Early Clinical Trials Of Neural Transplantation For The Treatment Of Pd
Modern neural transplantation began as early as the 1970s. PD was the first neurodegenerative disorder to be treated using stem cell grafts because the loss of nigrostriatal dopaminergic neurons was limited in number and area and symptoms were secondary to cell loss . Successful trials of DA-rich fetal ventral mesencephalon grafts appeared in the 1980s, with improvements of Parkinsonian symptoms seen in rodents and non-human primates, which pushed clinical trials of neural transplantation in the latter part of the decade .
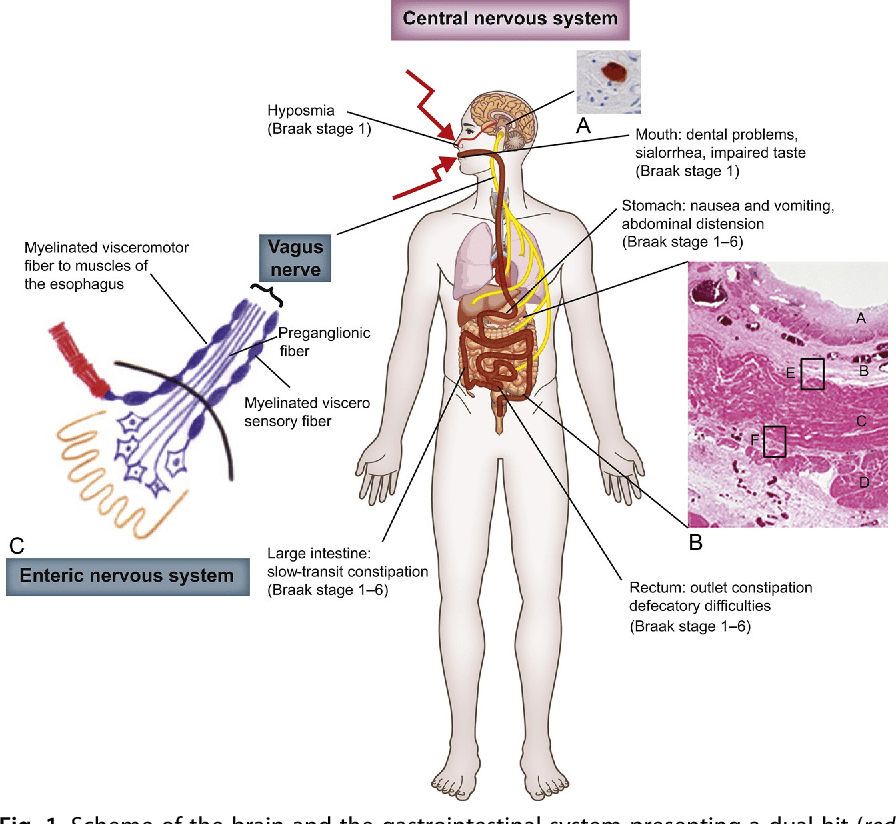
What Are The Non
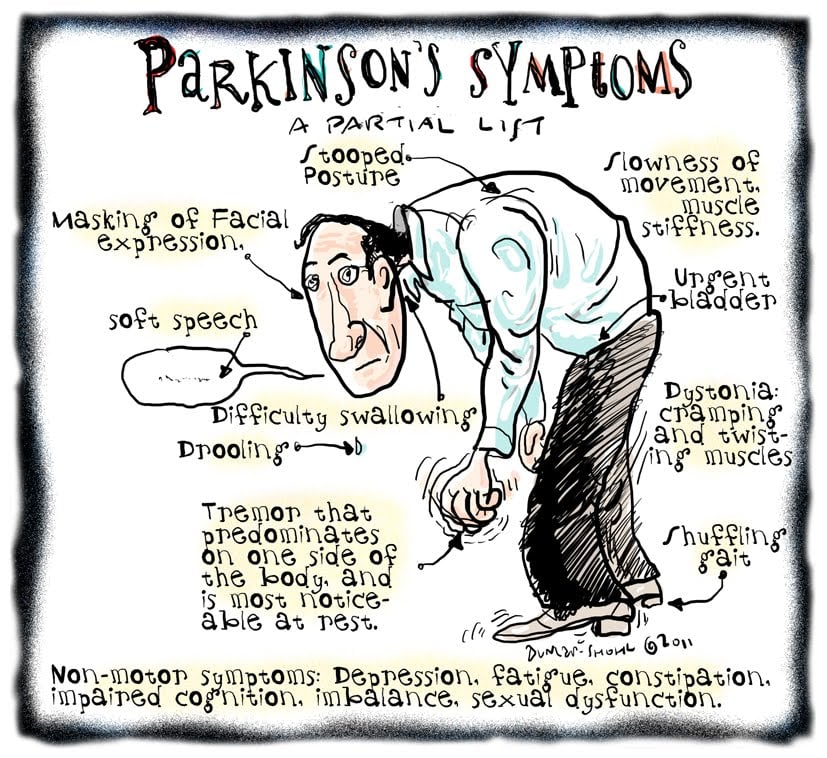
Parkinsons is officially classified as a movement disorder because it involves damage to the areas of the brain, nerves and muscles that influence the speed, quality, fluency and ease of movement. While the effects of Parkinsons on movement are often the most visible symptoms, like tremor, non-motor symptoms of Parkinsons, like emotional and cognitive challenges, can sometimes have an even greater effect on your quality of life.
The effects of Parkinsons not related to movement are called non-motor symptoms. Non-motor symptoms of Parkinsons may actually outnumber motor symptoms and can appear years before motor symptoms.
In this article, we will help you identify and learn about the various non-motor symptoms of Parkinsons so you can take the first steps to living well.
Non-motor symptoms of Parkinsons are effects not related to movement.
There is a wide variety of possible non-motor symptoms of Parkinsons, ranging from physiological effects like trouble swallowing, pain and fatigue, to mental and emotional impacts, such as mood changes, cognitive challenges and anxiety. Just as Parkinsons affects everyone differently, the type, frequency and severity of non-motor symptoms each person experiences vary. Remember, just because something is listed as a non-motor symptom of Parkinsons does not mean you will experience it.
Its a lot harder to explain the Parkinsons that people dont see. Paul
