Nursing Diagnoses/outcomes And Interventions Of Icnp For Patients With Parkinson’s Disease In Rehabilitation
We analyzed 2123 nursing documentations from 352 medical records of patients with PD who participated in a rehabilitation program at a specialized centre in Rio de Janeiro, Brazil, from May 2009 to March 2014. From these documents, empirical evidence regarding nursing diagnoses, outcomes, and interventions was extracted. These dates were crossmapped with ICNP® 2013 and validated by judges to build a terminological subset of ICNP® for patients with PD in rehabilitation .
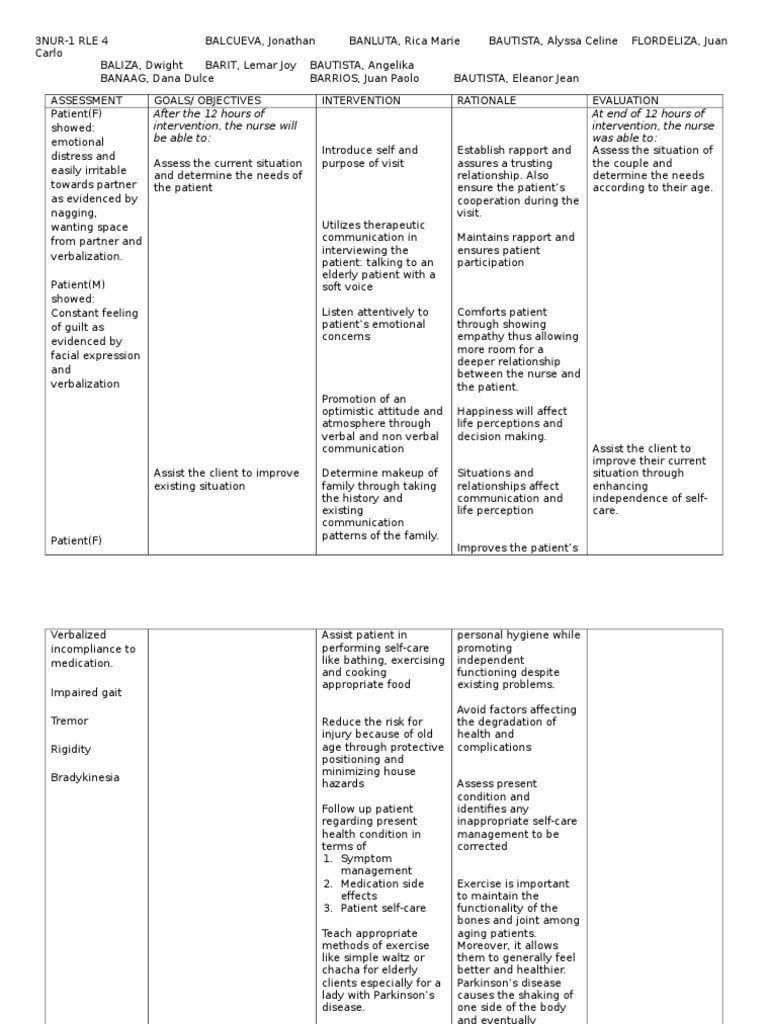
The diagnoses, outcomes, and interventions were divided into categories including motor symptoms, nonmotor symptoms, and principles of rehabilitation, as shown in Figure 2.
Greater variability was observed in nursing diagnoses, outcomes, and interventions related to nonmotor symptoms of Parkinson’s disease in general, it appears that nurses work in a comprehensive and communicative manner with other professionals on multidisciplinary teams.
Figure 2.
Treatment Of Parkinsons Disease
Currently, Parkinsons disease has no cure. However, treatments are extremely helpful in managing its signs and symptoms.
Box : Further Assessment Of Depression In Patients With A Chronic Physical Health Problem6
If a patient with a chronic physical health problem answers yes to either of the depression identification questions , a practitioner who is competent to perform a mental health assessment should:
- ask three further questions to improve the accuracy of the assessment of depression, specifically:
- during the last month, have you often been bothered by feelings of worthlessness?
- during the last month, have you often been bothered by poor concentration?
- during the last month, have you often been bothered by thoughts of death?
© NICE 2009. Depression in adults with a chronic physical health problem: recognition and management. Available from www.nice.org.uk/cg91 All rights reserved. Subject to Notice of rights. NICE guidance is prepared for the National Health Service in England. All NICE guidance is subject to regular review and may be updated or withdrawn. NICE accepts no responsibility for the use of its content in this product/publication.
