What Challenges Can People With Parkinsons Experience Later In Life
As Parkinsons disease is a progressive condition with variable motor and non-motor symptoms, patients may face considerable problems in late stages. Impairment of functions that are difficult to manage may bring limitations in daily activities and increase dependence.
The problems in later stages of Parkinsons disease include worsening walking disorders, with postural impairment and falls speech and swallowing disorders and progressive functional disability in the hands. They can also include non-motor issues, which may have a negative impact on quality of life including fatigue and sleep problems with restless legs or REM sleep disorder, bladder problems and constipation, drooling and orthostatic episodes, mood and behavioural disorders, hallucinations and cognitive impairment.
Does Parkinsons Affect Your Lifespan
Parkinsons research and treatments have come a long way, so much so that the average life span of a person with Parkinsons is the same or near the same as someone without Parkinsons disease. However, the lifespan of a person can vary widely based upon that persons health choices, such as their diet, exercise routine, if they have a history of smoking and many other factors. So, for most people with Parkinsons, as long as you focus on managing your Parkinsons disease and make healthy choices your lifespan should not be shortened.
Theory Of Pd Progression: Braaks Hypothesis
The current theory is that the earliest signs of Parkinsons are found in the enteric nervous system, the medulla and the olfactory bulb, which controls sense of smell. Under this theory, Parkinsons only progresses to the substantia nigra and cortex over time.
This theory is increasingly borne out by evidence that non-motor symptoms, such as a loss of sense of smell , sleep disorders and constipation may precede the motor features of the disease by several years. For this reason, researchers are increasingly focused on these non-motor symptoms to detect PD as early as possible and to look for ways to stop its progression.
Page reviewed by Dr. Ryan Barmore, Movement Disorders Fellow at the University of Florida, a Parkinsons Foundation Center of Excellence.
Don’t Miss: Stage 1 Parkinson’s Treatment
Myth : Aside From Medication There Isnt Much You Can Do
Fact: This it is what it is theres nothing I can do to help myself myth is counterproductive. There is a lot you can do chiefly, keeping as active as you can. A recent study found that patients with Parkinsons who took part in weekly, hourlong exercise sessions were able to do more in their daily lives than those who did not.
What Makes Pd Hard To Predict
Parkinsonâs comes with two main buckets of possible symptoms. One affects your ability to move and leads to motor issues like tremors and rigid muscles. The other bucket has non-motor symptoms, like pain, loss of smell, and dementia.
You may not get all the symptoms. And you canât predict how bad theyâll be, or how fast theyâll get worse. One person may have slight tremors but severe dementia. Another might have major tremors but no issues with thinking or memory. And someone else may have severe symptoms all around.
On top of that, the drugs that treat Parkinsonâs work better for some people than others. All that adds up to a disease thatâs very hard to predict.
Don’t Miss: Diagnostics For Parkinson’s Disease
What Are The Early Warning Signs Of Parkinson’s Disease
Parkinsons warning signs can be motor symptoms like slow movements, tremors or stiffness. However, they can also be non-motor symptoms. Many of the possible non-motor symptoms can appear years or even decades ahead of motor symptoms. However, non-motor symptoms can also be vague, making it difficult to connect them to Parkinson’s disease.
Non-motor symptoms that might be early warning signs include:
- Sleep problems such as periodic limb movement disorder , rapid eye movement behavior disorder and restless legs syndrome.
