Excessive Daytime Sleepiness In Pd
Excessive daytime sleepiness is a common symptom in PD and can occur anywhere from 15 to 21% early in the disease course and up to 46% as the disease progresses . A study of early and untreated PD showed that EDS may be related to disease progression and is independent of other sleep disorders, while others have shown that dopaminergic medication appears to increase EDS in a dose-dependent fashion . Some studies have also suggested an association of EDS in PD with depression . Interestingly, patients with PD and EDS appeared to have reduced uptake in the basal ganglia on dopaminergic terminal imaging compared to those without EDS . The PD and EDS groups also have worse scores on motor, nonmotor, autonomic, and cognitive testing . This suggests that more severe disease could be a contributing factor to development of EDS, in addition to dopamine medication levels .
The presence of EDS negatively impacts quality of life in PD. One study evaluated 198 patients with PD using the Parkinsons Disease Questionnaire 39 , a measure of quality of life . This study demonstrated that those with PD and EDS had a significantly lower overall score on the PDQ-39 than those without EDS , as well as individual emotional, social, and physical domains measured by this survey . EDS in PD also represents an additional risk of falling. One study evaluated 120 patients with PD and found that every point increase on the Epworth Sleepiness Scale was associated with a 20% higher risk of falling .
How Are Sleep Problems Treated In People With Parkinsons Disease
Your provider will recommend treatments that address whats causing your sleeping challenges. Your provider may:
- Change your medication: If a medication could be causing your sleep issues, your provider may decide to adjust your treatment plan. Reducing the dose or switching medicines may solve the problem.
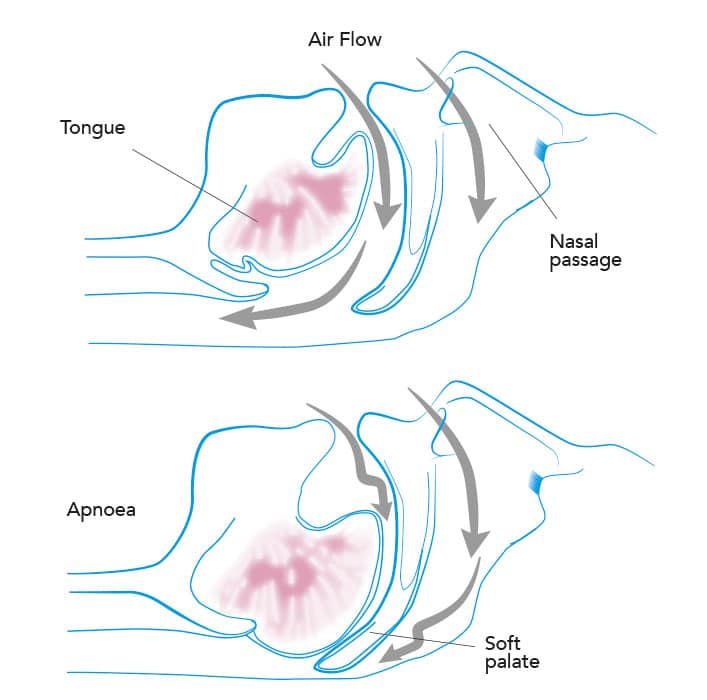
- Prescribe a new medication or therapy: If you have a sleep disorder, your provider will discuss your options. In some cases, your provider may recommend a new medication. If you have sleep apnea, wearing a special oral appliance can help. The device enables you to get a steady flow of oxygen, so your body doesnt gasp for air.
- Suggest lifestyle changes: Your daily habits and sleeping environment can help or hurt your sleep efforts. Setting regular sleep and wake times, keeping the room dark and avoiding electronic screens at bedtime may improve how well you sleep. If you have REM sleep disorder, your provider will discuss options for how best to protect you while you sleep.
Deep Brain Stimulation In The Treatment Of Sleep Disorders In Pd
Studies investigating the effect of DBS in the treatment of sleep disorders in PD patients showed that DBS improved the sleep scales and quality . Baumann-Vogel et al. found that subthalamic nucleus DBS-enhanced subjective sleep quality, reduced sleepiness measured by the Epworth sleepiness scale, and reduced sleep fragmentation shown by actigraphy recordings. However, the authors observed that subthalamic DBS was not improved REM sleep features . Similarly, Cicolin et al. reported that RBD symptoms did not benefit from STN DBS. On the other hand, Chahine et al. reported that STN DBS improved significantly symptoms of RLS in PD patients. The effect of PPN DBS on sleep disorders in PD has been investigated in several studies . One study showed that PPN DBS improved sleep quality and reduced EDS however, it caused a reduction in REM latency and a relevant increase in REM sleep . In another study, it has been reported that PPN DBS improved the total duration and rate of REM sleep . As a result, DBS seems to be beneficial in the treatment of sleep disorders in PD because it seems to be useful in improving sleep quality. However, large-scale prospective studies are needed to understand the benefits of DBS in the treatment of sleep disorders in PD.