Recommended Reading: Cleveland Clinic Parkinson’s Bicycle Study 2017
Availability Of Data And Materials
On the consent form, participants will be asked whether they agree with the following statement: I know that participating in this trial is voluntary. I also know that at any time I can decide to withdraw from the trial. I do not have to give any reason. The data that is collected until that moment, will be used for the research. A number of people are allowed to view my data. These include the members of the research team, the Ethical Committee, people that verify the safety of the trial , and the Dutch Healthcare Inspection.
This trial does not involve collecting biological specimens for storage. The aggregated datasets analyzed during the current study will be available from the corresponding author upon reasonable request.
Risk For Falls And Injury
With Parkinson’s disease, bradykinesia, rigidity and tremors can lead to gait problems and a risk for falls and injury.
The nursing assessment includes evaluating the patient’s movement and gait and understanding his/her home environment. Improving movement and gait can reduce the risk of falls .
To promote safety and avoid falls, suggest removing potential hazards in the home, such as loose rugs or obstacles in pathways.
Recommend handrails on both sides of stairways, non-skid surfaces and grab rails in showers and tubs, and raised toilet seats. Suggest that patients with PD wear appropriate shoes with smooth, non-slippery soles. Encourage the family or caregiver to supervise ambulation, as needed. A bedside urinal or commode may be helpful for some patients to prevent nighttime falls.
Some patients with Parkinson’s disease experience orthostatic hypotension. If patients become dizzy when moving from a lying to a standing position, teach them to rise slowly, to remain seated for a few minutes with legs dangling over the side of the bed and ex feet upward, then to stand, sitting back down immediately if they feel dizzy. Recommend having someone with them when they stand up.
Review medications, as some anti-Parkinson’s drugs may cause dizziness these can be discussed with the physician to see if alternative medications might be beneficial.
Don’t Miss: On Off Phenomenon
Monoamine Oxidase B Inhibitors
- Selegiline hydrochloride
- Rasagiline mesylate
The enzyme monoamine oxidase B breaks down dopamine in the brain. MAO-B inhibitors prevent this breakdown, thus increasing the amount of dopamine in the brain and reducing the motor symptoms of Parkinson’s disease.
MAO-B inhibitors to treat the symptoms of PD can either be used alone or with levodopa. In early PD, they can delay the need for starting levodopa. Later in the disease, they can be given with levodopa, to enhance and prolong the effects to levodopa, thus reducing the “wearing off” phenomenon. When taken in combination with levodopa, it may allow the dose of levodopa to be reduced.
Side effects of MAO-B inhibitors include nausea, dizziness, headache, confusion, postural hypotension, hallucinations and insomnia. Confusion and hallucinations are more common in the elderly.
MAO-B inhibitors should not be used with meperidine or other opioids because of potential life-threatening drug interactions at high doses. MAO-B inhibitors at high doses could also potentially precipitate a hypertensive crisis if very large amounts of tyramine containing foods are eaten. Serious drug interactions have been reported with MAO-B inhibitors and some antidepressants.
Selegiline and rasagiline are available as standard oral tablets. An oral disintegrating selegiline tablet is also available for people who have difficulty swallowing tablets.
Inclusion And Exclusion Criteria
The inclusion and exclusion criteria for patients are kept purposefully broad in order to represent the full diversity of the PD spectrum and thus generate results that apply to real clinical practice. All patients with PD, regardless of disease severity or disease duration, male and female, aged 18years or older at the time of PD diagnosis are eligible. We will only exclude patients for the following reasons:
-
Lack sufficient knowledge of the Dutch language to complete questionnaires
-
Have received care from a PDNS in the past 2 years
-
Have a score < 18 on the Mini Mental State Examination and < 12 on the Frontal Assessment Battery
-
Have a type of atypical parkinsonism caused by medication , a metabolic disorder , encephalitis, or a neurodegenerative disorder
-
Residing in a nursing home or another type of residential care facility
-
Have any other medical or psychiatric disorder that, in the opinion of the researcher, may compromise participation in the study
Don’t Miss: Similar To Parkinsons
Signs And Symptoms Of Parkinsons Disease
- Tremor. The presence of tremors is one of the triad symptoms of Parkinsons disease. Tremors usually start in the limbs, most commonly in the hands and fingers. They are likely to occur when the body is at rest and relaxed. Pill-rolling tremors are common in Parkinsons disease patients. It is characterized by the rubbing of thumb and forefinger back and forth.
- Bradykinesia. One other main symptom of PD is slow movements or bradykinesia. Individuals with PD display a distinctive slow and shuffling gait. Slowness in movements often make it more difficult for people with PD to complete activities of daily living.
