Parkinson’s Disease And Palliative Care
This page outlines the decline of Parkinson’s disease and helps those coping with Parkinson’s understand what a palliative care team provides. There is a brief discussion of when and how to get palliative care, an online quiz to determine if palliative care is right for your family and a link to a palliative care provider search tool.
My Parkinsons Story: Advanced Parkinsons
This 10-minute video alternates between an interview with a man and his wife and his palliative care team, including a doctor, nurse, clerg and social worker. The man and his wife shares his experience with late stage Parkinsons. The palliative care team explains that their job is to support the best physical, emotional and spiritual wellbeing of the immediate family as well as help the family make end of life decisions.
What To Do With Deep Brain Stimulation At The End Of Life
Deep brain stimulation uses an Implantable Pulse Generator, usually placed in the infraclavicular area, connected to leads within the brain. There is a remote programmer, and also a charging unit in the case of a rechargeable device, which are given to the patient and their carer. It improves dyskinesias and also has a levodopa sparing effect.37
Deactivation of DBS may lead to increased symptom burden as mentioned in the section above and so awareness of features of PHS should be considered if there is failure at the end of life. Supportive treatment should be given if possible,38 and anticipation of symptoms of distress from rigidity and fever.
After death, deactivation of the device with the patients handheld programmer is required before removing the pulse generator and battery in the case of a cremation.
You May Like: Parkinson’s Online Chat Group
Preparing For End Of Life
Whether you are a person with Parkinson’s or a relative, friend or carer, thinking about the future now may help you feel more in control and confident about what lies ahead.
This section looks at the practical and emotional issues relating to Parkinson’s and the later stages of life.
This includes decisions you may need to make and the care you would like to have, and how to put your affairs in order. There is also advice and information for carers, close family and friends, including how to arrange a funeral and finding bereavement support.
Thinking about the future now, and discussing your wishes and preferences with the people in your life, may help you feel more in control and confident about what lies ahead.
It also takes away the burden from family or friends of having to make decisions on your behalf, should you become too ill to make decisions for yourself.
For the majority of people, Parkinson’s will not significantly affect their life expectancy. However, some of the more advanced symptoms can lead to increased disability and poor health, which can make someone more vulnerable to infection.
Parkinson’s is a progressive condition. This means it will get worse over time. Its difficult to predict at what speed your Parkinson’s will progress or what symptoms you may get, because the condition is different for everyone.
Your GP, Parkinson’s nurse or specialist should be able to advise on treatments to help with this, too.
This can mean:
Motor Symptoms And Global Disability
Motor symptoms, as measured using the Unified Parkinsons Disease Rating Scale , Hoehn and Yahr Scale and the Progressive Supranuclear Palsy Rating Scale , were significant predictors of mortality in patients with PDRD. Beyer et al found higher mean UPDRS scores, 65 versus 42 , suggesting that greater motor impairment predicted death. Studies with median follow-up times ranging from 4 to 8 years estimated the association of 10-unit increases in baseline motor UPDRS Score on mortality and found statistically significant increased HRs for mortality of 1.17 up to 1.4 for each 10-unit increase in UPDRS Score. Baseline H& Y staging was significantly higher among those who died ) compared with those who survived ). Posada et al went further by splitting H& Y into early and later progression stages at baseline as a predictor for mortality and found that HRs increased by stage, from 1.5 for H& Y stages 1 and 2 to 2.3 for H& Y stages 35, both compared with patients with no PD and after controlling for comorbidities and demographic characteristics. Oosterveld et al stratified UPDRS total motor scores by greater than or equal to 30 compared with less than 30 and found an HR of 1.63 . Chiu et al compared the association of PSPRS scores on mortality and found increased HRs of 1.96 for 3548 on the PSPRS, 2.99 for 4862 and 8.55 for greater than 62 when compared with scores of 034.
Also Check: How To Improve Parkinson’s Gait
How To Manage Symptoms At The End Of Life
At the end of life, good practice is to plan for any potential symptoms that may arise. The most common symptoms anticipated are pain, dyspnoea, nausea and vomiting, agitation, anxiety, delirium and noisy respiratory secretions.18 For patients with PD particular considerations should be given to the more commonly used medicines, specifically anticholinergics and antidopaminergics. These are usually prescribed for treatment of respiratory secretions and nausea and vomiting. Alternatives are available for respiratory secretions, and include glycopyrronium, in preference to hyoscine hydrobromide. Although this is an anticholinergic, only a small proportion crosses the blood brain barrier.
