Additional Resources That Can Help Support Parkinsons In The Home
Parkinsons Home Care services, in order to be truly effective, require coordination and collaboration among a variety of specialties. The reason this coordination is so important is there are a variety of symptoms that may need to be managed through both medicine but also exercise and diet.
All of these methods can impact Parkinsons Disease symptoms in a variety of ways, as well as other symptoms that may not be related to Parkinsons Disease.
Broad Street incorporates the collective treatment plans from all of the specialists into your daily routine. Not to overwhelm, but to simplify and encourage.
Also, because we work with you so frequently, and with our Nurse Oversight, Broad Street can be helpful in communicating with these specialists, so they are well informed as to how the treatment plans are working.
We work this way so we can help manage your symptoms instead of your symptoms managing you.
Some of the specific specialist we work with and have as part of our Parkinsons support services network include:
-
Movement Disorder Specialists and Neurologists
-
Other Specialists including Cardiologists, Sleep Disorder Specialist,
-
Geriatric Physicians
Clinical Oversight From A Nurse Supervisor
Clinical oversight is also provided throughout your care by a Nurse Supervisor who provides support to you and your care professionals and addresses any changes in your condition. Nurse oversight is also about communication.
Through direct feedback and proactive management, we ensure that necessary information is shared with your family and your multidisciplinary team.
This allows us to work together in providing the most effective level of care.
THE BEST RESULTS
If You Have Parkinson’s Disease
If you have been diagnosed with Parkinson’s, call your doctor if:
- You notice any significant change in your symptoms, such as severe episodes of freezingâa sudden loss of mobilityâwhich may affect walking.
- Your response to your medicine changes.
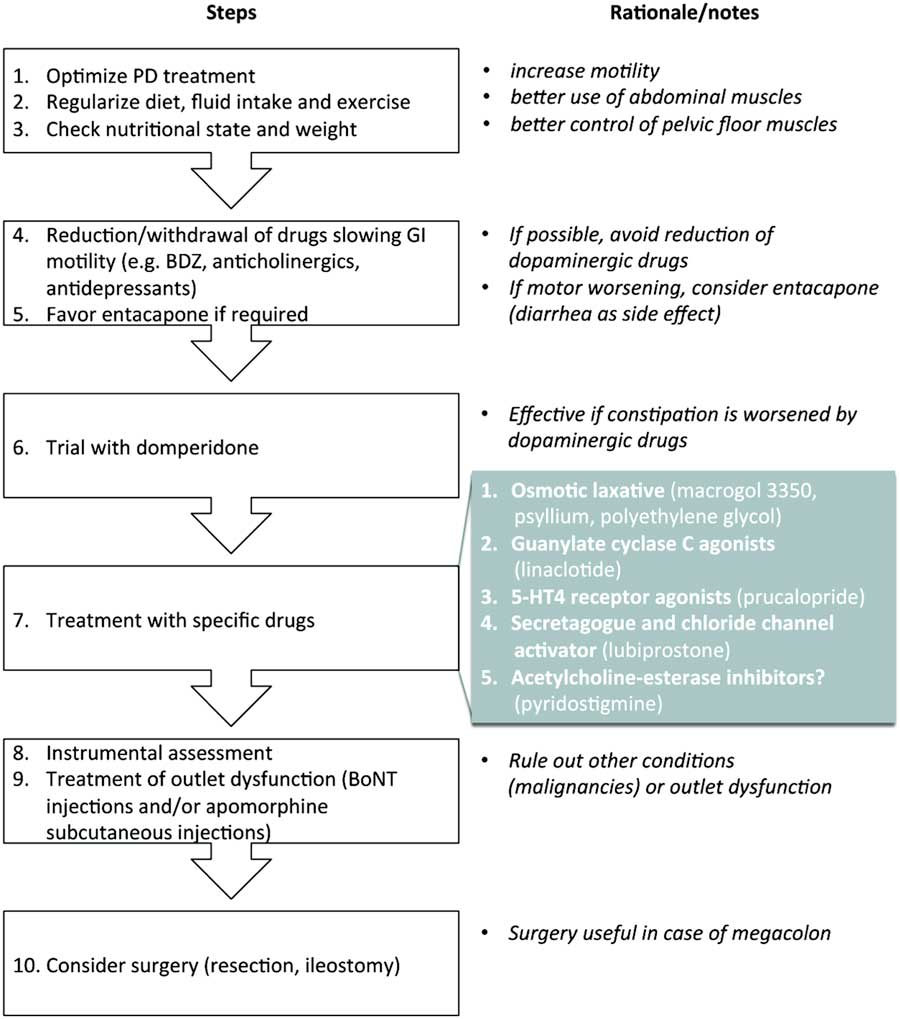
- Any other symptoms occur, such as constipation, sexual problems, or incontinence.