Read Also: Meds For Parkinson’s Psychosis
Limitations Of Estimating Pd Prevalence
When asked about the limitations of the study, Dr. Natalie Diaz, a board-certified neurologist at the Pacific Movements Disorder Center at Pacific Neuroscience Institute at Providence Little Company of Mary Medical Center Torrance in Torrance, CA, not involved in the study, told MNT:
While the study looks at PD incidence by age, sex, and geographical variation in each of the datasets, there is no mention of racial and ethnic differences. Caucasian and Hispanic populations have a higher incidence of PD as compared to African, American Indian, or Asian populations. Could race and ethnicity play a role in regional differences of incidence or could the changing demographics of our nation play a role in the increase of the projected incidence of PD in North America?
Dr. Shilpa Chitnis, Ph.D., professor of neurology at UT Southwestern Medical Center, not involved in the study, added that the data may be unrepresentative of today, given the increased prevalence of risk factors such as diabetes, pesticides, and physical inactivity since 2012.
Effect Of Melatonin On Daytime Sleepiness
Five studies used the Epworth Sleepiness Scale to assess the daytime sleepiness of patients with PD. The study of Medeiros showed that in the melatonin group, the mean change in ESS score at the end of treatment was 0.3 it was 0.2 in the placebo group. However, the difference was not statistically significant. The trial showed that treatment with 4 weeks of 3 mg melatonin did not affect daytime sleepiness in patients with PD. In a 6-week, randomized, clonazepam-controlled study, Litvinenko et al. reported that melatonin and clonazepam increased ESS scores in patients with PD. The results showed that ESS scores significantly increased after treatment with 6 weeks of 2 mg clonazepam and were slightly increased after treatment with 6 weeks of 3 mg melatonin .
Delgado et al.’s study used 25 mg of melatonin to assess its efficacy on daytime sleepiness in patients with PD. Melatonin was taken at noon and 30 min before bedtime for 3 months. The results showed that the use of high-dose melatonin failed to reduce the presence of excessive daytime sleepiness . Meanwhile, similar results were observed in that ESS scores after treatment with 4 weeks of 2 mg PRM were not different from baseline .
Recommended Reading: Signs And Symptoms Of Early Parkinson’s Disease
The Impacts Of Insomnia On Those With Parkinsons Disease
Sleep disorders are one of the most common non-motor symptoms of people living with Parkinsons disease. In fact, research shows that sleep disorders affect approximately 64 percent of people with PD. Of that percentage, up to 80 percent deal with insomnia a far higher percentage than the general population who live with sleep difficulties.
While insomnia refers to the inability to fall asleep or stay asleep, sleep issues can lead to a host of issues, including the following medical conditions:
- Fatigue and excessive daytime sleepiness
- Increased stress
You May Like: Nad Therapy For Parkinsons Disease
Treatment For Rem Sleep Disorder
Consider making environmental adjustments to protect the person with RBD and bed partner from injury. This may include padding the floor, creating a barrier between bed partners, or sleeping in separate beds or rooms.
Read Also: Gender Differences In Parkinson’s Disease
Cognitive Performance In Rapid Eye Movement Sleep Behavior Disorder And Epworth Sleepiness Scale Subgroups
Cognitive measures in patients with abnormal ESS scores indicating daytime sleepiness did not differ from patients with normal ESS values . When analyzing cognitive performance in patients with and without RBD, no differences were detected in the overall PANDA cognition results and the TAP scores , and no relevant differences in clinical and PSG parameters were detected between both groups .
Table 6. Cognitive parameters of patient subcohorts with and without REM Sleep Behavior Disorder .
Sudden Onset Of Sleep And Eds
Sudden onset of sleep may warrant other measures, and those with high sleepiness scores should be advised to drive cautiously and not to drive alone or for long distances . Dopamine agonists when started should be titrated up slowly especially in older patients, and patients with excessive day-time sleepiness may respond to an alternative agonist. In patients with severe EDS, concurrent medications that may be sedating should be eliminated or reduced. Formal sleep studies may be required in some patients, and in those with a narcolepsy-like phenotype, modafinil may be useful. Modafinil, a sleepwake cycle activator, is non-stimulating and is the only drug which has shown efficacy in improving EDS without detrimental effect on PD when examined in double-blind placebo-controlled trials . A 7-week double-blind placebo crossover study of 200 mg modafinil followed by a 4-week open-label extension study by Adler et al. showed significant improvement in ESS with modafinil and improvement in clinical global impression scores for wakefulness in the open-label arm. Where EDS is thought to be secondary to the use of dopamine agonists, modafinil may allow the continuation of dopamine agonist therapy.