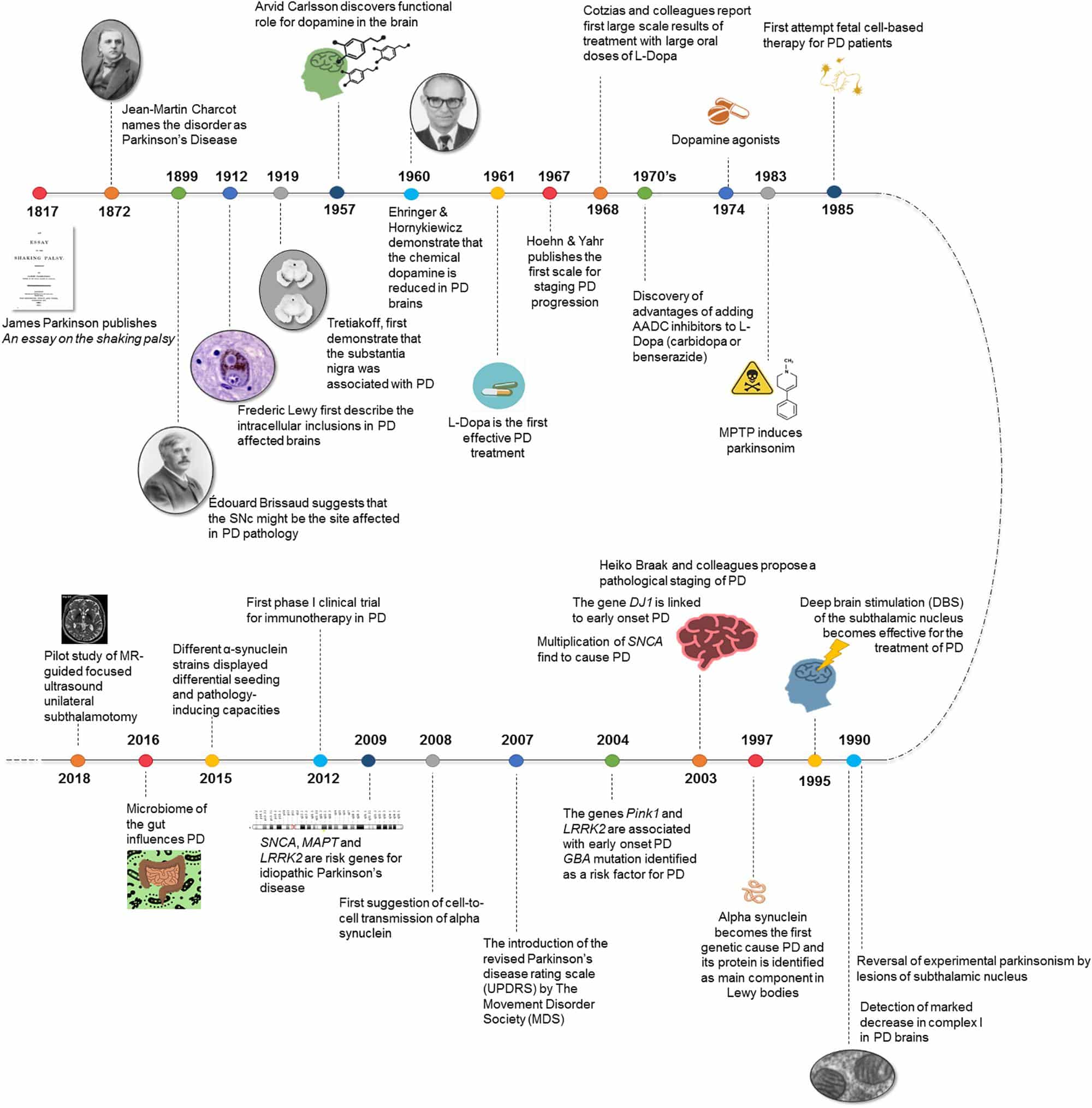
Myth : Parkinsons Research Is Stalled
Fact: It may feel as though theres nothing dramatic going on in the Parkinsons disease field, but there are several recent and very exciting breakthroughs regarding our understanding of the underlying pathology and disease mechanism. This will translate into actual clinical results in the next few years.
Read Also: What Does Parkinson’s Feel Like
Management Of Psychological Care
At the end stage of Parkinsons a high incidence of cognitive impairment and dementia is found to occur in up to 60% of people with Parkinsons after 12 years .
Wandering, sundowning, agitation and combativeness are all behavioural symptoms of dementia and can be difficult for families to manage in the community.
