What Causes Pain In Cases Of Parkinsons Syndrome Sufferers
Parkinsons Syndrome Sufferers may present with various combinations of back, buttock and leg pain, numbness and muscle weakness, Symptoms are often aggravated by an abnormal asymmetrical gait arising from loss of spatial awareness muscle spasm and loss of limb control. The back pain may arise from irritation within the disc wall but more commonly arises from the pinching of the trapped nerve in the exit doorway from the spinal column. The foramen may be distorted and the nerve is tethered by years of scarring reaction to repetitive bruising, can not evade the pinching by the bulging distorted disc wall or overriding facet joints . The disc may be degenerate and bulging and contribute to the irritation of the tethered nerve. When advanced the compression causes numbness and weakness to develop. The patchy weakness or spasm of the muscles controlling the spinal segments results in asymmetrical loss of control or stiffness of the disc levels and aggravation of the effects of the local pathology at each level and aggravation of symptoms arising at these levels.
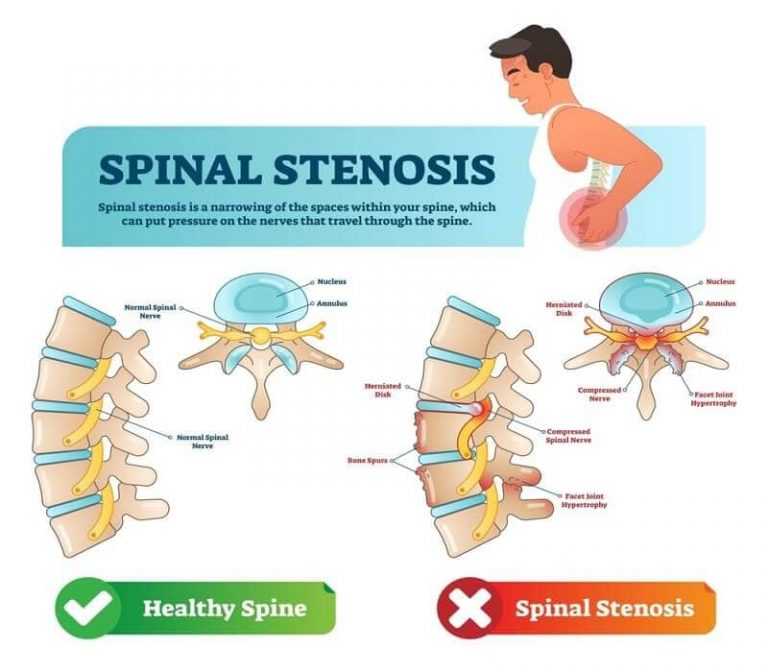
Is There A Test For Spinal Stenosis
Doctors use a variety of tools to see if you have spinal stenosis and rule out other conditions, including:
- Medical and family history, which helps to determine if an injury, aging, or an underlying condition is causing your symptoms.
- Physical exam, which may check how you move and walk, when your pain happens, muscle strength in your arms and legs, and your balance.
- Imaging tests such as x-rays, MRI , and computerized tomography scans.
Treatment For Cervical Myelopathy
For those rare occasions where patients with cervical spondylotic myelopathy have tremors, surgery won’t necessarily help the condition, Dr. Highsmith said.
“If it’s from the cervical myelopathy, there’s usually been permanent damage. So even with surgery and decompression, a patient still often has symptoms,” Dr. Highsmith said. “It’s one of those things we treat but sometimes doesn’t get better.”
In the case of the 91-year-old patient, doctors performed procedure to help manage the condition. An ACDF is a surgical procedure to treat spinal cord compression by removing a degenerative or herniated disc in the neck.
Within eight weeks after surgery, the man’s tremors went away, and his unsteadiness eventually resolved, the report states.
Also Check: Physiotherapy Management For Parkinson’s Disease Ppt
Study Found Tremors Can Be Due To Spinal Compression
Parkinson’s was the initial diagnosis for one 91-year-old man who was hospitalized after having tremors in his limbs. The tremors progressed over two weeks to the point where the man could not feed himself or walk without support.
The case of the man’s diagnosis was the focus of a medical report published in 2019 by physicians in the Department of Orthopaedic Surgery, Division of the Spine at Singapore’s Tan Tock Seng Hospital.
Besides the tremors, the man’s progressing symptoms included difficulty with fine motor skills such as using chopsticks and buttoning his shirt, the report states.
