How Are Swallowing Problems Treated
The first step to addressing swallowing issues is to speak to a neurologist about getting an evaluation performed by a SLP. This professional will take a medical history and interview the person with PD about eating and swallowing.
This is typically followed by either a video X-ray or an endoscopic examination, so the medical specialist can observe the swallowing process as an individual sips liquid and eats food, as these substances flow from the mouth, down the throat and esophagus, to the stomach. With these tests it is possible to see where the trouble is occurring and to recommend therapies.
Follow the recommendations of the swallowing specialist, which may include the following:
- Exercise and Swallow Hard. Just as exercise can ease other PD-related movement difficulties, it can also help with swallowing. The Lee Silverman Voice Technique® helps a person exaggerate speaking and swallowing. Working with an SLP on an individualized program helps the person to swallow hard and move food from the mouth down the throat.
- Expiratory Muscle Strength Training. This therapy strengthens respiratory muscles, improves cough and swallowing and reduces aspiration.
- Change in food. Modifying liquids and solids can help. For people who find liquids get into the airway, liquids may need thickening. Taking bigger or smaller bites or sips or pureeing solid foods may help. First get an evaluation, so the SLP can recommend how to modify food and liquid.
What Causes Gait To Change
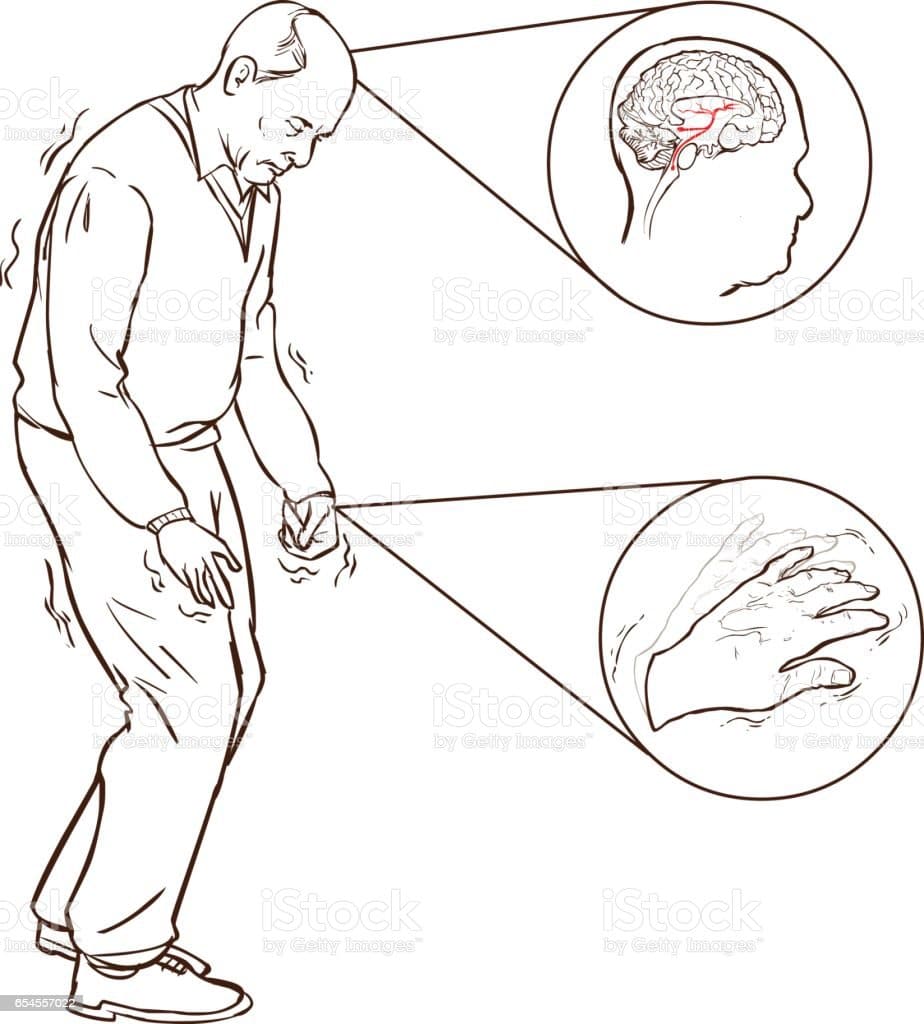
PD causes damage to the nerves in the brain and in the body, as well as causing accumulations of the protein alpha-synuclein, called Lewy bodies.