Early referral to the psychiatric team is important for management of the symptoms. Education of carers in behavioural management, with support from social services in delivery of care in the home, is also important.
Medications which may be used to treat dementia in Parkinsons are cholinesterase inhibitors such as rivastigmine and donepezil.
Psychosis can affect people with Parkinsons whether or not they have cognitive impairment. Visual hallucinations and delusions are the most common psychotic symptoms in Parkinsons and are quite often related to side effects of medication, so frequent reassessment of medication is important in the end stage. First rule out intercurrent medical conditions, such as constipation, dehydration or infection, which may be hidden causes of psychosis.
Agitation and delirium at end of life
At least 80% of dying people experience delirium to some degree, and this may give rise to agitation and restlessness. It is important to involve the specialist palliative care team who have the expertise to manage the delirium and support the family and/or carers .
What Are The Symptoms
The best-known symptoms of Parkinson’s disease involve loss of muscle control. However, experts now know that muscle control-related issues aren’t the only possible symptoms of Parkinson’s disease.
Motor-related symptoms
Motor symptoms which means movement-related symptoms of Parkinsons disease include the following:
Additional motor symptoms can include:
- Blinking less often than usual. This is also a symptom of reduced control of facial muscles.
- Cramped or small handwriting. Known as micrographia, this happens because of muscle control problems.
- Drooling. Another symptom that happens because of loss of facial muscle control.
- Mask-like facial expression. Known as hypomimia, this means facial expressions change very little or not at all.
- Trouble swallowing . This happens with reduced throat muscle control. It increases the risk of problems like pneumonia or choking.
- Unusually soft speaking voice . This happens because of reduced muscle control in the throat and chest.
Non-motor symptoms
Several symptoms are possible that aren’t connected to movement and muscle control. In years past, experts believed non-motor symptoms were risk factors for this disease when seen before motor symptoms. However, theres a growing amount of evidence that these symptoms can appear in the earliest stages of the disease. That means these symptoms might be warning signs that start years or even decades before motor symptoms.
Non-motor symptoms include:
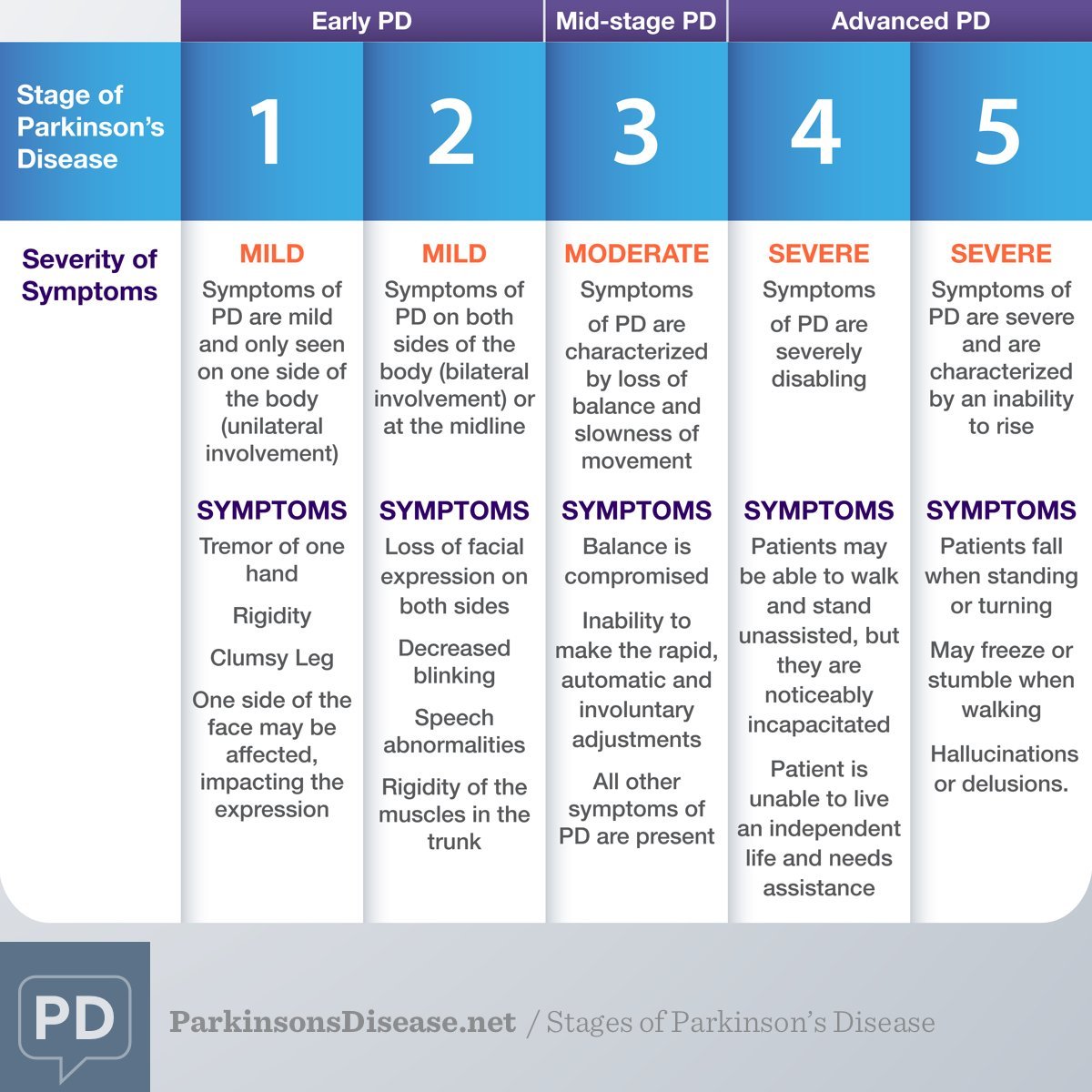
Stages of Parkinsons disease
Don’t Miss: Treating Parkinson’s Disease In Dogs
