Medicines For Parkinsons Disease
Medicines can help treat the symptoms of Parkinsons by:
- Increasing the level of dopamine in the brain
- Having an effect on other brain chemicals, such as neurotransmitters, which transfer information between brain cells
- Helping control non-movement symptoms
The main therapy for Parkinsons is levodopa. Nerve cells use levodopa to make dopamine to replenish the brains dwindling supply. Usually, people take levodopa along with another medication called carbidopa. Carbidopa prevents or reduces some of the side effects of levodopa therapy such as nausea, vomiting, low blood pressure, and restlessness and reduces the amount of levodopa needed to improve symptoms.
People living with Parkinsons disease should never stop taking levodopa without telling their doctor. Suddenly stopping the drug may have serious side effects, like being unable to move or having difficulty breathing.
The doctor may prescribe other medicines to treat Parkinsons symptoms, including:
- Dopamine agonists to stimulate the production of dopamine in the brain
- Enzyme inhibitors to increase the amount of dopamine by slowing down the enzymes that break down dopamine in the brain
- Amantadine to help reduce involuntary movements
- Anticholinergic drugs to reduce tremors and muscle rigidity
Diagnosis In Young Onset Parkinsons
Many young onset patients experience delay in diagnosis given the uncommon age and often different symptoms as outlined below. Similar to late onset patients, the diagnosis is made based on history and clinical examination. There are still no proven diagnostic tests that can definitively diagnose PD. In some cases, other mimics of Parkinsons need to be evaluated for given their increased likelihood in younger patients. Given the complexities, it is important to seek evaluation by a neurologist and in many cases a movement disorder specialist.
In addition, young onset patients are more likely to have a genetic risk factor or cause to their symptoms, especially if there is a family history. Genetic testing can be considered, but should always be done after consulting a physician and in many cases a genetic counselor.
What Is The Treatment For Parkinsons Disease
There is currently no treatment to cure Parkinsons disease. Several therapies are available to delay the onset of motor symptoms and to ameliorate motor symptoms. All of these therapies are designed to increase the amount of dopamine in the brain either by replacing dopamine, mimicking dopamine, or prolonging the effect of dopamine by inhibiting its breakdown. Studies have shown that early therapy in the non-motor stage can delay the onset of motor symptoms, thereby extending quality of life.
The most effective therapy for Parkinsons disease is levodopa , which is converted to dopamine in the brain. However, because long-term treatment with levodopa can lead to unpleasant side effects , its use is often delayed until motor impairment is more severe. Levodopa is frequently prescribed together with carbidopa , which prevents levodopa from being broken down before it reaches the brain. Co-treatment with carbidopa allows for a lower levodopa dose, thereby reducing side effects.
In earlier stages of Parkinsons disease, substances that mimic the action of dopamine , and substances that reduce the breakdown of dopamine inhibitors) can be very efficacious in relieving motor symptoms. Unpleasant side effects of these preparations are quite common, including swelling caused by fluid accumulation in body tissues, drowsiness, constipation, dizziness, hallucinations, and nausea.
Read Also: What Are The Side Effects Of Parkinson’s Disease
What Is The Main Cause Of Death In Parkinsons Disease Patients
Parkinsons is often referred to as a bespoke disease because it affects each patient differently. Another factor worth considering is that Parkinsons disease generally affects people in their 60s, most of whom die of unrelated conditions such as cancer, heart disease or stroke. However, the most common cause of death in those with Parkinsons disease is pneumonia. This is because the disease can impair your ability to swallow in the later stages, putting you at risk for aspirating food or liquid into the lungs.
Circumstances And Societal Engagement In Yopd And Implications For Management
In general, people with YOPD tend to have different family and societal engagements to those with late-onset PD. For example, most people diagnosed with YOPD will have a job, whereas some people with late-onset PD have already retired. Additionaly, it is not unusual that people with YOPD have young children , or may want to start a family.