Don’t Miss: Is Fatigue A Symptom Of Parkinson’s
Assessment Of Risk Of Bias
The risk of bias of each RCT was assessed independently by two authors, and another author resolved any disagreement. We used the Cochrane Risk of Bias Tool to assess the risk of bias. The assessment tool is composed of seven parts: random sequence generation allocation consultation blinding of the participants and personnel blinding of outcome assessment incomplete outcome data selective reporting and other bias. We divided the research into three categories, including low risk of bias,high risk of bias, or unclear risk of bias.
Conflict Of Interest Statement
GL received honoraria for participation in clinical trial as sub-investigator from UCB Pharma PC received honoraria for speaking engagements or consulting activities from Allergan Italia, Lundbeck Italy, UCB Pharma S.p.A, Chiesi Farmaceutici, AbbVie srl, Eli Lilly and Company, Zambon FP received honoraria for speaking engagements or consulting activities from Sanofi and Bial. The other authors declare no conflict of interest.
Recommended Reading: Natural Supplements For Parkinson’s Disease
Nighttime Hallucinations Psychosis & Confusion
Nighttime hallucinations and confusion may result from any combination of cognitive impairment, dopaminergic medications, age and PD-related vision changes and lack of sleep. Psychosis may first appear after infection, trauma, surgery or prolonged hospitalization. Symptoms may range from a sensation that someone or something is standing at the side of or behind the person, to very detailed and often frightening visions. Delusions may occur as well.
Treating Parkinsons Psychosis
The first-line approach to treatment of PD psychosis involves simplification of the anti-PD medication regimen and adjusting dose timing , treating other sleep disturbances, providing a consistent and familiar sleep environment , and in more severe cases, the use of atypical antipsychotic drugs.
Most of the available anti-psychotics are always avoided in PD psychosis because they block dopamine receptors and can cause significant problems with movement. However, two anti-psychotic medications, quetiapine and clozapine, are sometimes used as they have less of an ability to worsen motor symptoms. However, data for the use of quetiapine is limited and clozapine requires the patient to undergo frequent blood draws to monitor blood counts. A newer medication pimavanserin, was approved by the FDA to treat PD psychosis. It has a different mechanism of action, and does not block the dopamine system, but rather the serotonin system, and therefore does not increase motor symptoms.
Restless Legs Periodic Limb Movements And Sleep
Both drug-naïve and drug-treated PD patients may develop a syndrome of nocturnal restlessness resembling RLS and periodic leg movements during sleep, whereas RLS has been reported to occur in PD at a rate twice the normal prevalence of RLS in general population .
Sleepy PD patients may also have day-time somnolence because of sleep-disordered breathing, and formal polysomnography will identify sleep apnoea in a considerable number of such patients . Obstructive sleep apnoea may occur in up to 50% of patients with PD with resultant daytime sleepiness and tiredness. Sleep apnoea may co-exist with RLS or PLM or RBD . This is important to diagnose as these patients need specific and targeted treatment.
Also Check: Is Rls Related To Parkinsons
Also Check: Parkinson’s Disease Breakthrough 2021
Rbd And Other Parasomnias
In patients with PD, beyond the well-known and peculiar occurrence of REM sleep behavior disorder , non-REM-sleep parasomnias and parasomnia overlap disorder have also been described.
Bassetti and co-workers systematically investigated the presence of sleepwalking in 165 consecutive PD patients. 3.6% reported adult-onset sleepwalking. In 4 out of 6 patients, RBD was detected on video-polysomnography . In another study, video-polysomnography was used to assess 30 patients with PD . Again, 8 out of 10 patients with a history of sleepwalking presented RBD on vPSG. Sleepwalking in this cohort was associated with depression, higher disease severity, and functional disability. Due to the frequent occurrence of overlap parasomnia, the authors suggested that a common underlying disturbance of motor control during sleep exists in PD .
The diagnostic criteria for RBD comprise repeated episodes of sleep-related vocalization and/or complex motor behaviors, and these behaviors need to be documented by PSG as occurring during REM sleep, or, based on a clinical history of dreaming, are presumed to occur during REM sleep. In addition, it is obligatory that polysomnographic recording demonstrates REM sleep without atonia . Other sleep-related movement disorders that are frequent in PD might produce similar symptoms mimicking RBD by history and need to be excluded.