What Are The Important Points Regarding Apomorphine At The End Of Life
Apomorphine is a dopamine agonist, which is given as a subcutaneous infusion either continuously or intermittently and also as single subcutaneous injections. An overview of studies into apomorphine use shows improvement in motor off periods and in dyskinesias.39
Apomorphine has side-effects similar to other dopaminergic medication but also notably nausea and vomiting. Ondansetron is not recommended for nausea in patients using apomorphine due to adverse effects.21
Subcutaneous apomorphine has been used at the end of life in a patient with advanced PD although with the recommendation that this is by a healthcare professional experienced in its use.40
What Is The Definition Of Palliative Care
The word palliative derives from the Latin pallium, meaning cloak or covering. It is reflected in the Middle Eastern blessing: May you be wrapped in tenderness, you my brother, as if in a cloak.
We could use the word cloak to symbolise the holistic care we aim for, which encompasses the physical, psychological, social and spiritual aspects of care, and is highlighted in the following definition of palliative care:
Palliative care is an approach that improves the quality of life of patients and their families who are facing problems associated with life-threatening illness. It prevents and relieves suffering through the early identification, correct assessment and treatment of pain and other problems, whether physical, psychosocial or spiritual.
The early development of the palliative care ethos was synonymous with cancer care, but as research in palliative care developed it became recognised that people living with life limiting, non-malignant illness had as many complex care needs as those suffering with cancer. The recognised definition of palliative care devised by the World Health Organization was therefore revised to incorporate the care of those with life limiting illnesses.
Further reading
The trajectory of Parkinsons is variable and complex, making it essential that each person is assessed regularly by the multidisciplinary team and their changing needs are managed on an individual basis.
2.2.1 Dynamic model of palliative care services
Recommended Reading: Parkinson’s And Sense Of Smell
What Causes Parkinson Disease
Parkinson disease arises from decreased dopamine production in the brain. The absence of dopamine makes it hard for the brain to coordinate muscle movements. Low dopamine also contributes to mood and cognitive problems later in the course of the disease. Experts don’t know what triggers the development of Parkinson disease most of the time. Early onset Parkinson disease is often inherited and is the result of certain gene defects.
