bladder control problems drooling sleep problems loss of sense of smell vision changes and restless leg syndrome.
- Mental changes may include: Difficulty with attention, focus, planning, multitasking visual spatial functions apathy or lack of motivation hallucinations and/or delusions impulsive behavior problems with memory.
- Emotional changes may include: Anxiety and depression.
The four main symptoms of Parkinsons are:
- Tremor, which means shaking or trembling. Tremor may affect your hands, arms, or legs.
- Stiff muscles.
- Slow movement.
- Problems with balance or walking.
Tremor may be the first symptom you notice. Its one of the most common signs of the disease, although not everyone has it.
More importantly, not everyone with a tremor has Parkinsons disease.
Tremor often starts in just one arm or leg or on only one side of the body. It may be worse when you are awake but not moving the affected arm or leg. It may get better when you move the limb or you are asleep.
In time, Parkinsons affects muscles all through your body, so it can lead to problems like trouble swallowing or constipation.
Recommended Reading: Shaking Disease Not Parkinson’s
Eat Plenty Of Protein But Not With Levodopa Medications
If youre taking a levodopa medication, your doctor may tell you to avoid protein when taking your meds. Both animal and plant protein can interfere with the absorption of levodopa medications.
But you should still eat plenty of protein. Just be strategic with the timing. Dont take levodopa medications with meals, Dr. Gostkowski says. Its best to take it on an empty stomach either 30 minutes before your meal or an hour after eating.
If you get nauseous from the medication, eat a small amount of starchy food with it, such as crackers. Make sure whatever you eat with your medicine doesnt have protein. Its a misunderstanding that people with Parkinsons should avoid protein, Dr. Gostkowski says. You definitely need protein in your diet. Just dont eat it when youre taking your levodopa medication.
Sidebar: Advances In Circuitry Research
The brain contains numerous connections among neurons known as neural circuits.
Research on such connections and networks within the brain have advanced rapidly in the past few years. A wide spectrum of tools and techniques can now map connections between neural circuits. Using animal models, scientists have shown how circuits in the brain can be turned on and off. For example, researchers can see correlations between the firing patterns of neurons in a zebrafishs brain and precise behavioral responses such as seeking and capturing food.
Potential opportunities to influence the brains circuitry are starting to emerge. Optogenetics is an experimental technique that involves the delivery of light-sensitive proteins to specific populations of brain cells. Once in place, these light-sensitive proteins can be inhibited or stimulated by exposure to light delivered via fiber optics. Optogenetics has never been used in people, however the success of the approach in animal models demonstrates a proof of principal: A neural network can be precisely targeted.
Thanks in part to the BRAIN Initiative, research on neural circuitry is gaining momentum. The Brain Research through Advancing Innovative Neurotechnologies Initiative is accelerating the development and application of new technologies that enable researchers to produce dynamic pictures of the brain that show how individual brain cells and complex neural circuits interact at the speed of thought.
NIH Publication No. 15-5595
Recommended Reading: Does Nick Nolte Have Parkinson’s Disease
Challenges You As A Caregiver Are Likely To Face
There are challenges that a person with Parkinsons disease confronts. First, the disease can vary from day to day. There will be times when they can function almost normally and then other times when they will be very dependent. This is a natural part of the disease. But it can make a caregiver feel that the person is being unnecessarily demanding or manipulative. Keep in mind that Parkinsons is unpredictable and each day can pose new challenges for you and your loved one.
Also, keep in mind that Parkinsons is a progressive disorder. While medications and surgery can provide significant relief of symptoms, they do not stop the progression of the disease.
Depression is also very much a part of the disease. It is important to recognize the signs and symptoms of depression so you can help your loved one seek treatment promptly. And, if you are feeling depressed and having trouble coping, its just as important to get care for yourself.
The Best News Of The Year Is That Anyone Can Take Them
From: Robert Rodgers, Ph.D.
As a seasoned researcher, I wanted to take on a research project that was the challenge of all challenges, a project that no one else thought could lead to useful findings. After dabbling with one project idea after another, researching how Parkinsons Disease can be healed from the inside out has become my passion.
PAPERBACK: CLICK ON THE BOOK BELOW TO ORDER
Five Steps to Recovery
Parkinsons Disease has profoundly affected my family. My mother had Parkinsons. My uncle had Parkinsons. I accepted their fate at the time, a fate that doctors said would inevitably lead to perpetual decline and illness.
Everyone said the same thing: Parkinsons Disease is a degenerative disease. You dont get better. One day I woke up and the insight flashed: It is not true. People can heal from Parkinsons. The body does know how to heal itself.
I launched an aggressive research program to identify the therapies, modalities and approaches that are helping people with the symptoms of Parkinsons. I stumbled on people who are symptom free today after experiencing symptoms that were debilitating.
My research has revealed person after person is taking positive action on one suggestion or another. As a result more and more people with Parkinsons are feeling better. These are exciting times to be alive.
You May Like: Lifespan For Parkinson’s Disease
Impulsive And Compulsive Behaviour
Some patients who take dopamine agonists can experience problems controlling impulsive or compulsive behaviour .
Impulsive behaviour refers to the inability of patients to resist carrying out certain activities, some of these activities could be harmful to themselves or others. In many cases, this behaviour is out of character.
Compulsive behaviour refers to an overwhelming urge to act in a certain way to reduce the worry or tension this urge produces. This behaviour can be expressed in a number of ways, including addictive gambling, impulsive shopping, binge eating and hypersexuality.
