What Is The Prognosis And Life Expectancy For Parkinson’s Disease
The severity of Parkinson’s disease symptoms and signs vary greatly from person to person, and it is not possible to predict how quickly the disease will progress.
- Parkinson’s disease itself is not a fatal disease, and the average life expectancy is similar to that of people without the disease.
- Secondary complications, such as pneumonia, falling-related injuries, and choking can lead to death.
- Many treatment options can reduce some of the symptoms and prolong the quality of life.
What Causes Parkinsons Disease
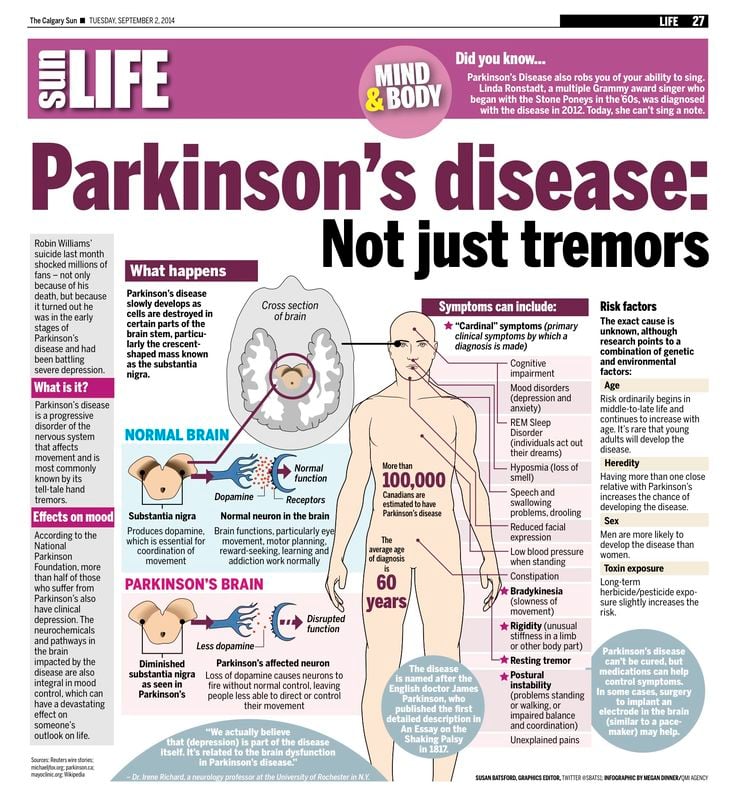
Parkinsons disease occurs when nerve cells in an area of the brain called the substantia nigra become impaired or die. These cells normally produce dopamine, a chemical that helps the cells of the brain communicate . When these nerve cells become impaired or die, they produce less dopamine. Dopamine is especially important for the operation of another area of the brain called the basal ganglia. This area of the brain is responsible for organizing the brains commands for body movement. The loss of dopamine causes the movement symptoms seen in people with Parkinsons disease.
People with Parkinsons disease also lose another neurotransmitter called norepinephrine. This chemical is needed for proper functioning of the sympathetic nervous system. This system controls some of the bodys autonomic functions such as digestion, heart rate, blood pressure and breathing. Loss of norepinephrine causes some of the non-movement-related symptoms of Parkinsons disease.
Scientists arent sure what causes the neurons that produce these neurotransmitter chemicals to die.
What Is The Outlook For Persons With Parkinsons Disease
Although there is no cure or absolute evidence of ways to prevent Parkinsons disease, scientists are working hard to learn more about the disease and find innovative ways to better manage it, prevent it from progressing and ultimately curing it.
Currently, you and your healthcare teams efforts are focused on medical management of your symptoms along with general health and lifestyle improvement recommendations . By identifying individual symptoms and adjusting the course of action based on changes in symptoms, most people with Parkinsons disease can live fulfilling lives.
The future is hopeful. Some of the research underway includes:
- Using stem cells to produce new neurons, which would produce dopamine.
- Producing a dopamine-producing enzyme that is delivered to a gene in the brain that controls movement.
- Using a naturally occurring human protein glial cell-line derived neurotrophic factor, GDNF to protect dopamine-releasing nerve cells.
Many other investigations are underway too. Much has been learned, much progress has been made and additional discoveries are likely to come.
Also Check: Cleveland Clinic Parkinson’s Bicycle Study 2017
Whats Different About Young
The age of diagnosis matters for a variety of reasons, from probable causes of early cases to symptoms and treatment:
- Genetics. As with any case of Parkinsons disease, the exact cause is usually unknown. That said, The young-onset cases of Parkinsons disease are, on average, a bit more likely to be familial or genetic, says Gregory Pontone, M.D., director of the Johns Hopkins Movement Disorders Psychiatry Clinic.