The motor symptoms of PD, like Parkinsonian gait, are caused by damage to the part of the brain called the substantia nigra pars compacta. The neurons in the substantia nigra produce dopamine, a neurotransmitter that transmits signals from the substantia nigra to other parts of the brain to produce smooth, purposeful movement.2,4
Damage to the neurons in the substantia nigra causes a reduction in dopamine, creating the motor symptoms seen in people with PD.2,4
Medication Not Working The Way It Used To
In the early stages, taking medicine works well to get rid of symptoms. But as Parkinsons progresses, your medication works for shorter periods of time, and symptoms return more easily. Your doctor will need to change your prescription.
Dr. Valerie Rundle-Gonzalez, a Texas-based neurologist, says to pay attention to how long your medicine takes to kick in and when it stops working. She says you should feel like symptoms significantly improve or are almost gone while on medication.
Also Check: Parkinson’s And The Mind
Depression Anxiety And Crankiness
As many as half of people with Parkinsonâs get depressed or anxious at some point. You may feel sad, uninterested, tired, or cranky. Or you may worry and feel on edge all the time.
How can I manage them?
- Exercise regularly. Research shows physical activity eases depression and anxiety.
- Stay in touch with your friends and family.
- Join a support group.
What are the treatments? Youâll want to see a mental health expert, such as a therapist. One kind of therapy, called cognitive behavioral therapy, has been shown to help with depression. You learn to spot negative thoughts and respond in a better way. Your doctor may also prescribe medicine, like antidepressants or anti-anxiety drugs.
Associations Between Gait Changes And Change In Levodopa Dose Over Time
LEDD increased by 106 mg/day each year. Ninety-three percent of people with PD had increased LEDD compared to baseline assessment . Only one gait characteristic was related to LEDD change larger increases in step width variability related to greater increases in LEDD over time . Inclusion of the LEDD × Time interaction resulted in no significant change in step width variability , indicating that step width variability change is at least partially explained by a change in LEDD. All other gait characteristics meeting criteria 1 and 3 did not show associations between gait change and LEDD change and therefore exhibited disease-specific change that was not related to levodopa adjustments .
Read Also: Boxing For Parkinson’s Disease
The Role Of Levodopa In Pd Gait Progression
Although the precise mechanisms of non-dopaminergic gait control are unclear, emerging evidence suggests the importance of the cholinergic system . Cholinergic neurons in the pedunculopontine nucleus influence gait and postural control , and slower walking speed in PD is associated with increases in short-latency afferent inhibition and cholinergic denervation . Also, deep brain stimulation within the PPN may improve step velocity suggesting interventions that target brain regions not primarily dependent on dopamine may therefore help to mitigate gait impairment in PD. The benefits of drugs targeting the cholinergic system on PD gait are also being explored . Overall, interpretation of the relationship between dopamine and gait progression is limited as gait was not assessed off medication, nor were biomarkers of dopaminergic activity such as DAT imaging used. Nevertheless, our findings indicate that discrete gait characteristics progress irrespective of levodopa, suggesting the importance of non-dopaminergic mechanisms in gait impairment.
Implications For Understanding Fog
In this study, the finding that FoG was associated with an underestimation of duration of actual walking through a doorway suggests two broad categories of interpretation: abnormal locomotor execution or abnormal internal representation of locomotion. One could postulate that the absence of a significant motor imagery duration difference between groups in the present study indicates that motor representations are not more impaired in PD subjects with FoG than in PD subjects without FoG, but that FoG arises downstream from these representations, in the execution stage. This explanation is consistent with the theory that FoG is associated with problems in the locomotor centers in the brainstem specifically, in the pedunculopontine nucleus or mesencephalic locomotor region .
You May Like: Everything You Need To Know About Caregiving For Parkinson’s Disease
Sensory Feedback During Walking And Turning
Asymmetric proprioceptive input elicited by vibration of axial muscles produces steering and turning , whereas proprioceptive input from the leg contributes to fine adjustment of the spinal pattern generators for walking . Input from axial muscles would play the role of a servo-mechanism, whereby minor asymmetries initiated by asymmetric foot placement would affect the spinal generators to produce the necessary fine changes in leg and foot kinematics accompanying heading changes.
Whether or not continuous walking along a circular trajectory is also favored by a shift in our straight-ahead goes beyond the scope of this short review, but we would note that a shift in subjective straight-ahead occurs after a period of stepping in place on a rotating treadmill . In turn, it is not unlikely that a shift in the straight-ahead is produced by the feedback from the muscles producing the rotation of the pelvis and trunk over the standing leg when walking along a curved trajectory or when stepping in place and turning . Vision is obviously not necessary for implementing a curved trajectory , but the continuous visual field motion would nonetheless favor the fine tuning of the gait synergies underpinning the production of the circular trajectory .