Nurses who suspect a patient might be experiencing compulsive or impulsive behaviour should discuss the issue with the patient and the patients neurologist or GP as soon as possible.
How To Start Exercising If Youre Living With Parkinsons
Safety is key. The first thing you need to do is talk with your neurologist and primary care doctor to make sure that the exercise regimen that you embark upon is safe for you.
Next, ask for a referral for physical therapy. A physical therapist will be able to figure out what movement challenges you may have and design a program to help you improve. There are certain physical therapists with additional training in Parkinsons. Your physical therapist will work with you for your allotted sessions, and then can help you plan your ongoing exercise regimen that is tailored to you. You can contact the APDA National Rehabilitation Resource Center for Parkinsons Disease for help finding resources in your area.
Additionally, physical therapy can help counteract the tendency for people with PD to reduce the size of their movements. The Lee Silverman Voice Technique has designed a program called LSVT-BIG which trains participants to make big movements. You can search for an LSVT-trained professional near you.
Anyone starting out on an exercise program could benefit from APDAs Be Active & Beyond exercise guide which includes clear photos with simple instructions that are easy to follow, with exercises that address all levels of fitness.
Recommended Reading: Does Parkinson’s Get Worse
Be Proactive About Improving Your Quality Of Life
The most important step you can take is to seek help right from the beginning. Education and support will help you deal with any challenges ahead. Taking action early will help you understand and deal with the many effects of the disease. A counselor or mental health care provider can design a treatment plan to meet your specific needs. The goal is to help you regain a sense of control over your life and improve your quality of life.
Other steps you can take include the following.
- Find out as much as you can about the condition.
- Talk to your friends and family about it. Don’t isolate them. They will want to be involved in helping you.
- Do things you enjoy.
- Donât be afraid to ask your doctor, nurse, or other health care provider to repeat any instructions or medical terms that you don’t understand or remember. They should always be available to answer your questions and address your concerns.
- Make use of resources and support services offered by your hospital and in your community.
- Learn to manage stress. This will help you to maintain a positive physical, emotional, and spiritual outlook. Being stressed out will only make the situation worse. You should try to organize a daily routine that will reduce stress, with down time for both you and your family members.
- If you are depressed — and this is more than just feeling sad occasionally — antidepressants can be prescribed to help lift your mood.
When Should I Talk To My Healthcare Provider
Talk to your healthcare providers about your mood at every appointment. Talking about it regularly will prompt you to open up. And it will help your healthcare providers notice symptoms of depression early so they can provide care.
If you start to think about hurting yourself, call a healthcare provider immediately. You can also call the National Suicide Prevention Lifeline at 800.273.8255. This hotline connects you to a national network of local crisis centers for free and confidential emotional support. The centers support people in suicidal crisis or emotional distress 24 hours a day, 7 days a week.
In an emergency, call 911.
A note from Cleveland ClinicDepression from Parkinsons disease isnt a sign of weakness or something you have to live with. Its related to chemical changes in your brain, and treatments can help. Talk to your healthcare provider about your mood, especially if you feel down for weeks at a time. Several strategies can help you feel better. You can still take part in things you enjoy and better manage the symptoms of Parkinsons disease.
Last reviewed by a Cleveland Clinic medical professional on 12/20/2020.
References
Also Check: Does Parkinson’s Cause Insomnia
What Tests Will Be Done To Diagnose This Condition
When healthcare providers suspect Parkinsons disease or need to rule out other conditions, various imaging and diagnostic tests are possible. These include:
- Blood tests .
- Positron emission tomography scan.
New lab tests are possible
Researchers have found possible ways to test for possible indicators or Parkinsons disease. Both of these new tests involve the alpha-synuclein protein but test for it in new, unusual ways. While these tests cant tell you what conditions you have because of misfolded alpha-synuclein proteins, that information can still help your provider make a diagnosis.
The two tests use the following methods.
- Spinal tap. One of these tests looks for misfolded alpha-synuclein proteins in cerebrospinal fluid, which is the fluid that surrounds your brain and spinal cord. This test involves a spinal tap , where a healthcare provider inserts a needle into your spinal canal to collect some cerebrospinal fluid for testing.
- Skin biopsy. Another possible test involves a biopsy of surface nerve tissue. A biopsy includes collecting a small sample of your skin, including the nerves in the skin. The samples come from a spot on your back and two spots on your leg. Analyzing the samples can help determine if your alpha-synuclein has a certain kind of malfunction that could increase the risk of developing Parkinsons disease.
Living Well With Parkinson’s
While medication and DBS surgery are the most effective treatments for PD, individuals often choose to delay these treatments because of their adverse side effects. Until a therapy is developed that can halt the progression of PD, there is a significant need for strategies that provide symptom relief without causing negative side effects.
Diet, Exercise, and Stress Reduction
Findings from several studies suggest that exercise has the potential to provide relief from certain PD symptoms. Anecdotally, people with Parkinsons disease who exercise typically do better. However, many questions remain. Among them is whether exercise provides a conditioning effect by strengthening muscles and improving flexibility or whether it has a direct effect on the brain.
In an NINDS-funded trial comparing the benefits of tai chi, resistance training, and stretching, tai chi was found to reduce balance impairments in people with mild-to-moderate PD. People in the tai chi group also experienced significantly fewer falls and greater improvements in their functional capacity.
Technologies that Improve Quality of Life
Don’t Miss: Parkinson’s And Eye Twitching