How Is Parkinsons Managed
There is currently no cure for Parkinsons but there are medications and therapies that can help to manage Parkinsons symptoms.
Medicines that increase the level of dopamine in the brain are the main treatment used to manage the symptoms of Parkinsons. Medicines are tailored to each individuals needs.
Symptoms will get worse when someones Parkinsons medicines are wearing off and improve again after Parkinsons medicines are taken. If people with Parkinsons dont get their medication at the right time, it leads to their motor symptoms becoming uncontrolled. It can take some time to get their symptoms under control again. If you work in a hospital or care home, it is important to be aware that medicine timings will vary from person to person and may be different to ward medicine rounds.
As well as medicines, surgical options are available for some people with Parkinsons, depending on their symptoms.
Treatments can help to manage the symptoms, but may become less effective in the later stages of the condition.
Parkinsons UK has more information on how Parkinsons affects people and how it can be managed.
South Nj Hospice Care For Parkinsons Disease Patients
Parkinsons disease is a progressive nervous system disorder that affects movement and, according to the Parkinsons Foundation, nearly one million people in the U.S. are living with it.
While ultimately the severity of Parkinsons differs from person to person due to the diversity of the disease, living with end-stage Parkinsons disease can be difficult. You may suffer from an increased severity in falling, freezing, and stiffness. There may be an increased need for a wheelchair or you are bedridden with severe posture issues. In these cases, hospice care for Parkinsons disease may be your best option.
Where Can I Find Support If I Have Parkinson’s Disease And Want To Exercise
You can find exercise support in your community. For example, many gyms and community centers offer seated exercise classes for people who struggle with balance. Ask your healthcare provider for ideas if you have Parkinsons disease and want to exercise.
A note from Cleveland Clinic
Exercise is an important part of managing Parkinsons disease. Talk to your healthcare provider about your exercise program and choose activities you enjoy so you stay motivated to get up and move every day.
Last reviewed by a Cleveland Clinic medical professional on 04/08/2021.
References
Recommended Reading: Foods Not To Eat With Parkinson’s Disease
Can I Afford Hospice Care
Medicare pays for hospice services under the Medicare Hospice Benefit. Under this benefit all care, medications and medical supplies related to the hospice diagnosis are completely covered. The benefit allows for months of care not just during the last weeks of life.
Medicaid and most private insurances also have a hospice benefit that covers costs. For patients not receiving Medicare, Medicaid or private insurance benefits, Lower Cape Fear LifeCare never refuses care based on someones ability to pay.
Caring For A Person With Advanced Parkinsons Disease

In this 47-minute webinar Anne Wallis, Associate Director of Education at the Parkinsons Foundation, talks with doctor of physical therapy, Sarah King, about when to look for outside help, how to lasso the power of your friends and family , and how to build an allied healthcare team that decreases your stress and improves your loved ones care.
You May Like: What Are Some Symptoms Of Parkinson’s Disease
Thank You To The Ontario Trillium Foundation
We would like to thank the Ontario Trillium Foundation for their support of Evergreen Hospice through their Resilient Communities Fund. This fund is supporting Evergreen to make changes to be able to open our offices safely post-pandemic helping us with the impacts of COVID-19 so we can continue to effectively meet the needs of our community. Thank you Ontario Trillium Foundation!
What Is The Prognosis And Life Expectancy For Parkinsons Disease
The severity of Parkinsons disease symptoms and signs vary greatly from person to person, and it is not possible to predict how quickly the disease will progress.
- Parkinsons disease itself is not a fatal disease, and the average life expectancy is similar to that of people without the disease.
- Secondary complications, such as pneumonia, falling-related injuries, and choking can lead to death.
- Many treatment options can reduce some of the symptoms and prolong the quality of life.
Read Also: Parkinsons Foundation Kansas City
Also Check: Parkinson’s Disease And Foot Pain
What Can I Expect If I Have This Condition
Parkinsons disease is a degenerative condition, meaning the effects on your brain get worse over time. However, this condition usually takes time to get worse. Most people have a normal life span with this condition.
Youll need little to no help in the earlier stages and can keep living independently. As the effects worsen, youll need medication to limit how the symptoms affect you. Most medications, especially levodopa, are moderately or even very effective once your provider finds the minimum dose you need to treat your symptoms.
Most of the effects and symptoms are manageable with treatment, but the treatments become less effective and more complicated over time. Living independently will also become more and more difficult as the disease worsens.