- Symptoms. In many patients with YOPD, dystonia is an early symptom. People with YOPD also report more dyskinesia . They also tend to exhibit cognitive problems, such as dementia and memory issues, less frequently.
- Progression. Patients with young-onset Parkinsons appear to have a slower progression of the disease over time, says Pontone. They tend to have a milder course, staying functional and cognitively intact for much longer.
- Treatment. Most patients with Parkinsons take the medication levodopa. However, other drugs, such as MAO-B inhibitors, anticholinergics, amantadine, and dopamine receptor agonists, may be used before levodopa.
Do People Die From Parkinsons
PD does not directly kill patients people with PD die from other causes, not from PD itself. Two major causes of death for those with PD are falls and pneumonia.
People with PD are at higher risk of falling, and serious falls that require surgery carry the risk of infection, adverse events with medication and anesthesia, heart failure, and blood clots from immobility.3
Pneumonia is a common cause of death, and those with PD are at risk for aspiration pneumonia.3 People with PD often have problems with swallowing, so the risk of aspirating food or drink, or having food or drink going down the wrong pipe is higher. In PD, the person may not be able to cough up the food or drink they aspirated, and it can remain in the lungs, eventually causing an infection.3 Even with general pneumonia, when coughing is weakened, as in PD, the mucus and other material that needs to be coughed up isnt able to be expelled, and this makes effective treatment of pneumonia more difficult in those with PD.
You May Like: On-off Phenomenon
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinsons disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didnt exercise or didnt start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinsons, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinson’s. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments whether medicines or deep brain stimulation are optimal and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
What Are The Later Secondary Signs And Symptoms Of Parkinson’s Disease
While the main symptoms of Parkinson’s disease are movement-related, progressive loss of muscle control and continued damage to the brain can lead to secondary symptoms. These secondary symptoms vary in severity, and not everyone with Parkinson’s will experience all of them, and may include:
You May Like: Sam Waterston Tremor
Circumstances And Societal Engagement In Yopd And Implications For Management
In general, people with YOPD tend to have different family and societal engagements to those with late-onset PD. For example, most people diagnosed with YOPD will have a job, whereas some people with late-onset PD have already retired. Additionaly, it is not unusual that people with YOPD have young children , or may want to start a family.
Complications Related To Parkinsons Can Affect Survival
Claudia Chaves, MD, is board-certified in cerebrovascular disease and neurology with a subspecialty certification in vascular neurology. She is an associate professor of neurology at Tufts Medical School and medical director of the Lahey Clinic Multiple Sclerosis Center in Lexington, Massachusetts.
Parkinsons is a common neurodegenerative disease, and although it is not fatal, research suggests it may influence life expectancy.
A 2012 study in Archives of Neurology examined the six-year survival of nearly 140,000 Medicare beneficiaries with Parkinsons disease in the United States. During the six-year period, 64% of the participants with Parkinsons disease passed away.
The risk of death of those with Parkinsons was then compared to Medicare beneficiaries who did not have Parkinsons or any other common diseases, including:
When controlling for variables like age, race, and gender, the six-year risk of death among people with Parkinsons was found to be nearly four times greater than those Medicare beneficiaries without the disease or other common diseases.
At the same time, the rate of death among those with Parkinsons disease was similar to those with hip fracture, Alzheimers dementia, or a recent heart attackalthough it was higher than those who had been newly diagnosed with either colorectal cancer, stroke, ischemic heart disease, or chronic obstructive pulmonary disease.
Recommended Reading: How Long Does A Person Live With Parkinsons Disease
Read Also: What Foods Should Be Avoided When Taking Levodopa
Young Onset Parkinsons Disease
Parkinsons disease normally impacts people staring in their mid-to-late 60s. Young onset Parkinsons disease refers to people diagnosed with the condition before 50.
is incredibly rare, Beck said. The numbers are hard to come by but thought to be certainly less than 5% of all diagnoses each year are people under the age of 50.
There are some differences in people with young onset Parkinsons disease.
There seems to be a higher preponderance of those who may have a genetic mutation that can lead to Parkinsons disease, Beck explained.
Sometimes younger people face a delayed diagnosis. Take Days early symptom shoulder pain. Often achy muscles in a 40-something is a sign of aging.
The symptoms by themselves can make it difficult for the diagnosis. Its a constellation of symptoms, Beck said. There are four key symptoms that are called cardinal symptoms that people will develop.
The symptoms include:
- Bradykinesia, a slowness of movement.
- Tremors.
- Balance or gait problems.