- You have symptoms of depression, such as feeling sad or losing interest in daily activities.
- You or your family notice that you have problems with memory and thinking ability.
Recommended Reading: Parkinson’s And Memory Loss
When Should I See My Healthcare Provider Or When Should I Seek Care
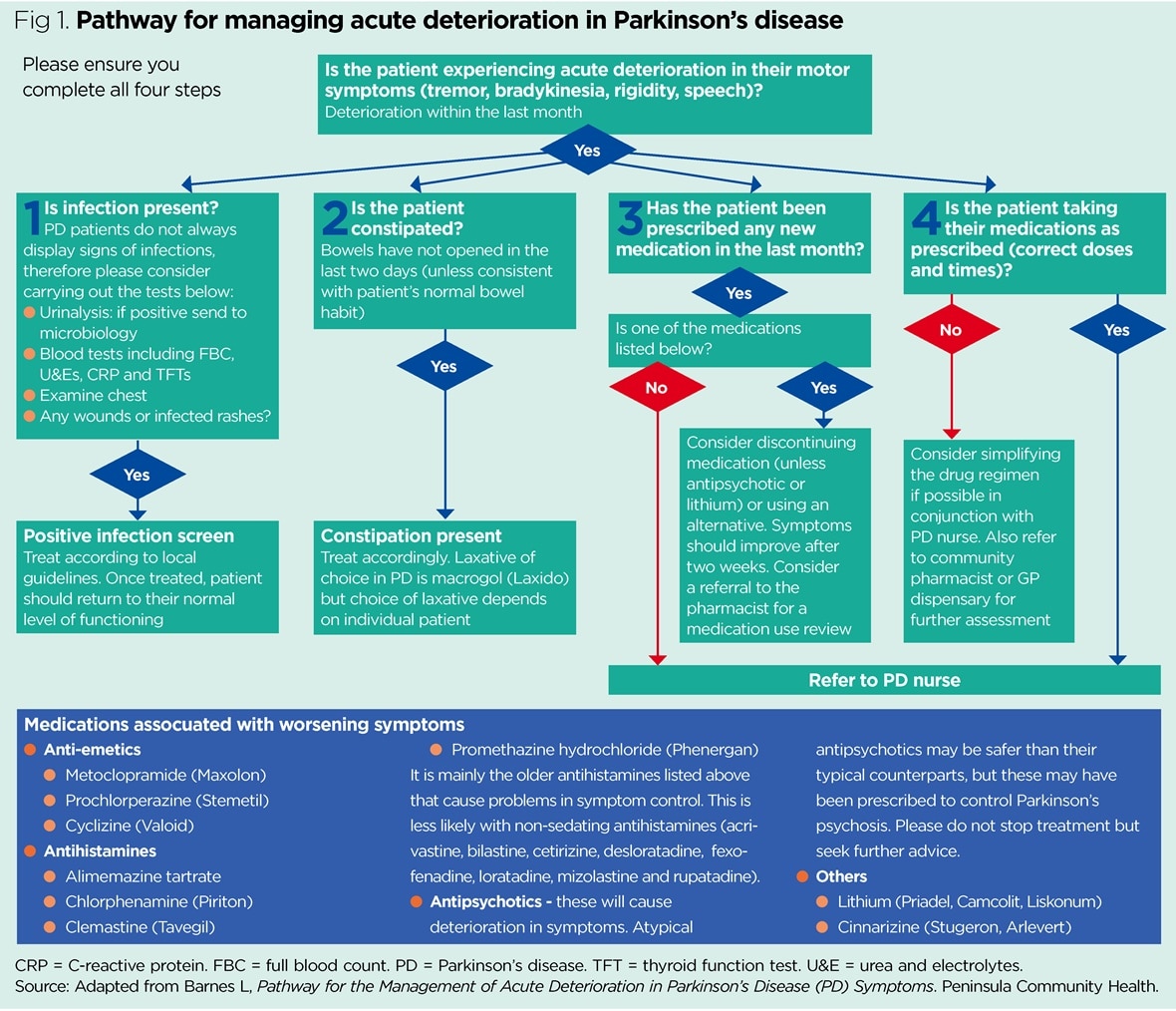
You should see your healthcare provider as recommended, or if you notice changes in your symptoms or the effectiveness of your medication. Adjustments to medications and dosages can make a huge difference in how Parkinsons affects your life.