How long does Parkinsons disease last?
Parkinsons disease isnt curable, which means its a permanent, life-long condition.
Whats the outlook for Parkinsons disease?
Parkinsons disease isnt fatal, but the symptoms and effects are often contributing factors to death. The average life expectancy for Parkinsons disease in 1967 was a little under 10 years. Since then, the average life expectancy has increased by about 55%, rising to more than 14.5 years. That, combined with the fact that Parkinsons diagnosis is much more likely after age 60, means this condition doesnt often affect your life expectancy by more than a few years .
Hospice And Palliative Care Support Where You Need It
When it comes to end-of-life care, a little assistance can go a long way. A caregiver from Oasis Hospice can assist loved ones once curative treatment is no longer viable. We work in tandem with hospice organisations and home health agencies to provide continuous, one-on-one care in a variety of settings, including inpatient hospice facilities, hospitals, assisted living facilities, skilled nursing facilities, and at home. Our compassionate caregivers enhance quality of life and dignity in death while providing peace of mind and respite to your loved ones.
We strive to improve your loved ones quality of life by keeping them as comfortable, aware, and functional as possible. Our mission is to bring peace, comfort, and dignity to the people. Our 24-hour care serves to meet the unique requirements of persons reaching the end of life in a variety of ways, including:
- Serving as an emotional support system
- Mediating depression
- Preventing a sense of abandonment with one-to-one companionship and support
- Offering respite for family members
Contact one of our Client Care Managers today to learn more about our hospice services.
Recommended Reading: What Is The Difference Between Tremors And Parkinson’s Disease
What Type Of Exercise Should I Do If I Have Parkinson’s Disease
Exercise is a planned, structured, repetitive activity that is intended to improve physical fitness. There is no right exercise for people with Parkinsons. Everyones regimen will differ, depending on overall health, symptoms and previous level of activity. Any exercise helps, and a variety of exercise types may provide well-rounded benefits.
Aerobic exercise
Aerobic exercise involves activities that challenge your cardiorespiratory system such as walking, biking, running, and activities in the pool. Participating in aerobic exercise at least three days a week for 30-40 minutes may slow Parkinsons decline.
Strength training
Strength training involves using your body weight or other tools to build muscle mass and strength. Strength training two days per week, starting with low repetition and weight, may be beneficial in Parkinsons disease. A focus on extensor muscles, or muscles in the back of the body, can help with posture.
Flexibility training
Stretching two or more days per week can be beneficial to maintain range of motion and posture. Holding each stretch of major muscle groups for 30 to 60 seconds can improve muscle length.
Balance and agility training
This type of training often combines aerobic exercise, strength training, and flexibility training. Examples include:
- Tai chi, yoga or Pilates.
Palliative Care In Parkinson’s Disease
In the absence of any curative treatment, the principles of palliative care should be applied throughout the course of the disease and not limited to the terminal end-of-life period. This chapter defines palliative care and discusses the palliative phase of Parkinson’s disease, palliative carers, care homes, social costs, withdrawl of drugs, pressure ulsers, end-of-life issues, recommendations and ethical issues.
Recommended Reading: Self Stabilizing Spoon For Parkinson’s Sufferers
Motor Symptoms And Global Disability
Motor symptoms, as measured using the Unified Parkinsons Disease Rating Scale , Hoehn and Yahr Scale and the Progressive Supranuclear Palsy Rating Scale , were significant predictors of mortality in patients with PDRD. Beyer et al found higher mean UPDRS scores, 65 versus 42 , suggesting that greater motor impairment predicted death. Studies with median follow-up times ranging from 4 to 8 years estimated the association of 10-unit increases in baseline motor UPDRS Score on mortality and found statistically significant increased HRs for mortality of 1.17 up to 1.4 for each 10-unit increase in UPDRS Score. Baseline H& Y staging was significantly higher among those who died ) compared with those who survived ). Posada et al went further by splitting H& Y into early and later progression stages at baseline as a predictor for mortality and found that HRs increased by stage, from 1.5 for H& Y stages 1 and 2 to 2.3 for H& Y stages 35, both compared with patients with no PD and after controlling for comorbidities and demographic characteristics. Oosterveld et al stratified UPDRS total motor scores by greater than or equal to 30 compared with less than 30 and found an HR of 1.63 . Chiu et al compared the association of PSPRS scores on mortality and found increased HRs of 1.96 for 3548 on the PSPRS, 2.99 for 4862 and 8.55 for greater than 62 when compared with scores of 034.