For nausea and vomiting, ondansetron,19 cyclizine, domperidone have all been suggested in PD.20 However, ondansetron has been shown to be inferior to domperidone in the pre-treatment of apomorphine.21 Cyclizine has anticholinergic properties and may exacerbate confusion, especially when comorbid psychosis or cognitive impairment are present. Levomepromazine, although it has antidopaminergic effects, has been shown to be effective for nausea with rotigotine in a case report.22
Agitation, dyspnoea and pain can all be managed with the same anticipatory medications as recommended.20 Specifically relating to PD, several case reports have supported the intraoperative use of midazolam, during sedation, for tremor and dyskinesias,23,24 as well as for agitation at the end of life.20
Therapeutic Management Of Late
, December 12, 2011
This review of the Movement Disorder Societys guidelines for therapeutic management of late-stage Parkinsons applies the guidelines to a case scenario. The guidelines first appeared in the European Handbook of Neurological Management. This review cites the Annals of Long-Term Care: Clinical Care and Aging, 2011 19 : 42-46.
Recommended Reading: Late Stage Parkinson’s Disease Symptoms
Benefits Of Lower Cape Fear Lifecares Hospice Services
- Manages pain, symptoms and anxiety associated with end-stage Parkinsons to improve quality of life for the patient and their loved ones
- Provides emotional and spiritual care thereby providing a whole-body approach to care
- Provides clinical team support 24/7 nights, weekends, and holidays
- Provides education and support for family caregivers
- Arranges for additional medications, supplies and equipment associated with the hospice diagnosis to be delivered
- Coordinates care with all the patients healthcare providers
- Assists in documenting an advance healthcare plan
- Offers continuity of care if pain and symptoms cannot be managed in a residential setting in its home-like inpatient hospice care centers available exclusively to our patients
- Offers continued grief care and support for loved ones after death
Cold Hands And Feet And Skin Mottling
Hands and feet may become colder and the skin may look blotchy and purplish . It happens because the heart is no longer able to pump blood as well. As a result, blood pressure goes down and the skin grows colder.
This mottling may slowly work its way up the arms and legs. The lips and nail beds can turn blue or purple too.
Read Also: Best Cane For Parkinson’s
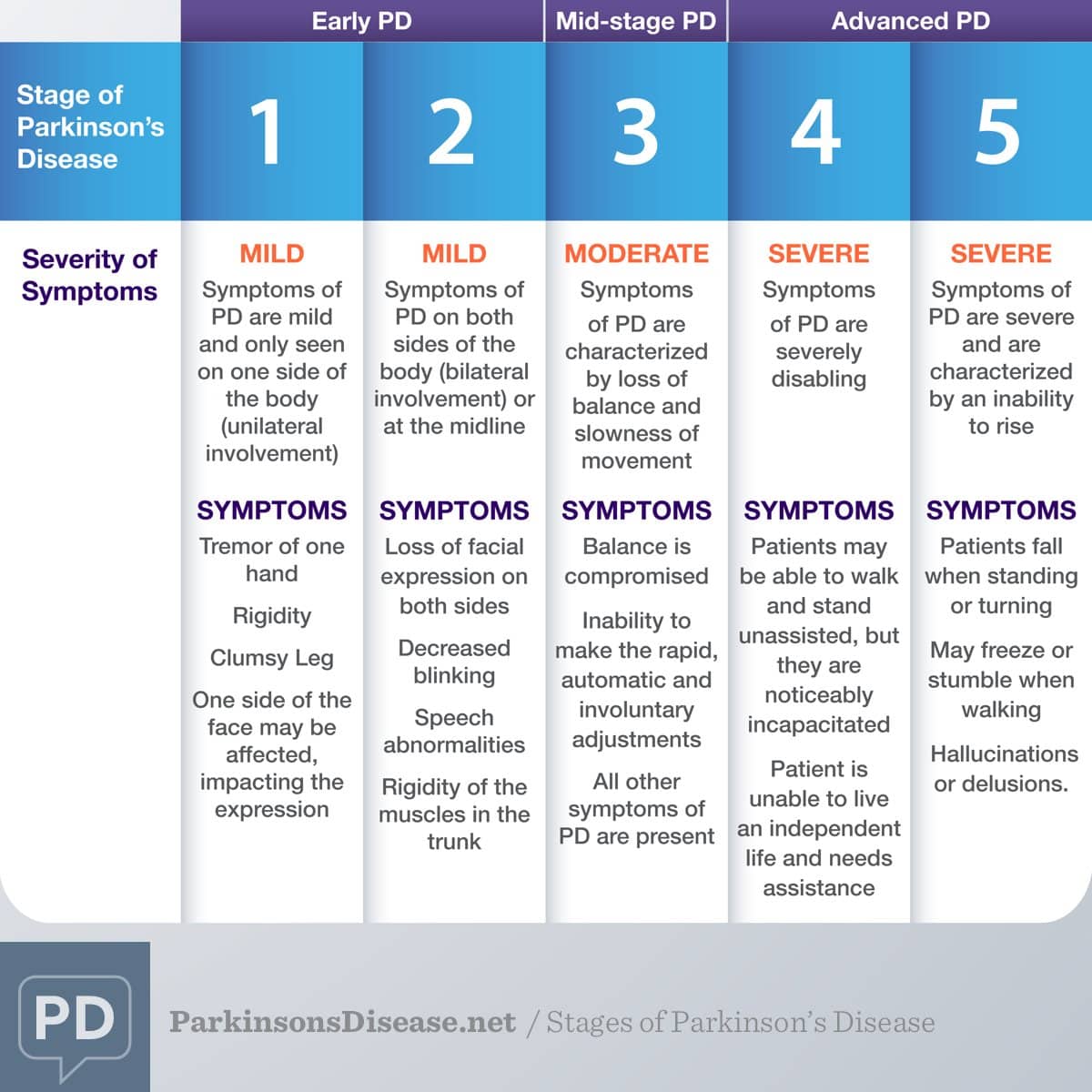
Stage Five Of Parkinsons Disease
Stage five is the most advanced and is characterized by an inability to rise from a chair or get out of bed without help, they may have a tendency to fall when standing or turning, and they may freeze or stumble when walking.