Insomnia And Daytime Sleepiness In Patients With Parkinsons Disease
As outlined above, patients with PD frequently experience insomnia, most often as a disorder of sleep maintenance, but also as a disorder of sleep onset or early morning awakening. The diagnosis of insomnia is always based on subjective symptoms. Patients report difficulties falling asleep or maintaining sleep, early awakening or non-restorative sleep, associated with subjective concern or daytime impairment . Notably, there is sometimes a discrepancy between subjective complaints of insomnia and only subtle disturbances of sleep structure in otherwise healthy people, whereas in patients with PD, in addition to the subjective complaints of insomnia, there is often a significant manifest disruption of the integrity of sleep macro and microstructure.
Joy and co-workers evaluated newly diagnosed levodopa-naïve patients with PD and reported frequent and variable alteration of sleep macro-architecture in these patients . However, Ferreira and co-workers reported poor sleep quality and sleep architecture changes in PD patients, which improved with levodopa following improvement of motor symptoms , but dopamine did not reverse sleep architecture changes .
You May Like: Mcc950 Clinical Trials Parkinson’s
Circadian Rhythm Sleep Disorders
Circadian rhythm sleep disorders potentially influence daytime and nocturnal dysfunctions. It is common to find that PD patients go to bed and wake up very early therefore, a phase advance may occur . Advanced sleep phase is usually associated with older age and characterized by involuntary sleep and waking times that are generally more than 3 h earlier than usual sleep times. For patients with PD, both age-related changes and brain damage can provoke circadian rhythm sleep abnormalities. This relationship deserves more careful clarification, although it is complex. For instance, a slower absorption rate of levodopa during nighttime, possibly related to delayed gastric emptying, has been reported in PD patients . In agreement with this example, it has been documented that phase advance in PD is possibly influenced not only by age but also by dopaminergic therapy and disease severity . Given the complexity of this issue, an abnormal pattern of daily activities and associated comorbidities, such as depressive symptoms and daytime sleepiness, could also influence circadian rhythms . Thus, the analysis of this complex issue must take all of these variables into careful consideration.
Develop A Bedtime Routine
Your bedtime routine should help you prepare for bed. So be sure to follow it every evening. Essential tasks that every bedtime routine must have include:
- Having a Light Snack: Eat only light snacks if you get hungry before bed. Heavy meals before going to bed are unhealthy and can result in weight gain. Also, avoid snacks that might contain stimulant ingredients like alcohol and caffeine.
- Taking a Warm Bath: Bathing in warm water before bed may improve sleep quality. However, be sure not to spend too much time in the bath as it may wake up your body.
- Go to the Toilet: Be sure to finish your business in the bathroom before bed. Minimize your liquid intake at least three hours before bedtime to help avoid nocturia.
- Brush Your Teeth: Brushing your teeth right before bed helps prevent dental problems, including cavities and decay. Although it is indirectly related to better sleep, having this step in a bedtime routine is helpful.
Read Also: Meds For Parkinson’s Tremors
Pathophysiology Of Excessive Daytime Sleepiness In Pd
It has been reported that there are three main causes of sleepiness in PD deterioration of night sleep quality, neurodegeneration of sleepwake-related brain regions, as a result of disease pathology, and the side effects of antiparkinsonian medications . However, many of the abovementioned causes may be related to EDS. For this reason, it is necessary to consider these causes in the diagnosis and treatment of EDS.
Symptoms And Diagnostic Considerations
Rapid Eye Movement Sleep Behavior Disorder is a non-familial sleep disorder, characterized by the loss of the inherent muscle atonia observed during normal REM sleep. This phenomenon is often referred to as REM Sleep without Atonia . Whilst isolated RSWA is frequently an incidental finding in sleep studies, it forms the substrate of the dream enactment behavior which defines RBD. Here, individuals experience vivid dreams which they act out during sleep.
It is important to remember that dream enactment and limb movements during sleep can occur in the healthy population, often in the context of heightened emotional states . The same symptoms may also be experienced during withdrawal from sedatives or alcohol. In non-pathological dream enactment, individuals typically respond to dream content during the transition from REM sleep to the awake state and while maintaining REM atonia during much of the REM period. In contrast, RBD individuals will maintain REM sleep during and immediately after most of their dream enactments. As acute dream enactment is generally self-limiting, the chronicity of symptoms is a key distinguishing factor, and forms part of the diagnostic criteria for RBD .
Recommended Reading: Sarah Raven Arthur Parkinson Podcast