How Can I Support Someone With Parkinsons At The Advanced Or Palliative Stage
In the advanced stages of Parkinsons, your patients care needs may be more complex and require careful planning along with the patient, their family and other health and social care professionals involved.
Palliative care should be holistic, considering the whole person to support the personal, social, psychological and spiritual needs of your patient and their family. It should give your patient some control and choice over areas such as treatment options and where they will be cared for, as well as providing advice and support to all the people involved in their care.
Palliative care in Parkinsons may be supported by a number of professionals, including a Parkinsons nurse specialist, local hospice or specialist palliative care team, physiotherapist, occupational therapist, speech and language therapist or dietitian. Many people with Parkinsons also find complementary therapies beneficial.
It is important that you find out whether the person has a care plan in place regarding their preferences for how the issues surrounding advanced Parkinsons should be managed. This could include legal documentation such as a Lasting Power of Attorney and an advance care plan. Advance care plans include information on what the persons wishes and preferences are for their care in the future. They may include decisions on any treatments the person doesnt want to have in the future this is called an Advance Directive, Advance Decision to Refuse Treatment or Living Will.
Don’t Miss: Parkinson’s Disease Occurs When
What Is Parkinson’s
Parkinson’s is a progressive neurological condition. This means that it causes problems in the brain and gets worse over time. The problems in the brain can cause different signs and symptoms, including slowness of movement, stiffness and tremor.
Parkinsons is sometimes called idiopathic Parkinsons disease. Idiopathic means the cause is unknown.
Parkinsons happens when there is a loss of nerve cells in the brain that make the chemical dopamine. Dopamine plays a central role in regulating the movement of the body.
About one person in every 500 has idiopathic Parkinsons. Thats about 145,000 people in the UK. Most people who get Parkinsons are aged 50 or over, but younger people can get it too.
Parkinsonism is a term used to describe a group of symptoms or signs that cause slowness of movement, stiffness and tremor. This includes Parkinsons but also conditions such as multiple system atrophy , progressive supranuclear palsy or corticobasal degeneration. Sometimes the side effects of certain medicines can cause Parkinsonism, for example metoclopramide and haloperidol.
What You Can Expect
Parkinson does follow a broad pattern. While it moves at different paces for different people, changes tend to come on slowly. Symptoms usually get worse over time, and new ones probably will pop up along the way.
Parkinsonâs doesnât always affect how long you live. But it can change your quality of life in a major way. After about 10 years, most people will have at least one major issue, like dementia or a physical disability.
Don’t Miss: Neck Brace For Parkinson’s
Death Rate From Parkinsons Disease Rising In The Us
Over the last two decades, the death rate from Parkinson’s disease has risen about 63% in the US, according to research published in Neurology, the medical journal of the American Academy of Neurology. The study also reported that the death rate was twice as high in men as in women, and there was a higher death rate in white people than other racial/ethnic groups.
“We know that people are living longer and the general population is getting older, but that doesn’t fully explain the increase we saw in the death rate in people with Parkinson’s,” study author Wei Bao, MD, PhD, who conducted the research at the University of Iowa in Iowa City. “Understanding why more people are dying from this disease is critical if we are going to reverse the trend.”
The study looked at a national death registry that included 479,059 people who died of Parkinson’s between 1999 and 2019.
After adjusting for age, researchers found that the number of people who died from the disease increased from 5.4 per 100,000 people in 1999 to 8.8 per 100,000 people in 2019. The average annual increase was 2.4%.
It’s important to continue to evaluate long-term trends in Parkinson’s death rates, said Dr. Bao. This can inform future research that may help pinpoint why more people are dying of the disease. Also, updating vital statistics about Parkinson’s death rates may be used for priority setting and financing of health care and policy.”