What To Expect From Diagnosis
Theres no single test for Parkinsons, so it can take some time to reach the diagnosis.
Your doctor will likely refer you to a neurologist, who will review your symptoms and perform a physical examination. Tell your doctor about all the medications you take. Some of these symptoms could be side effects of those drugs.
Your doctor will also want to check for other conditions that cause similar symptoms.
Diagnostic testing will be based on your symptoms and neurologic workup and may include:
You May Like: Do You Hallucinate With Parkinson’s
Clinical Evaluation Of Non
The following symptoms were assessed: hyposmia, neuropsychiatric disorders , autonomic dysfunctions , and sleep disturbances . A clinical interview was conducted to determine the presence of each NMS at the time of the examination. Informations on the current use of medications, such as laxatives, hypnotics, or antidepressants to treat some of these NMS, were also collected.
Smell loss was assessed by the validated Argentina Hyposmia Rating Scale starting by asking the subjects whether they noted a change in their ability to smell. Patients with factors that could impair odor identification, such as: current smokers, medical history of nasal surgery , allergic rhinitis, and traumatic nasal injuries were eliminated. According to these criteria, our sample for this test was restricted to 51 patients . Hyposmia was considered to be present if the AHRS score was lower than 22.
To evaluate the presence of depression and its severity, we used the MontgomeryAsberg Depression Rating Scale . The cut-off scores we used were: < 7 absent signs, mild signs = 718, moderate = 1834, and 35 reflects severe depression. This scale consistently has the highest Cronbachs alpha levels reaching 0.92 . Patients with severe depression were excluded from the study. Patients with scores 7 were considered having depression.
Typically Three Primary Areas Of Cognition Are Affected:
- Executive functioning: including multitasking, reasoning, problem-solving, concentration and complex planning.