Dont Miss: Similar To Parkinsons
You May Like: What Does Rasagiline Do For Parkinson’s
What Sets Young Onset Parkinsons Apart From A Diagnosis At An Older Age
Because the majority of people who get Parkinsons disease are over the age of 60, the disease is often overlooked in younger people, leading many to go undiagnosed or misdiagnosed for extended periods of time.
However, once it has been diagnosed, the rate of the diseases progression is usually much slower in younger than older people, due in part to the fact that younger people have fewer general health problems and are more capable during physical therapy treatment.
Symptoms of young onset Parkinsons disease
While common symptoms of Parkinsons may be similar no matter what age you are, the progression is often different:
- Young people often have more involuntary movement problems due to the most commonly prescribed Parkinsons disease medication, levodopa. For this reason, young onset patients are usually initially treated with alternatives to levodopa.
- Other problems associated with Parkinsons such as memory loss, confusion, and balance difficulties tend to be less frequent in young people with the disease.
Are There Doctors Who Specialize In Parkinsons Disease
Doctors who are specially trained to diagnose and treat conditions of the brain and nervous system are called neurologists. Some neurologists have a subspecialty in movement disorders and work extensively with patients who have Parkinsons disease and other similar conditions. These doctors also may have experience dealing with early onset Parkinsons symptoms. You can ask your physician if they have specific experience with younger patients, or whether they can refer you to a doctor who does.
Don’t Miss: What Does Carbidopa Levodopa Do For Parkinson’s
Eat Healthy Meals Throughout The Day
- Consuming a variety of foods from all five food groups provides consistent energy and keeps your immune system healthy. Focus on eating a minimum of five fruits and vegetables each day, eating a variety of high fiber foods, and staying hydrated, all of which help prevent constipation, which is often an issue for people diagnosed with YOPD.
- Watch this to learn how to use nutrition to help you live well with Parkinsons.
What Is The Prognosis For Someone With Early
One of the challenges of early-onset Parkinsons disease is that you will inevitably live longer with the condition, as Parkinsons alone is not fatal. Early-onset Parkinsons disease does not always present the same way as late-onset Parkinsons disease, and there is no definite prognosis. Younger Parkinsons patients may be more at risk of developing non-motor symptoms, such as depression, sleep disorders, anxiety and urinary issues, which can cause health complications as the disease progresses.
However, early-onset patients also show slower disease progression, and it can take years to move between stages. Each case of Parkinsons is reviewed on an individual basis, so only your doctor can tell you your prognosis.
Also Check: Parkinsons Hallucinations Commercial
Don’t Miss: Parkinson’s Side Effects Elderly
Impact Of Prior Mdma Administration
5-HT neurons would be affected by the pathological process linked to Lewy bodies before DA neurons . In addition, lesions of the 5-HT system are detected in de novo PD patients and also in asymptomatic subjects carrying SNCA mutations . We have therefore decided to investigate the impact of MDMA administration prior progressive MPTP on macaques . Compared to acutely MPTP-treated monkeys, double-lesioned ones exhibited less severe parkinsonism. But remarkably, double-lesioned monkeys exhibited more severe and persistent deficits of spontaneous activities and motor symptoms than MPTP moderately-lesioned ones. Greater deficits in spontaneous activities could reflect a lack of motivation or a higher level of anxiety-like behavior, as we have linked apathy, depression, and anxiety to 5-HT deficits in PD patients . The enhanced tremor observed in double treated monkeys was less surprising as 5-HT dysfunction has been linked to tremor in both parkinsonian rodents and patients . Finally, prior MDMA administration enhanced dystonic posture, suggesting the involvement of a 5-HT component. Of note, dystonia can be the presenting symptom of untreated PD, especially common in patients with young-onset PD and responds variably to DA treatments . The use of a specific 5-HT toxin, such as the 5,7-dihydroxytryptamine , combined to MPTP in NHPs, would be extremely useful to decipher deeper the 5-HT pathways involved in each of these symptoms.