Dont Miss: How Is Parkinsons Disease Associated With Headaches
What Type Of Exercise Should I Do If I Have Parkinsons Disease
Exercise is a planned, structured, repetitive activity that is intended to improve physical fitness. There is no right exercise for people with Parkinsons. Everyones regimen will differ, depending on overall health, symptoms and previous level of activity. Any exercise helps, and a variety of exercise types may provide well-rounded benefits.
Aerobic exercise
Aerobic exercise involves activities that challenge your cardiorespiratory system such as walking, biking, running, and activities in the pool. Participating in aerobic exercise at least three days a week for 30-40 minutes may slow Parkinsons decline.
Strength training
Strength training involves using your body weight or other tools to build muscle mass and strength. Strength training two days per week, starting with low repetition and weight, may be beneficial in Parkinsons disease. A focus on extensor muscles, or muscles in the back of the body, can help with posture.
Flexibility training
Stretching two or more days per week can be beneficial to maintain range of motion and posture. Holding each stretch of major muscle groups for 30 to 60 seconds can improve muscle length.
Balance and agility training
This type of training often combines aerobic exercise, strength training, and flexibility training. Examples include:
- Tai chi, yoga or Pilates.
You May Like: How Long Has Michael J Fox Had Parkinson
How Are Speech Problems Treated
There are many options to help improve your speech. A speech-language pathologist can help you pick the right approaches for you. Speech-language pathologists are trained health care professionals who specialize in evaluating and treating people with speech, swallowing, voice, and language problems.
Ask your doctor for a referral to a speech-language pathologist. It is also important to contact your health insurance company to find out what therapy and procedures are eligible for reimbursement and to find a list of SLPs covered by your plan. Finally, visit a SLP who has experience treating people with PD.
Have You Ever Thought How Challenging Drinking A Glass Of Water Can Be For Someone Suffering From Parkinsons Disease
On World Health Day, youll likely read about how healthy habits like exercising or drinking more water, can improve your health. While these are helpful tips and important topics to cover, we decided to take things a step further. What if you couldnt drink that glass of water by yourself? It can be daunting to consider, but this scenario can become all-too-real for a person suffering from Parkinsons disease. There are 10 million people in the world suffering from this disorder which is why, today, we decided to share with you how Parkinsons Disease can affect mobility and balance, and what can be done when the disorder is detected in its early stages. That is why raising awareness for this degenerative disease is important, and, while there is still much research to be done, we have high hopes that researchers will find a way to reduce the symptoms of Parkinsons disease, and eventually find a cure. This is becoming more and more urgent, given the fact that life expectancy is rising and the number of individuals with Parkinsons disease will only increase in the future. But is there another solution in sight?
Request Brochure
Recommended Reading: Can You Be Tested For Parkinsons
Read Also: Can Parkinson’s Cause Hip Pain
Changes In The Way You Think
Some people with Parkinsonâs have cognitive changes. That means you may have a harder time focusing, finishing tasks, forming thoughts, thinking of words, and remembering things. When these changes affect your day-to-day life, it becomes dementia.
How can I manage them?
- Exercise regularly, eat a healthy diet, and get enough sleep.
- Clear your home of clutter. Reducing things in the world around you may help with confusion.
- Create a regular routine. You may feel more comfortable with a structured day.
What are the treatments? These changes may be a medication side effect talk to your doctor.
You may need to see an occupational therapist, who can teach you ways to make daily life easier. A speech therapist can help with language issues. There are also some Alzheimerâs drugs that treat these cognitive symptoms.
Treating Freezing Of Gait For People With Parkinsons

Freezing of gait episodes often occur when a person is under-medicated and can improve with increased amounts of their PD meds, usually carbidopa/levodopa. However, as mentioned earlier, the brain abnormalities that lead to freezing of gait are very complex, so giving more dopaminergic medication is only part of the solution. In fact, some people have what is referred to as ON freezing. This means that freezing of gait episodes occur even when other PD symptoms are well treated with their medication regimen.
Cueing, or the introduction of an external sensory stimulus to facilitate movement, has been identified as a way to break a freezing episode. Terry Ellis, PhD, PT, NCS, Director of the APDA National Rehabilitation Resource Center at Boston University, and Tami DeAngelis, PT, GCS, compiled this list of cues that can be used to get out of a freezing episode:
Don’t Miss: Parkinson’s Disease Diet Plan
Treating And Managing Gait Problems
Unfortunately, problems with gait, posture and balance tend not to respond as well to medications as other common motor symptoms, such as tremor, rigidity and bradykinesia . In addition, higher doses of medication over time to manage symptoms such as dyskinesia and orthostatic hypotension can sometimes increase problems with gait.
