I Had A Hallucination: What Next
Research has shown that for many people with PD who have them, hallucinations begin after a change in medication, more specifically, an increase in levodopa . Additional factors make a person more likely to experience hallucinations when medications are changed, such as other cognitive problems or memory issues, depression and sleep problems. Dementia|A term used to describe a group of brain disorders that cause a broad complex of symptoms such as disorientation, confusion, memory loss, impaired judgment and alterations in mood and personality.] also increases the risk of hallucinations and delusions when PD medications are changed. Dementia means cognitive changes whether in memory, judgment or attention that interfere with daily life.
One thing that does not affect the risk of hallucinations is your regular dose of levodopa. Rather, studies show that it is a change in dose an increase in a dose that has been stable that sets off hallucinations.
Tip: Experiencing a hallucination does not mean you are going crazy. Many people recognize that their hallucinations are not real. Do not react to these visions or sounds or engage them dismiss them. Bring up the topic with your doctor immediately.
What Are The Symptoms Of End
In addition to needing help with daily tasks, symptoms of stage 5 Parkinsons include:
- Inability to rise from sitting or lying down without assistance
- Inability to walk or stand due to leg stiffness or freezing
- Possible hallucinations and/or delusions
People with end-stage Parkinsons can have a variety of severe motor and nonmotor symptoms including:
- Personality changes
What Should I Do Once The Hallucination Passes
After the hallucination passes, you can try to talk through the experience together. If the person has insight, it may be easier for them to understand and talk about what just happened.
Write down what happened during the hallucination. Note the time of day and what the person was doing when it started.
Taking notes each time it happens can help you identify the triggers. It could be related to the timing of medication, and your loved one might feel a sense of relief and control in knowing that pattern.
Ask what you can do to stop it from happening again. This might include adjusting their medication dosage or adding an atypical antipsychotic drug to their medication regimen.
Read Also: What Is The Life Expectancy Of A Person With Parkinson’s
Hallucinations And Rem Sleep Disorders In Parkinson’s Disease
At timestamp 1:58 in this recording of Thrive: HAPS 2020 Caregiver Conference, you will find a one hour talk by neurologist Joohi Jimenez-Shahed, MD. In it she delves into what REM sleep behavior disorder is and is not, and the distinctions between hallucinations, delusions, and delirium. Managment options for RBD and hallucinations are included.
Parkinsons Disease Psychosis: The What When Why And How
Psychosis is a psychiatric term used in neurology to refer to a spectrum of abnormalities. Parkinsons disease psychosis is where people experience hallucinations or delusions. Hallucinations is seeing, hearing, or smelling things that dont exist. With tactile hallucinations, one can feel a presence that isnt there. Delusions are believing something that is not true, like that a spouse is being unfaithful or caregivers are stealing. In this one-hour talk, movement disorder specialist Christopher Goetz, MD, focuses on hallucinations and spends a little time on delusions.
Don’t Miss: Micrographia In Parkinson’s Disease
Age And Duration Of Illness
Increased age has been associated with the presence of hallucinations. This might be explained by accerelated sensory loss or age related side effects of medication. One of the main confounders with age is duration of illness when the non-independence of these variables was controlled, Fénelon et alfound that duration of illness was the crucial factor. Grahamet al identified two subgroups of patients with Parkinson’s disease experiencing hallucinosis: in those with disease duration of 5 years or less, visual hallucinations were associated with rapid progression of the motor but not the cognitive component of the disease. In the remainder with longer histories, visual hallucinations were associated with postural instability, global cognitive impairment, and the lack of depression. Goetz et al contrasted patients with Parkinson’s disease who experienced hallucinations within 3 months of levodopa therapy with those who experienced hallucinations after 1 year of treatment. Diagnoses in the early onset group more often changed to Lewy body or Alzheimer’s disease. Lewy bodies are present to a greater or lesser degree in all cases of Parkinson’s disease and are known to be associated with visual hallucinations.
Types Of Hallucinations In People With Parkinsons Disease
Hallucinations involve the five senses: sight, smell, touch, hearing, and taste.
People with hallucinations have sensory experiences that feel real to them, but are not actually happening and are not apparent to anyone else.
Types of hallucinations include:
- Auditory: Hearing things
- Gustatory: Tasting things
For people who experience Parkinsons-related hallucinations, the hallucinations are usually visual. They are typically non-threatening, but less commonly they can be of a threatening nature.
Often people with Parkinsons disease psychosis see small people or animals, or loved ones who have already died. They are not interacting with them, just being observed.
Auditory hallucinations are more common in people with schizophrenia, but can happen with Parkinsons disease. With Parkinsons disease, auditory hallucinations are usually accompanied by visual hallucinations.
More specific types of hallucinations experienced by people with Parkinsons disease include:
Read Also: Sole Support For Parkinson’s
Hallucinations And Delusions In Pd
Hallucinations and delusions are collectively referred to as psychosis.