Sharing My Story To Help Others
The reason that I started this story about my youth is that I contend that Parkinsons may start at birth for some people. Maybe we were born with too little dopamine. Has anyone else thought the same thing? If so, we need to let the experts know. I hope my story will help some of you that are struggling with a new diagnosis of Parkinsons. I love to use it as an excuse for just about everything. Oops, didnt mean to say that its the Parkinsons. I even started flailing my arms around a student who was misbehaving. Oops, I said, Its the Parkinsons. I feel very lucky to have early onset Parkinsons. I am happy that I can still walk, talk, and have fun with family and friends. Im glad that I dont have cancer or a more serious illness. I thank God that they figured out dopamine helps. I hope that I will continue to be able to laugh at my Parkinsons and blame it for all kinds of things.
Also Check: Neck Brace For Parkinson’s
Eo Parkinsonism Associated With Metabolic Conditions
A number of metabolic disorders can present with EO parkinsonism. Diseases caused by mutations in genes encoding for mitochondrial proteins are usually characterized by short stature, diabetes, ophthalmoplegia, deafness, cardiomyopathy, as well as neurological disorders such as myoclonus, seizures, and stroke like episodes . The majority of the reports of parkinsonism and mitochondrial diseases consist of single case descriptions, as summarized in previous works . Although in most of these cases the neurological symptoms, including parkinsonism, manifest during childhood, onset after the age of 21 year is possible. Thus they should be considered in the differential diagnosis of EOPD. Some of these conditions are described below . Matrilineal heritability, due to mutations of genes in the mitochondrial DNA, can be a key factor for suspecting these diseases.
Parkinsonism has also been reported in a growing number of conditions caused by impairment of the lysosomal/lipid metabolisms, such as Gaucher disease . Parkinsonism has been described in single cases of Niemann Pick type C , although screenings of large cohorts of patients with PD failed to confirm the association between mutations of the NPC-causative genes, NPC1 and NPC2, and PD. On the contrary, variants of the SMPD1 gene, that is responsible for Niemann Pick types A and B, have been associated with PD across different populations . NPC and GD are far more common among Ashkenazi Jews.
Geographical Variation In Pd Incidence

The age and sex adjusted county rates of newly diagnosed, treated Parkinson disease among eligible Medicare beneficiaries, with Bayesian hierarchical modeling and smoothing to increase the precision of estimates in less populous areas, is shown in Fig. . A clustering of counties with a higher incidence of PD was observed at the juxtaposition of the Midwestern and Southern regions of the United States. Other higher incidence areas were found in southern California, southeastern Texas, central Pennsylvania, and Florida. Lower incidence areas included the Mountain West region, the western Midwest, and the far Northwest.
Fig. 2
Also Check: How Long Can I Live With Parkinson’s Disease
Causes Of Parkinsons Disease
Parkinsons disease is caused by a loss of nerve cells in part of the brain called the substantia nigra. This leads to a reduction in a chemical called dopamine in the brain.
Dopamine plays a vital role in regulating the movement of the body. A reduction in dopamine is responsible for many of the symptoms of Parkinsons disease.
Exactly what causes the loss of nerve cells is unclear. Most experts think that a combination of genetic and environmental factors is responsible.
Stooping Or Hunching Over
Are you not standing up as straight as you used to? If you or your family or friends notice that you seem to be stooping, leaning or slouching when you stand, it could be a sign of Parkinsons disease .
What is normal?If you have pain from an injury or if you are sick, it might cause you to stand crookedly. Also, a problem with your bones can make you hunch over.
Also Check: Parkinson’s Physical Therapy Interventions
Treating Early Onset Parkinsons Disease
Although no cure exists, identifying symptoms and determining a proper course of treatment helps many Parkinsons patients to remain active and lead fulfilling lives. Carbidopa/levodopa is usually prescribed for Parkinsons disease. However, early onset Parkinsons patients are more likely to develop side effects from this treatment, such as or involuntary movements at the medicines peak effect, and cramping as the effect wears off.
For this reason, physicians often treat movement symptoms in people newly diagnosed with early onset Parkinsons disease with other types of drugs, such as anticholinergics, monoamine oxidase B inhibitors, and dopamine agonists.