- Rigidity . Muscle stiffness is also a common sign of PD. It may occur in any part of the body and may lead to dystonia or uncontrolled painful muscle cramps.
- Impaired posture and balance. Most people with PD often have a stooped posture.
- Loss of automatic movements. Unconscious movements such as blinking, smiling, and swinging of hands when walking may be reduced in people with Parkinsons disease.
- Anosmia. Loss of the sense of smell may occur even years before the diagnosis of PD.
- Speech changes. Changes in speech may also be noted in people with PD. Their speech may become soft, fast, slur, and their tone may become monotonous.
Data Extraction And Quality Assessment
All articles were read by two independent review authors and data extracted according to predefined criteria, with any discrepancies resolved by discussion. Publications were assessed for methodological quality by recording specified eligibility criteria, method of randomisation and blinding, concealment of allocation, similarity of patients in treatment groups at baseline, variation in cointerventions received by patients throughout the trial period, whether an intention to treat analysis was performed, and the number of patients lost to follow-up.
Recommended Reading: Prayer For Parkinson’s Disease
Transdermal And Duodenal Drug Administration
Some medications may be delivered transdermally or by enteral duodenal infusion. A transdermal patch delivers a dopamine agonist around the clock to decrease off time its used in combination with L-dopa. Duodenal infusion avoids gastric emptying problems. It can be used short-term through a nasogastric tube and long-term through a percutaneous endoscopic gastrostomy tube that extends into the duodenum. These methods are still under review.
Caring For Patients With Parkinsons Disease
Among the most common neurogenerative diseases, Parkinsons disease most often affects people older than age 60. Yet one in 20 patients is younger than 40 when diagnosed. Its cause isnt known, although research now centers on genetic and environmental factors and brain trauma.
PD is characterized by loss of dopaminergic nerve cells in the substantia nigra of the basal ganglia in the brains lower region, on either side of the brainstem. Dopamine is integral to movement coordination once 70% of dopaminergic nerve cells are lost, PD signs and symptoms become evident. As dopamine levels continue to fall, manifestations become more apparent and new signs and symptoms arise. Another physiologic hallmark of PD is presence of Lewy bodies containing alpha-synuclein in this same brain region.
Don’t Miss: Voice Amplifiers For Parkinson’s
Other Motor Symptom Medications
- Amantadine hydrochloride
Amantadine is an anti-viral drug that was developed in the 1960’s to treat influenza. It was found coincidentally to decrease the symptoms of Parkinson’s Disease and levodopa-induced dyskinesias. It is not clear how amantadine works to improve the symptoms of PD. It can be used alone in the early stages of PD, especially to help those with tremor, or combined with anticholinergic drugs or levodopa. The effectiveness of amantadine seems to wear off after several months for about half the patients taking this drug.
Side effects include nausea, light-headedness, insomnia, confusion, hallucinations, anxiety, mottled skin , dry mouth, constipation, orthostatic hypotension, headache and possible heart failure . It should not be used by patients with angle-closure glaucoma. Patients taking amantadine should consult their physician before taking any new medications, including OTCs. When stopping this drug, it should be tapered off slowly. Stopping amantadine abruptly could precipitate a parkinsonian crisis similar to neuroleptic malignant syndrome .
Symptoms include fever, rigidity, cognitive changes, and sometimes tremor, tachycardia, tachypnea, diaphoresis, dystonia and chorea. Neuroleptic malignant syndrome is potentially life threatening and requires immediate emergency care and restarting of dopaminergic medications.
What Should You Not Do If You Have Parkinsons Disease
Your immune system can be harmed by excessive consumption of sugary foods and drinks. By reducing your sugar intake and choosing natural sweetened foods, Parkinsons symptoms can be managed. You shouldnt consume too much protein. For some Parkinsons medications, eating a lot of beef, fish, or cheese could reduce their effectiveness.
Read Also: Pfnca Wellness Programs
The Role Of Nurses In Parkinson’s Disease
Research has shown increasing specialization among nurses who care for patients with PD thus, knowledge of the pathophysiology of this disease is arguably an important starting point for vocational training . Based on this, we sought to hierarchically organize the major motor and nonmotor symptoms of PD using evidence gathered from the literature .
Figure 1.
Classification of the main motor and nonmotor symptoms in Parkinson’s disease.
The symptoms of PD are divided into motor and nonmotor each of these classifications contains various other signs and symptoms related to both the neurodegenerative disease process itself as well as multifactorial causes. Thus, hierarchical organization of symptoms is not an easy task, and various descriptions have been proposed to facilitate understanding of the pathophysiology of the disease however, none of them have structured the symptoms into an organizational chart.