-
INSIGHTEC, a medical technology innovator of incisionless…
How Is Parkinson Disease Diagnosed
Parkinson disease can be hard to diagnose. No single test can identify it. Parkinson can be easily mistaken for another health condition. A healthcare provider will usually take a medical history, including a family history to find out if anyone else in your family has Parkinson’s disease. He or she will also do a neurological exam. Sometimes, an MRI or CT scan, or some other imaging scan of the brain can identify other problems or rule out other diseases.
Read Also: Serotonin Syndrome And Parkinson’s
Large Study Finds Parkinson Disease Us Death Rate Soared 63% Over 20 Years
The authors said long-term trends in Parkinson disease were previously unknown and that the findings are important to determining national health care priorities.
The death rate from Parkinson disease has risen about 63% in the United States over the past 2 decades, according to a study released Thursday.
Although the increase was regardless of age, sex, race/ethnicity, urban-rural classification, and geographic location, some groups were affected more than othersnamely men and White individuals. In addition, city residents had higher death rates than rural ones.
The authors, writing in Neurology, said it is the most comprehensive study to date on the issue, that long-term trends were previously unknown, and that the findings are key to determining health care priorities, including financing and research.
In the United States, about 1 million individuals have PD, and nearly 60,000 new cases are diagnosed each year.
The investigators used data on 479,059 deaths due to PD from 1999 to 2019 from the National Vital Statistics System , a nationwide, population-based death registry. More than 99% of US deaths are recorded in the database, which is part of the CDCs National Center for Health Statistics.
After adjusting for age, the researchers found that the number of people who died from the disease increased from 5.4 per 100,000 people in 1999 to 8.8 per 100,000 people in 2019. The average annual increase was 2.4%.
Reference
Dry Eyes Are A Commonly Reported Symptom Of Pd
Vision changes can be caused by a number of factors. Reasons behind dry eyes or blurry vision can include “hormone changes, autoimmune disease, inflamed eyelid glands or allergic eye disease,” says the Mayo Clinic. Other times, your eyes are sending a warning signal about a more serious condition. Vision changes can be a symptom of eye cancer, early-onset dementia, or PD, among other conditions.
“Dry eye disease , which occurs when the eyes are not sufficiently moistened by tears, can lead to chronically dry eyes that cause discomfort and risk vision loss, significantly disrupting daily life,” reports Parkinsons News Today, noting that a recent study found the estimated occurrance of DED in Parkinson’s patients is between 53 percent and 60 percent.
“Some people with Parkinson’s report that their vision loses sharpness as their disease progresses,” advises the Parkinson’s Foundation. “Difficulties related to the eyes and vision often progress alongside other PD symptoms.”
Dry eyes can occur because of decreased blinking, which can also result in blurry vision. Other changes in eyesight include double vision, trouble with reading, and rouble voluntarily opening the eyes, known as apraxia, the Parkinson’s Foundation explains.
If you’re experiencing dry eyes, check with your healthcare provider about whether you should be screened for PD.
Read Also: Test To See If You Have Parkinson’s Disease
Collaboration Between Specialist Palliative Care And Pd Care
Specialist palliative care has an important role in the care of people with PD, and their families. This is in addition to, and in collaboration with, a wider multidisciplinary team approach for these patients, where a specialist team, working in movement disorders and including not only neurologists and specialist nurse but other disciplines, including physiotherapy, occupational therapy, psychological support, dietitian, spiritual support, speech and language therapy and counselling/social care.
The involvement of specialist palliative care has been shown to be effective and at the end of life there are potential triggers facilitating referral. However, throughout the disease progression there may be a role for managing complex issues and for other complicated issues, such as difficult decisions or ethical dilemmas. There is a need for greater awareness of all involved in PD care for the involvement of specialist palliative care, when the more generic palliative care that they are providing is not adequate or allowing the maximization of QOL. There are now several assessment tools that may be used on a routine basis with the aim of elucidating these complex issues. These include:
These scales can help to identify patient and families with particular issues and allow monitoring after management has been started to see how effective this has been. In this way the awareness of the role and possibilities of specialist palliative care can be raised.