- Language: including difficulty finding the right word in your mind or feeling tongue-tied.
- Memory: trouble retrieving memories that have already been encoded. This is different than Alzheimers, where memories are not able to be encoded.
In many situations, these challenges do not significantly impact daily life. For some people living with Parkinsons, these changes will never progress beyond mild cognitive impairment. Others experience a very slow cognitive decline over time.
If cognitive challenges start to have a significant impact on quality of life, such as making it difficult to drive or consistently forgetting important things like where you parked, if you paid a bill or even what you ate, mild cognitive impairment may be better described as dementia. Dementia brings up a lot of fear and can be difficult to discuss, even with your physician. However, physicians can perform objective tests to measure your thinking and memory to help identify when and cognitive impairment should be addressed. Keep in mind that the progression of dementia that can come for some people in the later stages of Parkinsons can be influenced when caught early and managed proactively.
Read Also: How Long Does Parkinson’s Take To Kill You
Other Symptoms: Aging Or Pd
Because the biggest risk factor for developing PD is age , skeletal problems associated with aging are often experienced by people with PD. While it is not clear that PD increases the risk or even the severity of these other skeletal conditions, the problems of PD can make the symptoms of these conditions more prominent.
- Osteoarthritis, the joint damage associated with general wear and tear on the joints, is nearly universal in aging. Osteoarthritis tends to affect larger joints such as the hip and knee.
- Arthritis of the spine is also very common. This may contribute to the development of spinal stenosis, narrowing of the canal in the spine that houses the spinal cord. In severe cases, spinal stenosis causes damage to the nerves as they exit the spine or even to the spinal cord itself.
- Disorders of the fibrous discs between the bones of the spine can also cause pain, or limb numbness or weakness.
How Are They Treated
There is currently no known cure for PD. However, there are treatments that can help manage the symptoms. Most treatments of the non-motor symptoms are specific to the symptom.3,4
For example, there are medicines that can reduce an overactive bladder in people who experience urinary problems. Or, pain may be relieved through a combination of medicine, physical therapy, and exercise.3,4
Some non-motor symptoms, such as constipation, sleep problems, psychotic symptoms, or impulsive behaviors, may be caused as a side effect of or worsened by drugs used to treat the motor symptoms of PD.3,4
In this case, people may be able to work with their doctors to adjust their medicine or dose. Complementary therapies, such as acupuncture or massage, may also help relieve some non-motor symptoms of PD.3,4
Also Check: Early Symptoms Of Parkinson’s Disease Include
Clinical Trials For Non
One of the major unmet needs in PD treatment is therapies for non-motor symptoms as these can have a significant effect on daily quality of life for both the person living with PD and their care partner. Therefore, it is particularly exciting to witness compounds being studied in clinical trials for these symptoms.
Many of the currently active clinical trials for non-motor symptoms involve studying medications that are already approved for other diseases or uses, in hopes of determining if the medication also works for a particular symptom in the context of PD. Although these trials are crucial, this blog will focus on clinical trials of newly developed compounds aimed to specifically treat non-motor symptoms in PD.
If you are interested in getting involved in a clinical trial, Clinicaltrials.gov is a website that you should know about. It is a database of all clinical trials for all diseases worldwide. When a clinical trial is registered with the site, it is assigned a unique number called the National Clinical Trial number. I will be referring to these numbers as I outline the clinical trials that are being conducted for newly developed compounds for non-motor symptoms of Parkinsons disease so that you can learn more about them if youre interested in participating in the trial.
What You Can Do Right Now To Live Well
An evaluation by a neuropsychologist, a specialist trained in measuring thinking and behavioral functions, can help identify cognitive difficulty or dementia. Neuropsychological testing measures thinking abilities such as concentration, attention, memory, language abilities, abstract thinking, spatial skills and executive functions and can help your physician determine what could be causing thinking problems.
Some people experience improvements in cognitive function when they take certain medications or even change their current medications. Talk with your physician about which medications might work for you.