When should I go to ER?
Your healthcare provider can give you guidance and information on signs or symptoms that mean you should go to the hospital or seek medical care. In general, you should seek care if you fall, especially when you lose consciousness or might have an injury to your head, neck, chest, back or abdomen.
Broad Street Can Help
If you or a family member is struggling with the limitations imposed by Alzheimers disease or Dementia, its time to arrange for the support you need.
Broad Street Home Care offers a wide range of services from personal care and companionship to Alzheimers and Dementia long-term care in Chicago.
If you would prefer to speak with us directly, please call
Read Also: Eyesight And Parkinson’s Disease
Dry Eyes Are A Commonly Reported Symptom Of Pd
Vision changes can be caused by a number of factors. Reasons behind dry eyes or blurry vision can include “hormone changes, autoimmune disease, inflamed eyelid glands or allergic eye disease,” says the Mayo Clinic. Other times, your eyes are sending a warning signal about a more serious condition. Vision changes can be a symptom of eye cancer, early-onset dementia, or PD, among other conditions.
“Dry eye disease , which occurs when the eyes are not sufficiently moistened by tears, can lead to chronically dry eyes that cause discomfort and risk vision loss, significantly disrupting daily life,” reports Parkinsons News Today, noting that a recent study found the estimated occurrance of DED in Parkinson’s patients is between 53 percent and 60 percent.
“Some people with Parkinson’s report that their vision loses sharpness as their disease progresses,” advises the Parkinson’s Foundation. “Difficulties related to the eyes and vision often progress alongside other PD symptoms.”
Dry eyes can occur because of decreased blinking, which can also result in blurry vision. Other changes in eyesight include double vision, trouble with reading, and rouble voluntarily opening the eyes, known as apraxia, the Parkinson’s Foundation explains.
If you’re experiencing dry eyes, check with your healthcare provider about whether you should be screened for PD.
Can Parkinsons Disease Be Cured
No, Parkinsons disease is not curable. However, it is treatable, and many treatments are highly effective. It might also be possible to delay the progress and more severe symptoms of the disease.
A note from Cleveland Clinic
Parkinsons disease is a very common condition, and it is more likely to happen to people as they get older. While Parkinsons isnt curable, there are many different ways to treat this condition. They include several different classes of medications, surgery to implant brain-stimulation devices and more. Thanks to advances in treatment and care, many can live for years or even decades with this condition and can adapt to or receive treatment for the effects and symptoms.