There are also a bunch of other symptoms that are associated with Parkinsons that are internal to the person, whats called non-motor symptoms. So that if you look at somebody who has Parkinsons they may look like theyre doing great, Beck said. But inside theyre having lots of problems.
Those include:
- Low blood pressure, also known as orthostatic hypotension.
- Constipation.
- Excessive sweating.
There is no cure for Parkinsons disease, but there are treatments.
About The Lecturio Medical Online Library
Our medical articles are the result of the hard work of our editorial board and our professional authors. Strict editorial standards and an effective quality management system help us to ensure the validity and high relevance of all content. Read more about the editorial team, authors, and our work processes.
Read Also: Idiopathic Parkinsons Disease Life Expectancy
Recommended Reading: Zhichan Capsule
What Are The Different Stages Of Parkinsons Disease
Each person with Parkinsons disease experiences symptoms in in their own unique way. Not everyone experiences all symptoms of Parkinsons disease. You may not experience symptoms in the same order as others. Some people may have mild symptoms others may have intense symptoms. How quickly symptoms worsen also varies from individual to individual and is difficult to impossible to predict at the outset.
In general, the disease progresses from early stage to mid-stage to mid-late-stage to advanced stage. This is what typically occurs during each of these stages:
Early stage
Early symptoms of Parkinsons disease are usually mild and typically occur slowly and do not interfere with daily activities. Sometimes early symptoms are not easy to detect or you may think early symptoms are simply normal signs of aging. You may have fatigue or a general sense of uneasiness. You may feel a slight tremor or have difficulty standing.
Often, a family member or friend notices some of the subtle signs before you do. They may notice things like body stiffness or lack of normal movement slow or small handwriting, lack of expression in your face, or difficulty getting out of a chair.
Mid stage
Mid-late stage
Standing and walking are becoming more difficult and may require assistance with a walker. You may need full time help to continue to live at home.
Advanced stage
What Is Parkinson’s Disease
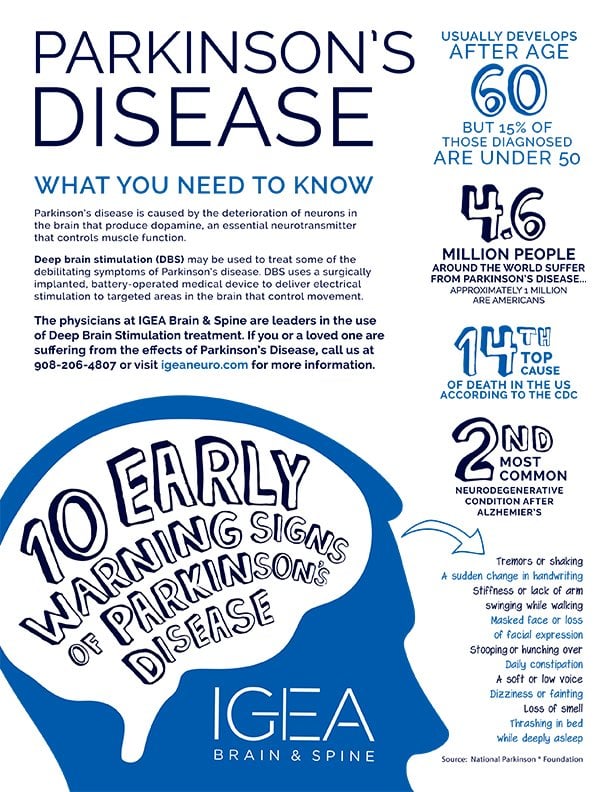
Parkinson’s disease is the second most common neurodegenerative disorder and the most common movement disorder. Characteristics of Parkinsons disease are progressive loss of muscle control, which leads to trembling of the limbs and head while at rest, stiffness, slowness, and impaired balance. As symptoms worsen, it may become difficult to walk, talk, and complete simple tasks.
The progression of Parkinson’s disease and the degree of impairment varies from person to person. Many people with Parkinson’s disease live long productive lives, whereas others become disabled much more quickly. Complications of Parkinsons such as falling-related injuries or pneumonia. However, studies of patent populations with and without Parkinsons Disease suggest the life expectancy for people with the disease is about the same as the general population.
Most people who develop Parkinson’s disease are 60 years of age or older. Since overall life expectancy is rising, the number of individuals with Parkinson’s disease will increase in the future. Adult-onset Parkinson’s disease is most common, but early-onset Parkinson’s disease , and juvenile-onset Parkinson’s disease can occur.
You May Like: Does Vitamin B12 Help Parkinson’s
Diagnosing Early Onset Parkinsons Disease
There is no single test to detect Parkinsons. A diagnosis may be difficult and take a while. The condition is usually diagnosed by a neurologist based on a review of your symptoms and a physical exam.