Our research on nursing diagnoses, outcomes, and interventions was based on this chart.
Nursing Assessment And Interventions
Managing Parkinson’s disease is a collaborative effort involving the patient, the patient’s family or caregiver, and the health care team. On the health care team, the role of the nurse is to provide education about PD, to help monitor medication management, and to help the patient maintain optimal functioning with as much independence as possible. PD is a complex multisystem disease. Symptoms vary from one person to the next. For each individual, symptoms change over time as the disease progresses. The nursing assessment is an ongoing process to monitor the symptoms of the disease and the effectiveness of treatment in managing these symptoms. Assessment includes: history of symptoms physical assessment and specific review of medication effectiveness or side effects.
History ofsymptoms : mobility problems, fatigue, sleep problems, eating/swallowing problems, weight gain or loss, falls, episodes of fainting or feeling light-headed, pain, muscle cramps, constipation, urinary problems, sexual dysfunction, excessive sweating, skin problems, restless leg syndrome, depression or other mood changes, hallucination or delusions, and behavior changes.
A nursing physical assessment includes: evaluation of overall appearance, weight, affect, facial expression, drooling, tremor , muscle rigidity, posture, gait, coordination, speech, skin, scalp, mental status.
Also Check: Does Sam Waterston Have Parkinsons
Depression In Parkinsons Disease
Depression is a common non-motor symptom in PD and is thought to occur in over 50% of people.2 Depression in PD can occur for various reasons but is generally considered a consequence of a chemical depletion in the brain and a response to living with the challenges of the condition.3 It is widely accepted that people with depression, regardless of whether they have PD or not, have an increased risk of suicide than those who do not have depression.4 A recent review of literature suggests that people with PD are much more likely to experience suicidal thinking than the general population, but it remains unclear if the risk of suicide is increased. The review concluded that there was often conflicting evidence on suicide and suicidal ideation in the Parkinsons population and that more studies were needed. However, it does state that the evidence suggests aggressive management of depression is the best approach.5
Read This Article To Learn More About:
- assessing mental health in Parkinsons disease
- the overlap between Parkinsons disease non-motor symptoms and depression
- the role of the Parkinsons disease nurse specialist in supporting people with Parkinsons disease.
Parkinsons disease is a progressive neurological condition that is characterised by tremor, stiffness, and slowness. These overt physical signs are commonly referred to as motor symptoms. However, signs unrelated to movement can manifest along the way, or even before the disease is formally diagnosed these non-motor symptoms can include autonomic, memory, mental health, and mood problems.
When a person is diagnosed with PD, a multi-disciplinary health and social care team often supports them. The team can include neurologists, occupational therapists, and Parkinsons disease nurse specialists . PDNSs are often central in coordinating care, conducting regular monitoring of the person with PD, managing medication, and generally being an accessible source of information and advice for patients, families, and other healthcare professionals. This framework for the role of the PDNS is supported by the 2017 NICE Guideline 71 on Parkinsons disease in adults.1
Don’t Miss: On And Off Phenomenon
Parkinsons Disease Nclex Review Care Plans
Nursing Study Guide on Parkinsons Disease
Parkinsons Disease is a common neurodegenerative disease characterized by changes in movement and posture.
It is a progressive illness with symptoms starting from barely noticeable to obvious signs and symptoms.
Tremors, rigidity, and bradykinesia are the triad of symptoms of Parkinsons disease.
Parkinsons disease has a prevalence rate of 0.5-1% in the 65-69 years old population. Its occurrence rises as the age progresses and its incidence is second to Alzheimers disease.
Data Collection And Management
Patients will be given a unique personal identification code not containing any information that refers back to the individual. The key file connecting personal identification codes to the individual patient will be stored on a secure Radboudumc data server. Only the research team has access to this key. The key file will be stored on a different server from the one with acquired study data for 5 years, allowing the research team to contact patients after they have finished the study. After 5 years, the key file will be destroyed.
Data from all paper-based case report forms completed by the researcher will be entered manually into an online certified data management system . Online CRFs will automatically be recorded in Castor EDC. When patients or caregivers are not able to complete questionnaires online, they also have the opportunity to do this on paper. We will send out the questionnaires by post, and patients can return the completed questionnaires using a self-addressed envelope. These questionnaires will be entered manually into Castor EDC. Both online and paper-based CRFs only contain the personal identification code.
Clinical notes taken by the PDNS in the online study report will also not contain any information that refers back to the individual. PDNSs are instructed to make notes according to a predefined structured format without mentioning personal information that traces back to an individual patient. The study report will be completed in Castor EDC.
You May Like: Yopd Life Expectancy