Also Check: Parkinson’s And The Brain
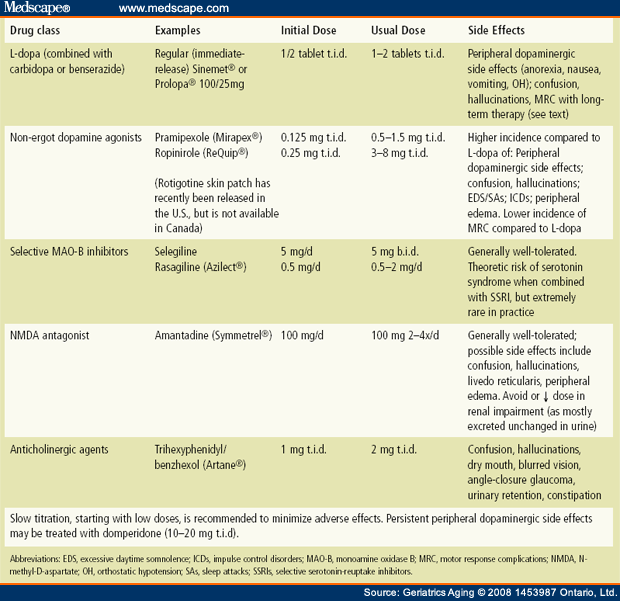
When Should I Start Taking Medication
If you have been diagnosed with Parkinsons, you may be wondering when you should start treatment and with what medication. There is no single strategy that applies to everyone. The timing will differ from person to person. It depends on a variety of factors, such as:
- the nature of your symptom
- your overall physical health
- whether you experience balance problems with walking
- changes in intellectual abilities, and
- your own attitude toward taking medication
When to start taking medication can be decided in consultation with your neurologist or movement disorder specialist. The decision to delay taking medication requires close monitoring and evaluation for risks of falls and injuries, especially if you are older. The older you are, the more you are at risk for a fall, and Parkinsons medication, when used appropriately, may reduce this risk.
Basics Of Parkinsons Disease
Parkinsons disease , or paralysis agitans, is a common neurodegenerative condition, which typically develops between the ages of 55 and 65 years. This disease was first named and described by James Parkinson in 1817. The progression of this disease is gradual and prolonged. It has a plausible familial incidence, although the estimates of these occurrences are low and usually sporadic. This disease is organized into two classifications: genetic and sporadic. Genetic PD follows Mendelian inheritance. Sporadic PD, which accounts for about 90% of all Parkinsons cases, is a more complex category in which the pathogenic mechanisms that underlie it are not yet fully understood. Nonetheless, it is known that the byzantine interactions of genetic and environmental influences play roles in the determination of sporadic PD. Several subtypes of PD exist. Each has its own set of causative factors and susceptibilities, pathology, and treatment courses. General risk factors, symptoms, and pathology will be discussed first, before addressing some of the subtypes.
Also Check: What Happens To You When You Have Parkinson’s Disease
Management Of Parkinsons Disease
Overall treatment is specific to the patient and the symptoms they experience. Symptoms can be variable from day to day or even hour to hour therefore, it is important that patients have a good understanding of their treatment, disease, coping mechanism, support system and regular reviews. Life expectancy can be normal however, more advanced symptoms can lead to increased disability and poor health, which may make someone more vulnerable to complications .
When To Start Treatment
Deciding when to start drug therapy for Parkinsons disease should be individually tailored to a patients symptoms, circumstances and comorbidities. Treatment is indicated when symptoms impact on quality of life. When treatment is needed there is no evidence to support undue delay because of concerns about levodopa toxicity or the development of treatment resistance.3 The aim is to control symptoms and maintain an on state.
Some drugs with good symptomatic benefit are speculated to have a role in neuroprotection and some specialists advocate their use from the time of diagnosis.4 Delayed start trials have been used to try and differentiate symptomatic from disease-modifying effects. A recent delayed start study of rasagiline, a monoamine oxidase B inhibitor, in treatment-naïve patients with mild Parkinsons disease showed a small benefit in the low-dose treatment group. This was not seen with the 2 mg dose and a clear explanation for this has not been established.5 Further studies are needed before such treatments are considered truly disease modifying. Until a drug is unequivocally proven to slow disease progression, the time to commence treatment will remain contentious.