However, Parkinson’s was eventually ruled out because the patient didn’t have other symptoms of the disease. Instead, his symptoms, including the tremors, were attributed to cervical spondylotic myelopathy, a compression of the spinal cord in the neck. In this case, the compression was caused by a encroaching into the spinal canal and compressing the spinal cord .
Operative Procedure & Postoperative Course
Considering the patientâs degree of deformity and pain, we elected to perform revision surgery. Pedicle screws and rods were reinserted from the L1to S1 levels with iliac screws after performing a partial pedicle subtraction osteotomy at the L4 level with removal of the intervertebral discs at the level of L34 . The patientâs intraoperative and postoperative periods were uneventful, and she was able to walk with a straight back without any support a few days postoperatively. Follow-up X-rays obtainedapproximately 18 months after surgery showed significant improvement in her spinal parameters and kyphoscoliosis. Pre and postoperative surgical outcomes were measured with Modified Scoliosis Research Society-23 Outcome Instrument scoring system . A mean postoperative score of 20 out of 25 indicated a satisfactory outcome.
Lateral thoracolumbar X-ray showing PPSO & discectomy performed at the L4 and L34 level, respectively, and lateral thoracolumbar X-ray showing the correction angle of approximately 30 degrees at the same level postoperatively. PPSO : partial pedicle subtraction osteotomy.Follow-up anteroposterior and lateral whole spine X-rays showing satisfactory correction of coronal and sagittal imbalance. *Indicates the lumbar lordosis, **Indicates sagittal vertical axis. PI : pelvic incidence, LL : lumbar lordosis, SVA : sagittal vertical axis.
Read Also: What Is An Essential Tremor Parkinson
New Jersey Spine Treatment Center
Our team of board-certified spinal specialists at theBrain, Spine & Neuromuscular Care Center of The Department of Neurosurgery at Rutgers Health and RWJBarnabas Health treat a variety of all types of spinal stenosis affecting all areas of the spine, including lumbarspinal stenosis. We treat thousands of patients every year who suffer from neurological conditions, and offer a multidisciplinary approach from a dedicated, board-certified team of physicians who specialize in neuroscience, from neurology to neurosurgery and beyond.
Outcomes And Radiological Measurements
Data for age, gender, body mass index , disease duration from diagnosis of compression fracture to that of burst fracture and/or appearance of neurological symptoms, surgical procedures, and postoperative complications were acquired from medical charts. In patients with PD, the Hoehn & Yahr stage before surgery and at follow-up was assessed by senior neurologists. Clinical symptoms, low back pain, radicular leg pain, and cauda equine sign were also stratified based on cleft formation. Radicular leg pain was defined as lower extremity pain consistent with a neurological dominant region. Cauda equina syndrome was diagnosed based on symptoms of neurogenic intermittent claudication or motor and/or sensory disturbance, including bladder dysfunction. The Japanese Orthopaedic Association score for neurological status was obtained before surgery and at follow-up, with all neurological evaluations performed by senior spine surgeons. Neurological improvement rate at follow-up was calculated using the following formula: ×100/. Plain standing radiographs were used to identify other vertebral collapses, the type of vertebral collapse, lumbar lordosis and local lumbar lordosis before surgery and at follow-up.
Figure 3
Read Also: What Is The Best Parkinson’s Charity
Parkinson’s Misdiagnosis: Thyroid Issues
Thyroid issues affect muscle strength and can cause fatigue, muscle aches, stiffness, and joint pain. The early stages of Parkinsons could look similar to thyroid problems. However, with time and as a patient learns more about his or her own symptoms, they are able to provide a fuller picture, which can lead to a clearer diagnosis.
My husbands endocrinologist adjusted his thyroid medicine and was so surprised when he did not feel any better.
Case : Bilateral Gpi Dbs
This patient was a 59-year-old man with PD and severe camptocormia. Parkinson disease was diagnosed based on the initial presenting symptoms of a severe stooped posture, decreased fine finger movements, and bilateral hand tremor. The patientâs camptocormia only minimally responded to dopaminergic medications, and he would fall several times a day. He had begun wearing kneepads to prevent further injury from his frequent falls. He underwent placement of bilateral GPi DBS electrodes to alleviate his parkinsonian symptoms as well as treat his camptocormia. He was discharged to an acute rehabilitation facility on postoperative Day 5 in good condition. At 15-month follow-up, while having some improvement in his parkinsonian symptoms, he continued to suffer from severe camptocormia.