Parkinsons News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Parkinsons Disease: Causes Symptoms And Treatments
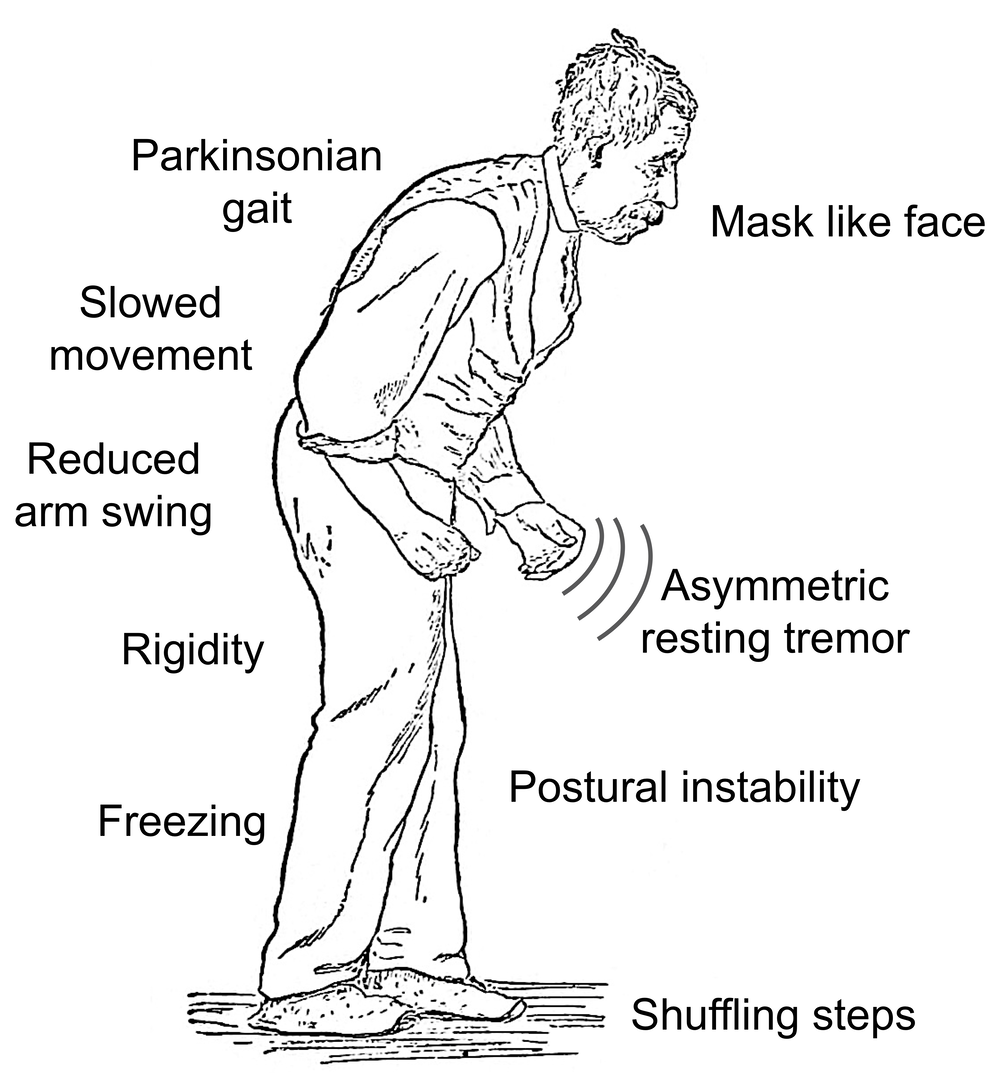
Parkinsons disease is a brain disorder that causes unintended or uncontrollable movements, such as shaking, stiffness, and difficulty with balance and coordination.
Symptoms usually begin gradually and worsen over time. As the disease progresses, people may have difficulty walking and talking. They may also have mental and behavioral changes, sleep problems, depression, memory difficulties, and fatigue.