Disease Burden And Mortality In Pd
PD is a slowly progressive multi-system neurodegenerative disorder, mainly affecting patients in later years of life . It is the second most common neurodegenerative disease worldwide, with its incidence and prevalence on the rise along with aging of the population .
The characteristic classical motor features of PD include bradykinesia, rigidity, resting tremor and postural instability. Patients with PD also suffered from multiple non-motor features including olfactory dysfunction, cognitive impairment, psychiatric symptoms, sleep disorders, autonomic dysfunction, pain and fatigue . As the disease progresses, both motor and non-motor symptoms become prominent and treatment-resistant. Advanced PD is identified by disability requiring help for the activities of daily living, presence of motor fluctuations with limitations to perform basic activities of daily living without help, severe dysphagia, recurrent falls, and dementia . Up to now there are no disease-modifying treatments that can stop or delay the disease process or mortality.
Also Check: L Tyrosine For Parkinson’s
Managing Advanced Parkinsons Disease
Module 13 of a continuing education course on Parkinsons disease for health care professionals outlines the complications of advanced of Parkinsons disease. Topics covered include medication issues, motor issues, nonmotor complications, sleep disorders, orthostatic hypotension, severe dysphagia, gastric dysfunction, constipation and urinary problems, managing falls, malnutrition and dehydration, impaired communication and the benefit of palliative care and hospice at home over nursing home care.
Free Inhome Consultation From Oasis Hospice
If you or a loved one suffers from Parkinsons disease and requires assistance at home, please contact Oasis Hospice Home Care. We will conduct a free in-home evaluation to determine your loved ones care needs and develop an appropriate care plan. For more information about our Parkinsons care services in Chicagoland, Wheaton, Glen Ellyn, Illinois, and the surrounding locations in DuPage county, call 941-4838.
Recommended Reading: Why Does Parkinson’s Disease Kill You
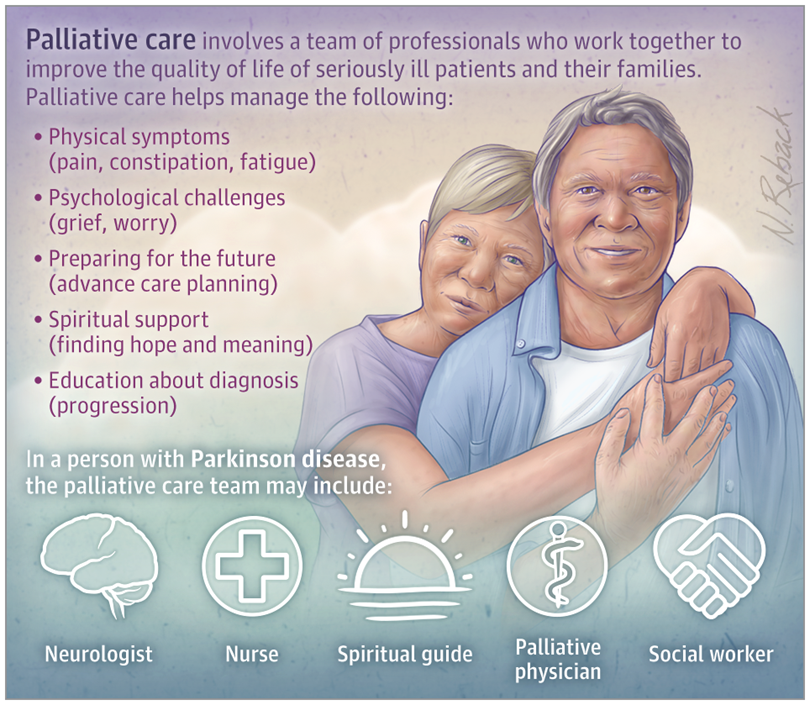
What Is Palliative Care For Parkinsons
Palliative care is a specialized type of support program for people with complex progressive and chronic conditions such as Parkinsons disease.
Palliative care programs are provided by a team of doctors, nurses, physical therapists, and other medical professionals. The team focuses on goals such as:
- minimizing pain
- providing emotional and mental health support
- educating patients and their families about conditions
- setting future goals
- monitoring patients through the years as conditions progress
Palliative care provides additional support for people with Parkinsons disease. It doesnt replace your regular doctors and therapists, and you wont need to stop any treatments or therapies you currently receive.