Visual hallucinations are the most common type of hallucination. In a visual hallucination, someone sees things that are not actually there. There can also be auditory and olfactory hallucinations. Often hallucinations are not alarming to the person experiencing them.
Delusions are when there is an alternative view of reality: an entire irrational story is created. Paranoia is a common type of delusion. Capgras delusions are a specific type of delusion where the person believes that a spouse, adult child, or other family member has been replaced by an imposter.
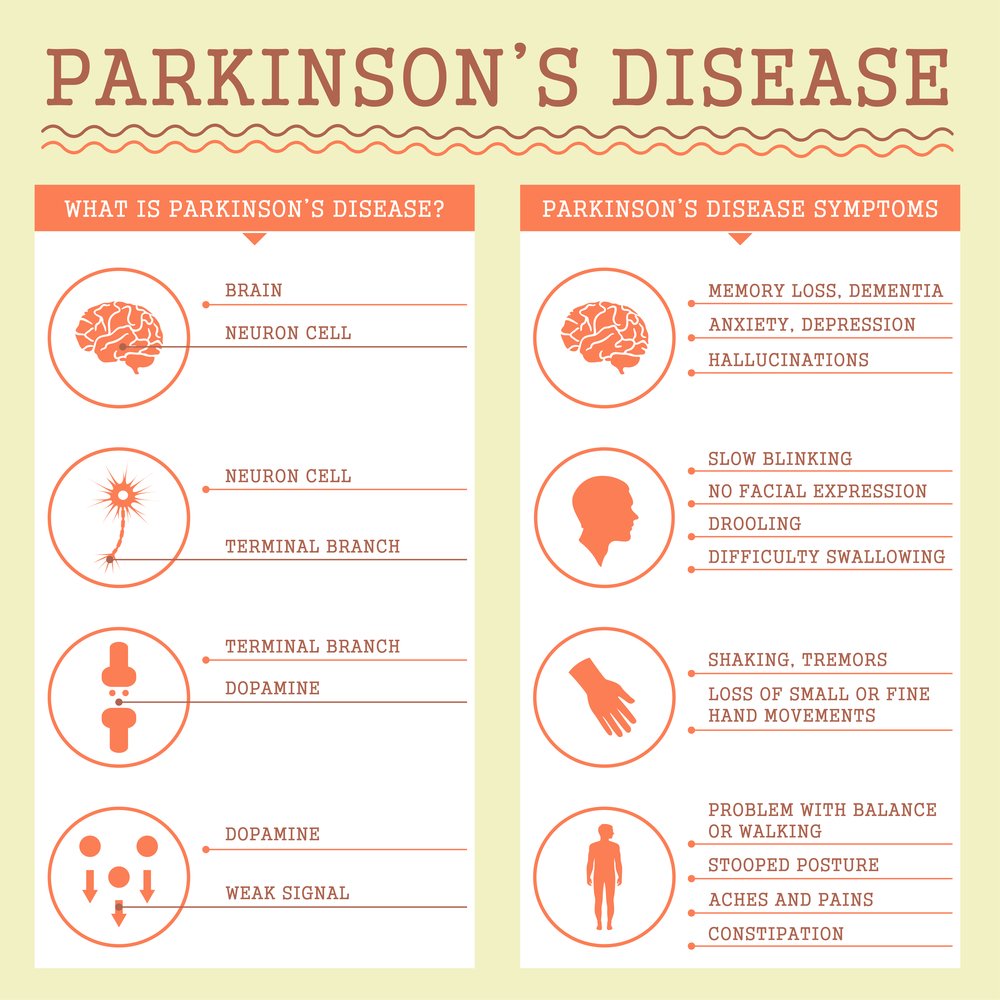
Motor And Nonmotor Symptoms Of Pd
At its core, PD is characterized by four cardinal symptoms: bradykinesia, rigidity, resting tremor, and postural instability.4 Along with these typical motor symptoms come many nonmotor symptoms with significant associated morbidity and mortality. These include autonomic dysfunction, disorders of sleep and wakefulness, cognitive dysfunction and dementia, mood disorders, and psychosis.5 These nonmotor symptoms of PD are responsible for a significant proportion of hospitalizations, with psychosis reportedly accounting for 24% of hospital admissions in patients with PD.6 This fact signifies the importance of properly managing patients with PD psychosis on both an inpatient and an outpatient basis.6
Recommended Reading: How To Tell The Difference Between Essential Tremor And Parkinsons
Don’t Miss: Medicine For Parkinson’s Hallucinations
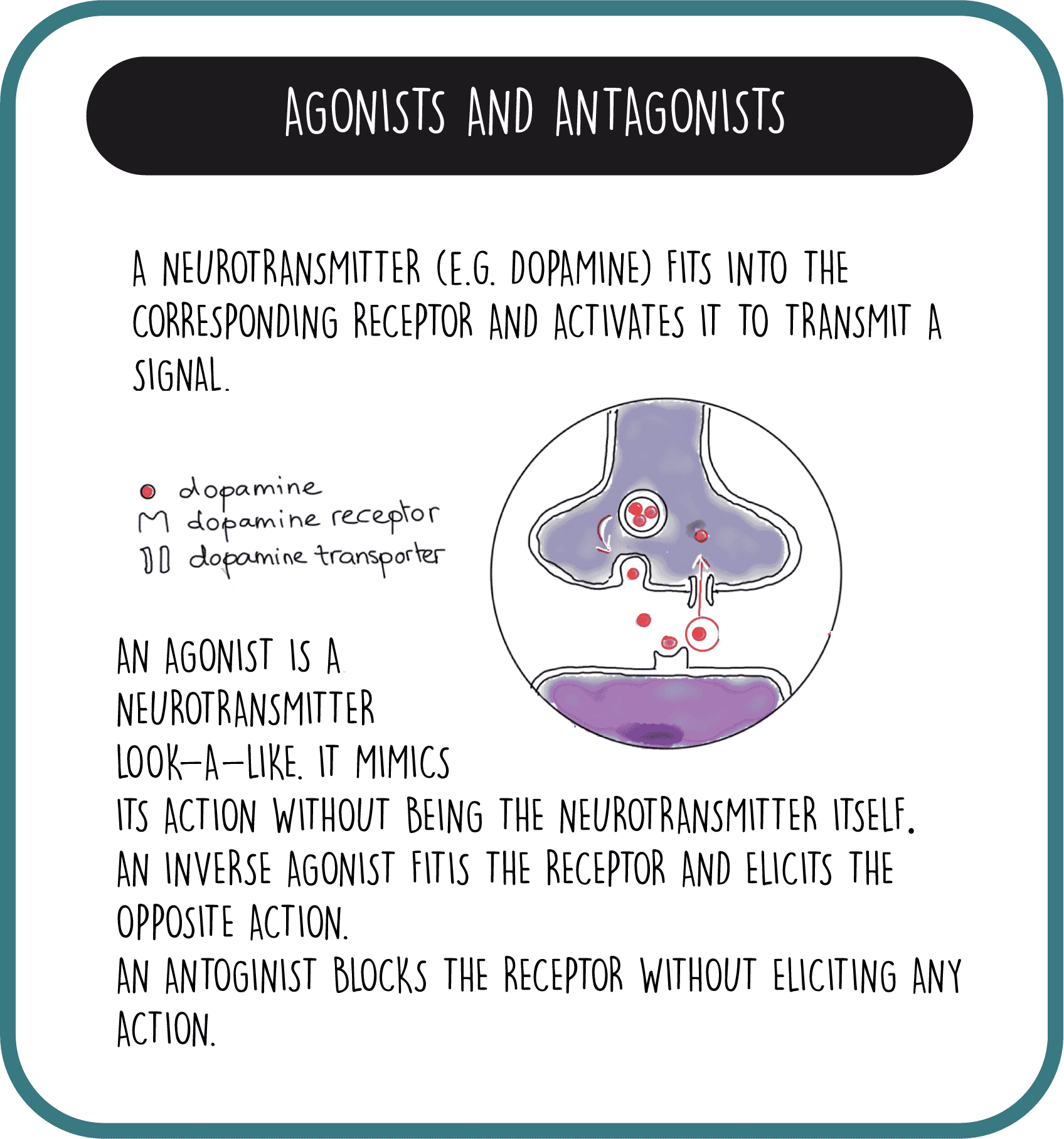
Pathology Of Neurotransmitter Pathways In Pd Psychosis And Relevance Of Medications