Around-the-clock assistance is required at this stage to reduce the risk of falling and help the patient with all daily activities. At stage five, the patient may also experience hallucinations or delusions.
While the symptoms worsen over time, it is worth noting that some patients with PD never reach stage five. Also, the length of time to progress through the different stages varies from individual to individual. Not all the symptoms may occur in one individual either. For example, one person may have a tremor but balance remains intact. In addition, there are treatments available that can help at every stage of the disease. However, the earlier the diagnosis, and the earlier the stage at which the disease is diagnosed, the more effective the treatment is at alleviating symptoms.
What Are The Important Points Regarding Duodopa At The End Of Life
Duodopa is a continuous infusion of dopaminergic medication administered as a gel into the gut, pumped via a percutaneously inserted gastrostomy tube . There is a requirement for care of the stoma and PEG tube together with functioning of the pump by the patient or carer.41 It reduces the time in motor off periods in advanced PD and quality of life.42 There is evidence of effective treatment up until death from within a case series.43
Don’t Miss: Diseases Related To Parkinson’s
What Are The Risks Of Not Receiving Any Dopaminergic Medication
There is the possibility of neuroleptic malignant-like syndrome , a life-threatening and distressing condition resulting in rigidity and fever, from withdrawal of therapy.31 This can also occur with sudden cessation of Deep Brain Stimulation .32,33,34 To reduce the risk of this, dopaminergic therapy at the end of life should be continued.27 It should also be noted that in a patient dying of another condition, whose PD is still responsive to dopaminergic medication, the cessation of this also risks aspiration pneumonia.35 Transdermal rotigotine can be used in patients in whom a NG tube may cause excessive distress or is not possible. The dose should be calculated with an accepted converter.36
Pharmacologic Issues At End

As PD progresses there are fewer dopaminergic neurons in the substantia nigra as well as a progressively lower capacity to store exogenous levodopa and convert it to dopamine for storage and release in the remaining neurons. Additionally, as the dose requirements of levodopa increase, the patients functioning is inhibited before his next dose of medication . This usually takes place 24 hours after a levodopa dose and may appear as sensory , psychiatric or autonomic symptom, or progression of motor symptoms or dystonia . This is called end of dose wearing off. Wearing off has not been fully explored, but may be connected to pharmacokinetic changes, and shortening of striatal levodopa half-life resulting from progressive degeneration of nigrostriatal dopaminergic terminals . To treat motor symptoms it is necessary to deliver medication effectively. Patients with advanced PD often notice that protein-rich meals will diminish the effectiveness of levodopa doses . This can be alleviated by reducing protein intake during daytime and limiting protein intake at night to 40 grams . There are some strategies to Improve absorption of Levodopa include: advise patients to take levodopa before meals, on an empty stomach , advise patients to avoid protein-rich meals and bulk-forming foods , advise patients against lying down, and encourage them to move around, after ingesting a dose , and advise patients to mix levodopa, crushed into a powder, into sparkling liquid .
You May Like: Loving Someone With Parkinson’s
Professionals Need For Training
A range of experiences from clinical practice in relation to limited competences and skills in working with persons with PD were described. Health care professionals found themselves at the stage of conscious incompetence . They recognized the deficit of not knowing how to offer palliative care or not knowing what skills are needed. It was suggested that additional training can help overcome these deficits. Training could also help in feeling more confident in using the knowledge and skills. But also in helping health care professionals to address issues related to death and dying. Some professionals felt reluctant because of their own personal issues, such as taboo, uncertainty or personal life experiences and beliefs. .