Physical exercise has also been proven to help not just the body, but the brain. Exercise can improve cognitive function as well as reduce the long-term risk of dementia.
Our Brain Health & Memory Worksheet includes more ways to maintain cognitive functions like memory, planning and problem-solving.
Parkinsons impact on emotions and mood are often overlooked because they are complicated and harder to talk objectively about than physical symptoms. While a Parkinsons diagnosis itself can bring feelings of grief and anxiousness for the future, there are also biological changes caused by Parkinsons that can result in mood changes such as anxiety, apathy and depression.
Depression, anxiety and apathy can have a significant impact on you and your familys quality of life.
You May Like: How To Help Someone With Parkinson’s Disease
Gan Model And Training
The architecture of the GAN consisted of two neural networks: the generator and the discriminator. The discriminator had the same architecture as the CNN described earlier. This allowed us to directly compare the performance of the CNN and GAN discriminator and to isolate and understand the effects of training with and without data augmentation via a generator network. Henceforth, GAN discriminator refers to a shallow neural network trained with an adversarial generator to predict PIGD score and identify real walks from fake ones. CNN is the same shallow neural network but trained without a generator that predicts PIGD score alone.
The generator neural network accepted input noise with dimensions 400×100, sampled from the uniform distribution between 0 and 1 as in the study in ref. . The generator architecture consisted of 3 fully connected layers. The first 2 layers had 512 units, used the ReLU activation function and weight normalization. The last layer served as the output layer and consisted of 1152 units with no nonlinearity and L2 regularization. Weights were initialized using the He initializer with the uniform distribution, biases were initialized as 0s, and the weight norms as 1s. Figure summarizes the GAN generator architecture.
Fig. 3: GAN generator architecture.
Input noise sampled from the uniform distribution was fed into 3 fully connected layers, and the output of the last was reshaped to the dimensions of the input accepted by the discriminator.
Breathing Problems And Parkinsons Disease
Usually, trouble breathing is not thought of as a symptom of PD. Those with PD who complain of this will typically have testing of their heart and lung function. This is necessary since, as we continue to emphasize, a person with PD can develop medical problems unrelated to PD and needs every new symptom evaluated like someone without PD. However, often the testing does not reveal a cardiac or pulmonary abnormality. Could difficulty breathing be a symptom of PD itself?
There are a number of ways in which difficulty breathing may be a symptom of PD:
Shortness of breath can be a wearing-OFF phenomenon
Some non-motor symptoms can fluctuate with brain dopamine levels, which means that they change as a function of time from the last levodopa dose. For some people, shortness of breath can be one of the non-motor symptoms that appears when medication levels are low. However, shortness of breath can be due to anxiety which can also be a wearing-OFF phenomenon. Sometimes it is not possible to determine whether the key symptom is anxiety or shortness of breath. Treatment involves changing medication dosing and timing so that OFF time is minimized. You can view this webinar which discusses the concept of wearing OFF and potential treatments.
Abnormal breathing can be a type of dyskinesia
Restrictive lung disease
Aspiration pneumonia
Sleep apnea
Read Also: Judy Woodruff Parkinson’s Disease
Runny Nose And Parkinsons Disease
Runny nose, or rhinorrhea in medical jargon, is an annoying symptom that has been shown in a number of studies to be more common among people with PD than those without PD. The rhinorrhea of PD is not associated with a viral infection or environmental allergies, or any other common cause of runny nose.
Rhinorrhea can be an early feature of PD, sometimes present at the time of diagnosis. In fact, studies have shown that rhinorrhea is not correlated with disease duration, disease severity, or whether the PD is characterized more by tremor or gait difficulties. One study tested the smell of those with runny nose versus those without and determined that the presence of rhinorrhea did not correlate with deficits in the sense of smell.
There are no studies in the medical literature addressing how to treat the runny nose associated with PD. Ipratropium bromide is an anti-cholinergic medication that does not cross the blood-brain barrier and is available in two forms an inhaled form to treat asthma, chronic bronchitis and emphysema and a nasal spray that is used to treat allergic and non-allergic runny nose. The nasal spray may be worth a try in PD-related rhinorrhea.