Palliative care programs can stay with you through the years. Doctors from your palliative care team can communicate with your regular doctor and other members of your broader medical team if needed.
Study Designs And Descriptions Of Included Studies
The 42 studies were published until February 2020. The study designs were: retrospective cohort studies, prospective cohort and longitudinal studies, casecontrol studies and cross-sectional studies. Predictors of mortality included demographic and clinical markers, medical events, medication changes, disease-specific symptoms and patient and caregivers ratings of health-related quality of life. Eight studies described both predictors of mortality and causes of death.
Don’t Miss: Early Parkinson’s Symptoms In Young Adults
Relevance Of Palliative Care To Parkinson Disease
The World Health Organization defines palliative care asan approach that improves the quality of life of patients and families facing life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual.1 Advances in PC relevant to Parkinson disease include the following: recognition that PC needs may emerge at any point of an illness, including at the time of initial diagnosis PC may be effectively delivered in diverse settings including outpatient clinics PC may be integrated into standard disease-focused therapies and PC may be delivered by clinicians not specializing in PC, so-called primary PC.2,3
Despite significant morbidity and mortality , there are many areas where persons living with PD have unmet PC needs under current models of care. Patients report that receiving the diagnosis of PD is traumatic and frequently given without acknowledging psychosocial consequences.5 Nonmotor symptoms such as pain and depression are under-treated, and other psychosocial issues such as caregiver support are rarely addressed.6,7 Most patients with PD do not receive hospice care and most of then die in hospitals or other institutions.8,9
How Can Hospice Help Your Loved One In The Final Stages Of Parkinsons Disease
Hospice care is an extra layer of support to help you care for your loved one with end-stage Parkinsons disease. It is a special kind of care that provides comfort, support, and dignity at the end of life.
The comprehensive program focuses on physical, emotional, and spiritual quality of life through the help of a team of experts. The team includes a board-certified physician, nurse, social worker, certified home health aide , spiritual support counselor, and volunteer.
The nurse will explain the prognosis and what to expect in the upcoming days or weeks. They will also monitor pain and other symptoms. The CHHA helps with personal care needs like bathing and changing bed linens. The social worker helps address social, emotional and practical challenges including complex and inter-related needs. The spiritual support counselor helps explore spiritual concerns.
Most importantly, the hospice team will be there for you during this difficult time, bringing you peace of mind. The team is on call 24 hours a day even at 2:00 am.
Hospice is about making your final months and weeks as good as possible. This means focusing on what really matters to you.
You May Like: Earliest Symptoms Of Parkinson’s Disease
Providing Diagnosis And Prognosis With Compassion
There are few events as significant to patients as receiving their PD diagnosis.15 Although physicians may choose to focus on the relatively positive aspects of this diagnosis, namely that medical and other therapies can significantly improve many symptoms, they should not underestimate the potential impact of this diagnosis on patients and their families. Physicians can improve the experience by responding empathetically to emotional reactions, sharing information, and listening to the patients hopes and expectations. Clinicians should provide adequate time for these conversations and anticipate a need for close follow-up to prevent feelings of confusion and abandonment. Consider these communication approaches:
- SPIKES mnemonic for important conversations: Setting up the Interview Assessing patients Perception Obtaining patients Invitation Giving Knowledge Addressing Emotions Strategy and Summary.16
- Within this mnemonic the authors highlight a few points. When getting an Invitation, be prepared for patients and their caregivers to have different desires for how much information they want. For Knowledge, it is important to let patients know how the diagnosis is made but not to overwhelm them. For the Summary step, the authors recommend having an opportunity for follow-up within a few weeks, as patients and families may need time to process this information and may not hear everything that is said at the first visit.
When Your Loved One Is Fighting Cancer

Oasis Hospice makes life easier for cancer patients when they are in the hospital or recovering at home. We have a large number of qualified carers on hand right now. Oncology patients benefit from caregiving at home because it gives aid, rest, and improves their attitude. Our skilled caregivers prepare meals, assist with light housework, assist with washing, clothing, and personal hygiene, provide company, assist with exercise, and transport to and from doctors appointments or treatments. By minimising stress, weariness, and despair, caregivers may be able to aid recovery.
Our caregivers will also monitor and keep your loved one company during surgery, chemotherapy, or radiation treatments, as well as conduct errands or notify the charge nurse in an emergency. They also allow you or other family members to go home and relax, safe in the knowledge that your loved one will never be alone.
Don’t Miss: Effective Treatment For Parkinson’s Disease