You May Like: Games For Parkinson’s Patients
Case : Bilateral Stn Dbs
This patient was a 59-year-old man with advanced idiopathic PD and motor fluctuations. Preoperatively it was noted that he had severe camptocormia . He underwent placement of bilateral STN deep brain stimulators and a right chest dual channel pulse generator. He was discharged to an acute rehabilitation facility on postoperative Day 6 in good condition for several weeks after his hospitalization. At 2-year follow-up, his gait and ease of ambulation had improved, but he had no significant improvement in his camptocormia posture .
Case 1. Preoperative image of patient with severe camptocormia prior to DBS , and postoperative image obtained after DBS at 24-month follow-up .
What Is Special About Parkinsons Syndrome Sufferers
Parkinsons Syndrome is a condition where the important nuclei below the brain become dysfunctional resulting in impaired communication and transmission of nerve impulses to and from nerve fibres throughout the body. Consequently some cognitive processes, eyesight focus, muscle control or strength may deteriorate. This often presents in a haphazard fashion with increasing stiffness of the joints and muscles and intention tremor most noticeable in the hands. Fine movements and writing ability deteriorate, The gait deteriorates as seem as a shuffling pattern with small steps with a quickening of gait as power is mustered and spasm is overcome, Whilst there is a downhill trend the process of deterioration may arrest for periods.
Seldom does this process directly generate nerve pain such as sciatica. Back or Neck pain and pain referred in to the arm or leg may arise in Parkinsons Syndrome Sufferers as part of the Degenerative Disc Disease seen in the rest of the population and with the same pathologies disc protrusions, nerve entrapment / scarring / tethering, Lateral Recess Stenosis, Axial Stenosis, Spondylolytic Spondylolisthesis, vertebral slippage, Instability, Failed Back Surgery or failed chronic pain management.
Read Also: Living Alone With Parkinson’s
Our Treatment Method Provides For True Healing
It takes innovative thinking to create a new possibility. Our unique Treatment Protocols are just that. We specialize in what we do. Our saying is Specificity equals Success. The success is in what were doing. We get specific on what the problem actually is. When we can get specific about the problem, and specific with technology that serves that problem precisely, that allows us to get a good outcome.
We dont claim to be, or have, better outcomes at something that everyone else is already doing . We simply do something much different, and outside the box, that is unique to all other forms of care traditionally provided. Our Treatment Protocol is not physical therapy, spinal injections, or surgery.
Dementia With Lewy Bodies

Also Check: Natural Cure For Parkinson’s Disease
A Dilemma Of Symptom Overlap
Patients with Parkinsons disease may exhibit symptoms similar to those observed in cervical spondylotic myelopathy , including ataxia, weakness, and bowel or bladder dysfunction. These similarities present diagnostic and therapeutic challenges when PD and CSM coexist. While CSM is typically treated with surgical decompression , PD requires pharmacologic therapies and is expected to derive little benefit from decompression. This poses a dilemma for both neurologists and spine surgeons treating patients with PD who may have evidence of cervical spondylosis and myelopathy.
Clinical and quality-of-life outcomes following cervical decompression in the PD population remain undefined. Defining these outcomes may improve patient management and help avoid unnecessary surgical intervention. To that end, Cleveland Clinic Center for Spine Health clinicians and researchers recently sought to investigate clinical and QOL outcomes following cervical decompression among patients with CSM with and without coexisting PD. We hypothesized that both groups would benefit from surgery but that patients with concomitant PD would experience inferior outcomes.
Figure. Preoperative sagittal T2 MRI of a patient with coexistent cervical spondylotic myelopathy and Parkinson disease. Note the severe cervical stenosis and cord compression at C3-4and C4-5 . Postoperative X-ray after the patient underwent laminectomies at C3 through C5 and extension of her fusion to C3 via a dorsal approach.
Study Design In Brief
We retrospectively identified all patients with coexisting PD and CSM who underwent cervical decompression at Cleveland Clinic between June 2009 and December 2014 and then matched them to controls with CSM alone who underwent cervical decompression over the same period by the same team of spine surgeons . Matching was done on the basis of age, gender, American Society of Anesthesiologists classification, preoperative modified Japanese Orthopaedic Association score and operative parameters.
The primary outcome measure was postoperative improvement in mJOA score at patients last follow-up visit. The mJOA scale ranges from 0 to 18, with lower scores indicating greater neurologic disability. Two points was considered the minimum clinically important difference. Additionally, scores on the Nurick scale were collected to measure ambulatory status, with greater scores indicating greater impairment.
In a secondary QOL analysis, outcomes included QOL improvement as measured by the EuroQol 5 dimensions questionnaire , the Pain Disability Questionnaire and the Patient Health Questionnaire 9 . These measures were prospectively collected before and after surgery.