Nevertheless, there are lots of things you can do to help yourself and there are also experienced professionals who can offer very useful advice. Each case will be different and it is hard to generalise but depending on where you live your doctor will normally be your first contact and they may refer you to one or more of the professionals listed below.
Production Of Dopamine Neurons From Stem Cells: Could We Be One Step Closer To The Cure
As the disease progresses, people may experience reduced quality of life, if normal functions such as swallowing, start to be affected. Currently, there is no known cure for Parkinsons disease. Once Parkinsons is diagnosed, the symptoms can often be treated with medications and therapies, especially in the early stages. However, the scientific community is making every effort to find a way to cure or at the very least find more effective ways to lessen the symptoms of this physically impairing disease.
As we mentioned before, the disease primarily affects dopamine-producing brain cells or neurons. The good news is, scientists in Sweden have identified some insights and a set of markers that should help control the quality of stem cells engineered for clinical use to treat Parkinsons disease. As the disease progresses and dopamine-producing brain cells malfunction and die, it leads to lower levels of dopamine, which is a chemical messenger essential for controlling movement. These findings should help fine-tune stem cell engineering to produce pure populations of high-quality dopamine neurons. Then, a pool of progenitor cells can be transplanted into the brains of patients, so they can make new supplies of dopamine cells.
But while this exciting new research is still in the lab, what else can we hope for to delay the symptoms of Parkinsons and improve the quality of life of those suffering from the disease?
Sign up for our informative newsletters
Also Check: Drugs For Parkinson’s Psychosis
B: Pick Your Own Music
Now that youve seen the full effects of walking to a beat, take your pick of music.
Below I have laid out a list of songs you can try out that have a range of tempos. There is a slow, medium, and fast playlist. Start walking to a slower song . As you get comfortable, you can increase the tempo.
The end goal is to walk to a beat that is slightly faster than your stride. Not only will this push you to transcend your normal Parkinsonian gait, it will also give you a longer lasting therapeutic effect after you stop listening.
Here are the playlists:
You can, of course, choose your own songs. In fact, once you practice a few times with these songs, I encourage you to start using your own selections .
Either way, I want you to look forward to turning on your iPod or Android, and that means having songs that make you want to dance, to move, to run. If you dont know the tempo of a song you like, you can measure the beats per minute at songbpm.com.If you want to change the tempo of a song that is too fast or too slow, I like to use the app TempoSlowmo. You can download it for free in the Apple App Store for your iPod or on Google for your Android.
Good luck. If you have any questions or comments about the post, Id love to see them! Write them in the comment section below and Ill respond as soon as I see it!
Also Check: How Does Occupational Therapy Help Parkinson Disease
Why Does Freezing Of Gait Occur
It is not completely clear why some people with PD experience freezing of gait and others do not. Research suggests that there is a relationship between freezing of gait and cognitive difficulties. The brain circuitry that controls gait is extremely complex and involves multiple connections between various parts of the brain, including:
- areas in the front of the brain that plan and initiate movement
- areas of the basal ganglia where the dopaminergic neurons that refine and control movement are found
- areas in the brainstem which modulate movement and wakefulness
Freezing of gait seems to be caused by short-lasting episodes of inhibition of these brain circuits that coordinate gait. The specific abnormalities that cause the problem may differ from person to person.
Also Check: Laser Light For Parkinson’s Disease
How Does Parkinsons Disease Impact How You Walk
Since Parkinsonâs Disease is a neurodegenerative disorder that impacts both motor and sensory systems, this can manifest as changes in the way you walk. Gait analysis for patients with PD is particularly important as these changes are often suboptimal and make it more difficult to walk. The good news is that physical therapists can use information learned from gait analysis to help identify the areas a person can improve upon when they are walking, preserving their independence and reducing their risk for falls.â
Improving Flexibility And Range Of Motion
Improving your flexibility can help you improve your balance and gait, as well as reduce rigidity. Try these exercises:
- Sit in a chair and bend your upper body at the waist to your right and left.
- Get on all fours and turn your upper body to the right and left. Lift your arm on the side youre turning to as you turn.
Also work on lower-body strength training. Strength training can help you improve your balance, walk further distances, and potentially increase your walking speed. Some exercises to try include:
- Leg presses. While sitting down, push a weight away from your body using your legs.
- Squats. Start in an upright position with your legs slightly wider than hip distance. Bend your knees while pushing your glute muscles back, so that your knees dont come over your toes. You can hold onto something if necessary. You dont have to go down more than a few inches.
- Exercise bike. If you have access to a recumbent exercise bike , using the bike can help strengthen your legs.
- Repeatedly sit in and rise out of a chair. Repeating the motions of sitting down and rising helps strengthen your leg and core muscles. It also helps you practice a functional activity.
Read Also: New Research On Parkinson’s Disease