Treatment Of Urinary Dysfunction
New Conclusions
A total of 1 study was evaluated for the treatment of urinary dysfunction in PD, and 1 trial not meeting inclusion criteria was excluded. See Table for recommendations.
Solifenacin for the treatment of overactive bladder was evaluated in a high-quality, negative study. Because there were some significant benefits in the active arm, there is âinsufficient evidenceâ to make a conclusion on efficacy. The practice implications for solifenacin for the treatment of overactive bladder is âpossibly usefulâ as there were some significant benefits in this trial and because of the established efficacy and license of solifenacin in this indication outside PD., No safety concerns were reported. Systematic reviews reported typical peripheral antimuscarinic AEs in patients treated with solifenacin.- Because of the data available in the geriatric population, solifenacin is considered to pose an âacceptable risk without specialized monitoring.â
Also Check: Parkinson’s Fight Club The Villages Fl
Tips For Living With Hallucinations
It is important for people with PD to talk about hallucinations with their family and care team these are manageable and can be troublesome if not treated. Discuss all possible symptoms with your doctor, no matter how minor, rare or bizarre you may think they are.
Could This Be Due To Parkinsons Disease Uncommon Non
It is common for a person with Parkinsons disease to attribute every new symptom that develops to PD. That is largely because the list of non-motor symptoms commonly associated with PD is so varied, it can seem that almost anything is a symptom of PD! But if you take a closer look, there are some symptoms that are very commonly associated with PD, others that are virtually never associated with PD, and some in between.
Lets divide up non-motor symptoms into the following categories:
Don’t Miss: Early Parkinson’s Symptoms In Young Adults
Weakening Sense Of Smell And Taste
This may be due to degeneration of the anterior olfactory nucleus and olfactory bulb, one of the first parts of the brain affected by Parkinsons. This can happen so gradually that youre not even aware of it.
Losing your sense of smell and taste can make you lose interest in food. You may miss out on important nutrients and lose weight.
How Common Is Parkinson’s Disease Psychosis
Between 20-40% of people with Parkinsons report the experience of hallucinations or delusions.
When followed as the disease progresses over the years, this number increases. The increase does not mean that the hallucinations are persistent across the majority of people with PD. However, it is important to note that these statistics sometimes include delirium, in which the symptoms are temporary due to medication that needs to be adjusted or infection that needs to be treated, and isolated minor symptoms or minor hallucinations, including illusions, where instead of seeing things that are not there , people misinterpret things that are really there.
These are the most common types of psychosis in people with PD, with different studies placing the occurrence between 25-70% of people with Parkinsons. Typically, if the person with PD only has these minor hallucinations, their doctor will not prescribe an antipsychotic medication, though more significant psychosis that requires medication may develop over time. In one study, 10% of those with minor hallucinations had their symptoms resolved within a few years, while 52% saw their symptoms remain the same and 38% saw their psychosis symptoms get worse.
We recommend that people with Parkinsons not use a single percentage to represent the prevalence of hallucinations and PDP. Parkinsons is a complex disease and as it progresses the percentages and risk of symptoms will change.
Recommended Reading: What Specialist Treats Parkinson’s Disease
Training Considerations For Deep
We used the larger subject pool recorded at Tufts University to train our deep-learning pipelines, and the Study 2 dataset to test them. While both dataset distributions were concentrated around lower PIGD scores rather than higher scores, Study 1 dataset had more evenly distributed scores. Study 2 dataset had few subject recordings with PIGD scores in the middle a disproportionate majority of visits had low score labels with only a few visits with higher scores . Moreover, skewness was smaller for Study 1 than for Study 2, indicating that the distribution of Study 1 was less asymmetric . This in particular was important for generalization. A pipeline trained with the more skewed distribution of Study 2 scores would not have performed well when tested with examples not well represented by that dataset, namely walks for subjects with high scores .