A DaTscan to visualize your brains dopamine system may help confirm diagnosis. Blood tests and other imaging tests, such as an MRI scan, dont diagnose Parkinsons. However, they may be used to rule out other conditions.
Why Is Distinguishing Young
Socially, people who are affected by PD at a younger age experience the disease differently they may be at a different stage of their career and often have less time to engage in their own care. They may also have children or are planning to have children and have questions regarding passing on PD genes.
Medically, doctors tailor treatment when it is a younger person with PD. The younger you are, the more likely the disease is genetic. Your care team may offer genetic testing or counseling. Younger brains also have a higher neuroplasticity potential which allows the brain to handle and respond to disease and therapy differently.
Recommended Reading: Parkinson’s Bike Therapy
What Are The Surgical Treatments For Parkinsons Disease
Most patients with Parkinsons disease can maintain a good quality of life with medications. However, as the disease worsens, medications may no longer be effective in some patients. In these patients, the effectiveness of medications becomes unpredictable reducing symptoms during on periods and no longer controlling symptoms during off periods, which usually occur when the medication is wearing off and just before the next dose is to be taken. Sometimes these variations can be managed with changes in medications. However, sometimes they cant. Based on the type and severity of your symptoms, the failure of adjustments in your medications, the decline in your quality of life and your overall health, your doctor may discuss some of the available surgical options.
Eo Parkinsonism Associated With Additional Characteristic Features
EO parkinsonism and metals in the brain
Brain metal accumulation can manifest clinically as early-onset parkinsonism in several neurological disorders. Various metals can be accumulated in the brain and other body tissues in these conditions , calcium in Fahrs disease, and manganese in hypermanganesemia). Some of these disorders are genetically inherited, while others are acquired .
Typically, the clinical suspect for these conditions emerges after brain imaging studies . However, associated systemic findings, such as hepatic involvement in Wilsons disease and hypermanganesemia, can be the first clue to suspect metal accumulation in the brain .
Wilsons disease
Wilsons disease is distributed worldwide, with an estimated prevalence of 1 case per 30,000 live births in most populations . However, in some isolated populations, such as a small mountain village on the island of Crete, the prevalence is much higher , due to high rates of consanguinity .
Copper accumulation is associated with a progressive neurodegeneration of basal ganglia leading to a complex movement disorder often associated with bulbar symptoms. The movement disorder is usually characterized by tremor, dystonia, and/or parkinsonism. Bulbar symptoms consist of dysarthria, drooling and/or dysphagia. In addition, a range of additional neurologic features may be present, including cerebellar ataxia, chorea, hyperreflexia, seizures, cognitive impairment, and psychiatric features .
Fahrs disease
Read Also: Parkinson Bicycle Cleveland Clinic
Diagnosis In Young Onset Parkinsons
Many young onset patients experience delay in diagnosis given the uncommon age and often different symptoms as outlined below. Similar to late onset patients, the diagnosis is made based on history and clinical examination. There are still no proven diagnostic tests that can definitively diagnose PD. In some cases, other mimics of Parkinsons need to be evaluated for given their increased likelihood in younger patients. Given the complexities, it is important to seek evaluation by a neurologist and in many cases a movement disorder specialist.
In addition, young onset patients are more likely to have a genetic risk factor or cause to their symptoms, especially if there is a family history. Genetic testing can be considered, but should always be done after consulting a physician and in many cases a genetic counselor.
Parkin Rbr E3 Ubiquitin Protein Ligase Gene
The PRKN gene is located on chromosome 6 . The product of this gene is parkin, an E3 ligase in the ubiquitin proteasome system, which promotes proteolysis and degradation of dysfunctional mitochondria . A mutation of this gene was first described by Kitada et al. in a Japanese family with autosomal recessive Parkinson’s disease in 1998 . Since its first description, several mutations in this gene have been linked to autosomal recessive Parkinson’s disease . Table 4 briefly summarizes the most common clinical characteristics of PRKN-related PD.
Table 4. Common Clinical Characteristics of PRKN PD
| Young onsetConsistent good response to levodopaSlower progression compared to idiopathic PDLow rate of cognitive declineLower rate of hyposmiaHigher frequency of dystonia, that could be the manifesting feature, especially affecting the lower limb |
Further studies demonstrated that, despite the clinical resemblance, the neuropathology is different from idiopathic PD, and usually the neurodegeneration is not associated with Lewy bodies .
A smaller number of studies focused on DAT PET imaging with 11C-N–2-carbomethoxy-3-nortropane or CFT in PRKN mutation carriers, and found a reduction of binding in the striatum, without significant differences from non-PRKN young-onset PD .
Also Check: Fitflop Shoes For Parkinson’s