Don’t Miss: How Much Does It Cost To Treat Parkinson Disease
Medication Guidelines For Parkinson’s Disease
There is no one best mix of Parkinsonâs medicines. You and your doctor will have to try a few treatment approaches to figure out the best one for you.
But there are some general guidelines for taking your medication. Be sure to ask your doctor or pharmacist for any specific tips for your treatment.
Full Financial Disclosures For The Last 12 Months
Alessandra Fanciulli: Dr. Fanciulli reports royalties from Springer Nature Publishing Group, speaker fees and honoraria from the Austrian Autonomic Society, Austrian Parkinson Society, Ordensklinikum Linz, International Parkinson Disease and Movement Disorders Society and Theravance Biopharma and research grants from the Stichting ParkinsonFond and the Österreichischer Austausch Dienst, outside of the submitted work.
Fabian Leys: Dr. Leys reports no disclosures.
Cristian Falup-Pecurariu: Dr. Falup-Pecurariu reports royalties from Springer Nature Publishing Group, speaker fees and honoraria from the International Parkinson and Movement Disorders Society, outside of the submitted work.
Roland Thijs: Dr. Thijs reports speaker fees from Novartis, consultancy fees from Theravance Biopharma and research support from the Dutch Epilepsy Foundation Dutch, the Netherlands Organization for Health Research and Development and De Christelijke Vereniging voor de Verpleging van Lijders aan Epilepsie, outside of the submitted work.
Gregor K. Wenning: Dr. Wenning reports consultancy fees from Biogen, Biohaven, Lundbeck, Minoryx, Takeda, Theravance and research support from the Austrian Science Fund, International Parkinson Disease and Movement Disorders Society and the Medical University Innsbruck, outside of the submitted work.
Recommended Reading: Tao Patch For Parkinson’s
Prevalence Incidence And Risk Factors For Motor Complications
Nearly all patients develop motor fluctuations and LID by 15 to 20 years from time of diagnosis . However, prevalence and incidence figures through the course of PD vary depending on the study methodology employed and by the predominant treatment strategies of the time. Early literature suggested that approximately 10% of patients per year following initiation of treatment with levodopa develop motor fluctuations, with 40% of patients developing these complications within 46 years of treatment . A large cross-sectional study of 617 patients with PD found an overall prevalence of wearing off of 57% as assessed by neurologists and 67% as assessed by a patient-completed questionnaire . Of patients with disease duration < 2.5 years, wearing off was identified in 41.8% by the WOQ-19 and in 21.8% by neurologists, indicating that motor fluctuations can emerge as early as several months to a few years after the initiation of levodopa, as has also been observed in other studies . A retrospective analysis of an incident cohort of PD found estimated rates of dyskinesia of 30% by 5 treatment years and 59% by 10 treatment years .
Struthers Parkinsons Care Network
In 2016, Broad Street partnered with the Struthers Parkinsons Care Network which was instrumental in the development of our training curriculum. The Struthers team coordinates a network of care organizations across the country facilitating a method of communicating successes and struggles encountered in the delivery of care.
We continue to collaborate with The Struthers Parkinsons Care Network to ensure that we are delivering the most effective training and utilizing the best practices available in support of our clients.
Don’t Miss: How Long Can A Parkinson Patient Live
Associated Clinical Features Of Probable Pdd
Associated clinical features are defined along four primary cognitive domains and a spectrum of behavioural disorders . The MDS Task Force recommended a number of tests from which the clinician could choose to assess the four primary cognitive domains and suggested that the four-item Neuropsychiatric Inventory, which covers hallucinations, depression, delusions and apathy, might be useful in assessing behavioural symptoms associated with PDD . A diagnosis of probable PDD is made on the basis of a typical profile of cognitive deficits . If dementia exists in the presence of established PD, yet the associated clinical features are not considered typical , only possible PDD should be diagnosed.
| Find sources:Dietary management of Parkinsons diseasenews·newspapers·books·scholar·JSTOR |
Parkinsons disease is the 2nd most prevalent neurological disorder within the United States and Europe, affecting around 1% of the population over the age of 60. While the link connecting the onset of Parkinsons disease to environmental factors is known, the link between dietary patterns and the disease is just beginning to be researched more fully. Additionally, other research has sought to examine the symptoms of the disease and propose methods on how to alleviate these symptoms through changes in diet. Current medications that work to alleviate the symptoms of Parkinsons disease can also be made more effective through changes in diet.