Spiritual care was much less actively discussed among health care professionals than the other domains of palliative care . A few health care professionals remarked that spirituality was addressed only if the person with PD explicitly raised spiritual issues and was not always a standard subject in care. When professionals were confronted with spiritual care, they frequently referred to or involved others. Health care professionals underpinned spiritual care as an important part of palliative care. However, the awareness for spiritual needs and how to respond or act as a professional remains unclear. Some suggested that it was not enough to develop training on this topic.
Burden And Demographic Disparities Of Ltnf In Pd
We identified 469,055 Medicare beneficiaries aged 65 years and older who had a diagnosis of PD recorded in the year 2002. Twenty-four percent had claims consistent with residence in an LTCF. Compared with community-dwelling patients with PD, LTCF residents with PD were older and more often female . These sex and age differences are similar to those found in the general LTCF population, which consists mostly of women and individuals aged 75 years and older .,
Studies have also reported that minorities are underrepresented in the general nursing home population, with black persons having 25% to 50% lower LTCF utilization rates than white persons., We found that African Americans with a PD diagnosis were relatively overrepresented in the LTCF population . Hispanic individuals were more common in the community PD population .
Also Check: Insomnia Parkinson’s Disease Treatment
Causes Of Parkinsons Disease
Parkinsons disease is caused by a loss of nerve cells in part of the brain called the substantia nigra. This leads to a reduction in a chemical called dopamine in the brain.
Dopamine plays a vital role in regulating the movement of the body. A reduction in dopamine is responsible for many of the symptoms of Parkinsons disease.
Exactly what causes the loss of nerve cells is unclear. Most experts think that a combination of genetic and environmental factors is responsible.
Hospice Eligibility For Parkinsons Disease
Due to the progressive nature of Parkinsons disease, it can be challenging for families to know when their loved one is eligible for the support of hospice care. If a loved one has been diagnosed with six months or less to live or if they have experienced a decline in their ability to move, speak, or participate in the activities of daily living without caregiver assistance, it is time to speak with a hospice professional about next steps.
Read Also: Struthers Parkinson’s Center Golden Valley
If You Live In South Jersey And Have Questions About The Final Stages Of Parkinsons Disease Or Hospice Care For Your Loved One Please Call Samaritan At 229
Samaritan is a member of the National Partnership for Healthcare and Hospice Innovation, a network of not-for-profit hospice and palliative providers across the country. If you know someone outside of our service area who is living with advanced illness and can benefit from hospice or palliative care, please call 1 -GET-NPHI for a referral to a not-for-profit provider in your area.
Management Of Social Care
When someone faces diagnosis and then the progression of a life limiting condition, many psychosocial issues will arise. These may include fears around diagnosis and an uncertainty about their future, with loss of independence and losing their role within the family. They may have anxieties about finances, about their independence and finally a fear of developing dementia.
Management of these changes both physical and mental will require early identification and an impeccable assessment with prompt referral to the appropriate team or professional.
The family and/or carers will require support from social services, carer support groups and Parkinsons support groups. Signposting to charities that provide support, education and guidance is also advisable.
Dont Miss: Symptoms Of Parkinson Disease Webmd
Don’t Miss: Wearable Technology For Parkinson Disease
What Is An Advance Decision To Refuse Treatment
During the course of an individuals advance care planning discussion they may indicate that they wish to make an advance decision to refuse certain treatments.
This is a separate document to that of the ACP and must be instigated by a professional who is competent in this process. They are required to follow the guidance available in the Code of Practice for the Mental Capacity Act on Advance Decision to Refuse Treatment in England, Wales and Northern Ireland. In Scotland professionals must follow guidance available in the Adults With Incapacity Act .
- An Advance Decision to Refuse Treatment allows the person who is 18 years of age or over to specify what treatments they would not want and would not consent to later in life. In Scotland the age of advanced directives is 16. They cannot demand certain treatments or refuse basic care, ie offers of food and water by mouth, warmth, shelter and hygiene. But clinically assisted nutrition and hydration given by intravenous, subcutaneous or gastroscopy are considered medical interventions and can be refused. These decisions can be withdrawn if the individual gains or retains capacity.
- All healthcare providers must respect the individuals advance decision and ensure it is incorporated into the person-centred care planning. They will also have discussed who is to be made aware of the ADRT and where they wish to store it in the home. A copy of the document should be stored in their healthcare notes and their GP made aware.
Palliative Care In Parkinson’s Disease
In the absence of any curative treatment, the principles of palliative care should be applied throughout the course of the disease and not limited to the terminal end-of-life period. This chapter defines palliative care and discusses the palliative phase of Parkinson’s disease, palliative carers, care homes, social costs, withdrawl of drugs, pressure ulsers, end-of-life issues, recommendations and ethical issues.
Read Also: Is Parkinson’s Life Threatening