While virtually anyone could be at risk for developing Parkinsons, some research studies suggest this disease affects more men than women. Its unclear why, but studies are underway to understand factors that may increase a persons risk. One clear risk is age: Although most people with Parkinsons first develop the disease after age 60, about 5% to 10% experience onset before the age of 50. Early-onset forms of Parkinsons are often, but not always, inherited, and some forms have been linked to specific gene mutations.
You May Like: Home Care For Parkinson Disease
A Patient Perspective On Early
Michael S. Fitts, assistant dean for user access and diversity for The University of Alabama at Birmingham, speaks on his experience with early-onset Parkinson disease and the challenges and misconceptions associated with the condition.
Michael S. Fitts, assistant dean for user access and diversity for The University of Alabama at Birmingham, speaks on his experience being diagnosed with early-onset Parkinson disease at the age of 38 and the challenges and misconceptions associated with the condition.
Transcript
AJMC®: Hello, I’m Matthew Gavidia. Today on the MJH Life Sciences Medical World News, The American Journal of Managed Care® is pleased to welcome Michael S. Fitts, assistant dean for user access and diversity for The University of Alabama at Birmingham.
Diagnosed at the age of 38 with Parkinson disease, Michael serves as an advocate for the education of those with early-onset Parkinson disease and is part the Michael J. Fox Foundation Patient Council.
Michael, glad to have you on. Can you just introduce yourself and tell us a little bit more about your work?
Fitts: Yes, thank you for having me. As you already said, my name is Michael Fitts, and I am a patient advocate for the Michael J. Fox Foundation’s Patient Council. As far as my full-time job, I work at the University of Alabama at Birmingham, specifically UAB libraries, and there I serve as assistant dean for user access, which is all the services that we provide for the students, staff, and faculty.
Definition Of Parkinsons Disease
Parkinsons syndrome is characterized by the clinical triad of rigor, tremor, and akinesia as well as possible postural instability.
Based on etiology, one can further distinguish between idiopathic Parkinsons disease, which is synonymous with Parkinsons disease, and atypical and symptomatic parkinsonism.
Idiopathic Parkinsons disease or Parkinsons disease is considered a diagnosis of exclusion, in the absence of a specific cause.
Symptomatic Parkinsonism, however, is triggered by certain identifiable factors. For example, in the context of intoxication, manganese or lead may cause the disease. Parkinsons syndrome is also triggered by medication, e.g., neuroleptics.
Parkinsons syndrome occurring in the context of other neurodegenerative diseases is referred to as atypical Parkinsonism.
Recommended Reading: Parkinson’s Disease And Sleep Disorders
Eo Parkinsonism Associated With Other Neurological Symptoms
Dystonia-parkinsonism syndromes
Parkinsonism may be part of the clinical spectrum of syndromes defined as dystonia-parkinsonisms. This term applies to rare conditions where the severity of dystonia usually equals that of parkinsonism. Unlike the parkinsonian syndromes with additional dystonia , these conditions usually have their onset in childhood. The phenotype is often non-specific to a particular form and genetic investigations are required.
DYT-GCH1 typically presents with lower-limb dystonia, causing gait disturbance and a tendency to fall. Clinical features like diurnal fluctuation and sleep benefit are typically associated with this form and can be helpful in differentiating it from other forms of EOPD. The response to levodopa of both dystonic and parkinsonian signs is remarkable with low-doses with no development of the levodopa-induced dyskinesias.
Parkinsonism-ataxia
Parkinsonism, PEO, or optic atrophy
Parkinsonism and spastic paraplegia
Mutations in the SPG11 gene have been identified to be a major cause of autosomal recessive hereditary spastic paraplegia with thin corpus callosum. Juvenile-onset symmetric parkinsonism has been described, with variable response to dopamine intake .
Other SPG syndromes may display parkinsonism as part of the clinical picture, in particular in SPG7 and SPG15 .
Parkinsonism and intellectual disability
Phenotypes associated with mutations in WDR45 have already been discussed .
Parkinsonism and seizures