How Broad Street Develops Our Alzheimers Or Dementia Specialty Home Care
As with all specializations, we start with education and training. Our services go beyond just Personal Care and Companionship.
Alzheimers and Dementia are cognitive conditions where the brain often loses the ability to effectively connect between short term and long-term memory.
It may start with not remembering an appointment, or where keys were placed to eventually not remembering even the face of a loved one. This can cause frustration and depression which can even lead to behavioral issues.
If we understand the root of these cognitive impairments, we learn that the seemingly abnormal responses of clients with Alzheimers and Dementia are actually genuine.
This understanding, combined with training techniques including acknowledging and redirecting, along with things as simple as a warm smile and gentle touch, can help manage the frustration of these difficult symptoms.
Recommended Reading: Parkinson’s And Dementia Link
Dopaminergic Pathways For Pain Relief
Glutamate is the main excitatory neurotransmitter in the brain . Glutamatergic conduction is closely related to the sensitivity of the central nervous system, which can produce hypersensitive responses to harmful or non-harmful information. Exercise improves dopamine transmission and affects glutamate transmission and availability, thereby improving basal ganglia function .
Canadian Guideline For Parkinson Disease
See related article at www.cmaj.ca/lookup/doi/10.1503/cmaj.191089
Parkinson disease is chronic and progressive in nature, decreasing the quality of life for both patients with the disease and their caregivers and placing an onerous economic burden on society.1
The first Canadian guideline on Parkinson disease was published in 2012.2 Since that guideline, there have been substantial advances in the literature on the disease, particularly with respect to diagnostic criteria and treatment options. Parkinson Canada undertook to update the existing guideline to reflect these advances, as well as to add information on palliative care.
Also Check: What Are Off Episodes In Parkinson’s
Assembling Your Care Team
Assembling a team that will provide you with physical and emotional support and adapt to your needs over time is one of the best ways to remain healthy. Parkinsons disease is complex and requires an interdisciplinary approach to care. The care team may include, but is not limited to:
- Movement disorder specialist
- Rehabilitation specialists including physical, occupational, and speech therapists
How Soon After Treatment Will I Feel Better And How Long Will It Take To Recover
The time it takes to recover and see the effects of Parkinsons disease treatments depends strongly on the type of treatments, the severity of the condition and other factors. Your healthcare provider is the best person to offer more information about what you can expect from treatment. The information they give you can consider any unique factors that might affect what you experience.
Also Check: Parkinsons Tips And Tricks
Also Check: What Helps With Parkinson’s Nausea
Managing The Social And Emotional Impact
The effects of PD are broad and impact on the social and economic life of the person and their family from the time of diagnosis in a variety of ways.
Coping and adjusting to the diagnosis, facing increasing challenges at work and planning for the future can be a daunting undertaking.
Navigating this newfound uncertainty requires careful consideration and appropriate specialised support.
As the disorder progresses, caregiver burden also increases and quality of life can decrease.
A social worker specialised in movement disorders such as PD can assist the person with PD, their caregiver and family negotiate the challenges faced across the life time of the persons PD.
Social workers are highly skilled professionals who can assist you and your loved ones by:
- providing a range of different therapys like counselling
- assistance with linking to other support services
- directing you to financial support services
- information provision of entitlements for care packages
- help to facilitate suitable respite arrangements for the caregiver
- assistance and support with navigating the pathway to permanent residential care if the need arises.
After receiving a diagnosis of PD it is normal to experience a change in mood. A social worker has the appropriate specialised skills to help you deal with the reaction to your diagnosis.
Social workers are specifically trained to support you in understanding how best to manage such symptoms.