Simple and multivariable linear and logistic regression analyses were used to assess the impact of PD on primary and secondary outcomes.
Also Check: Medications For Parkinson’s Disease And Side Effects
Interested In Parkinsons Disease Research Sign Up For Our Forums And Join The Conversation
A total of 97 Parkinsons patients at a mean age of 67.7 years, including 60 men, and 97 individuals used as controls at a mean age of 67.5 years, including six men, without the disorder or other neuromuscular diseases, filled out a questionnaire on the intensity of local lumbar back pain. The intensity of leg radicular pain caused by inflammation and/or injury to a spinal nerve root was quantified by the visual analogue scale a continuous scale used to measure pain intensity.
In addition, the participants permanent functional disability was assessed via the Oswestry Low Back Pain Disability Questionnaire a self-completed questionnaire that includes 10 different topics: intensity of pain, lifting, ability to care for oneself, ability to walk, ability to sit, sexual function, ability to stand, social life, sleep quality, and ability to travel.
Patients were further asked to describe the painful sensation they experience as pricking, tingling, burning, paresthesia often described as feelings of pins and needles, or numbness or other.
The team also assessed Parkinsons duration, medications being used, severity of motor symptoms as assessed by the Unified Parkinsons disease rating scale part III and the Hoehn and Yahr stage, which is a system used to assess symptom progression.
According to the ODI results, minimal disability was reported by 43.8% of Parkinsons patients, moderate disability by 27.5%, severe disability by 22.5%, and crippled by 6.3%.
We Can Examine All Of The Above And You Can Experience The Miracle
TAKEYUKI SAKASHITA
Fifteen years of experience in this field, conducting more than 2000 treatment sessions in a year.
Began martial-arts at 20 years of age to learn body care for myself.
Stayed Yunnan province in china and researched medical treatment while practing martial arts in 2012.But there are nothing about medical treatment in chaina.
Studied Osteopathy and some Japanese manual therapy in 2013~2018.
Currently studying under the successor of the oldest Japanese martial arts.
Give treatment for Neurological disorder and paralysis all over the world and in Japan.
OTHER STAFFS
Ordinary he goes to around Japan as treatment for paralysis and neurological disorders.
He has correct technics and reliance of patients.
KYONHI
She does treatment for paralysis and neurological disorders everyday.
Most of her patients have strong trust to her and speak of satisfaction.
Don’t Miss: Parkinson’s Phlegm At Night
What Are The Symptoms Of Spinal Stenosis
Symptoms of spinal stenosis happen when the spaces within the spine narrow and put pressure on the spine. This occurs most often in the lower back and neck. For most people, symptoms develop slowly, and some people may not have any symptoms.
Symptoms of spinal stenosis in the lower back can include:
- Pain in the lower back.
- Burning pain or ache that spreads down the buttocks and into the legs, that typically worsens with standing or walking and gets better with leaning forward.
- Numbness, tingling, or cramping in the legs and feet. These may get worse when you stand or walk.
- Weakness in the legs and feet.
Symptoms of spinal stenosis in the neck may include:
- Numbness or tingling that spreads down the arms into the hands.
- Weakness in a hand, arm, or fingers.
Recommended Reading: Serotonin Syndrome And Parkinsonâs
What Is Wrong With Conventional Surgery
The use of multi-level open surgery in Parkinsons Syndrome Sufferers including microdiscectomy, decompression, solid or flexible fusion and is an overkill with negative side-effects including blood loss, potential nerve and tissue damage, extended post-operative care and unnecessarily operating on pain-free levels is fraught with aggravation of the current symptom status. It is not as effective as Foraminoplasty in addressing and ameliorating the effects of Parkinsons Syndrome Sufferers, rather it runs the risk of increased neurological complications as well as causing the complications of recurrent disc bulging, infection, nerve damage and scarring round the nerve, implant failure, major vessel damage or sexual dysfunction.
Recommended Reading: How To Treat Parkinson’s
Less Common Misdiagnoses Of Parkinsons Disease
- Reactions 0 reactions
Anyone with Parkinsons disease can tell you that the road to diagnosis is anything but direct. Too often, it comes down to a bit of luck as in, finding a doctor experienced enough to connect the symptoms straight away as Parkinsons disease.
For most members of the ParkinsonsDisease.net community, it took several doctor visits and several physicians to reach the correct diagnosis. Prior to that, the wrong diagnoses were all over the map.
To learn more, we asked members of our : Were you ever misdiagnosed with another condition before your PD diagnosis?
Almost 90 community members shared, naming many misdiagnoses. Here are the 7 less common answers.