The distribution of pathology in PD involves key components of dopaminergic and other important neurotransmitter pathways implicated in PD psychosis. Dopamine is synthesized in the substantia nigra, with projections to the striatum, limbic system and frontal lobe , and five recognized dopamine receptors with broad distribution throughout the brain and peripheries at varying levels of expression . It is known that dopaminergic medications have differential actions across these receptors, and, similarly, antipsychotic medications display different binding affinities for individual dopamine receptors .
While loss of dopaminergic neurons within the substantia nigra is a central pathological feature of PD , neuronal loss also occurs in multiple other subcortical nuclei with projections to cortical, limbic, and basal ganglia regions. These include the dopaminergic nuclei of the ventral tegmentum, noradrenergic locus coeruleus, serotonergic raphe nuclei, histaminergic tuberomammillary nucleus of the hypothalamus, and cholinergic nucleus basalis of Meynert and the pedunculopontine nucleus . LB deposition and neuronal loss in the locus coeruleus occurs earlier and is more prominent than PD pathology in the substantia nigra, with some evidence that pathology in this region may contribute to subsequent dopaminergic cell loss, because noradrenergic neurons directly innervate the substantia nigra .
Network Changes And Thalamic Drivers
Visual hallucinations have fascinated neurologists and neuroscientists for many years, with their tantalisingly rich and often narrative detail. Due to their transient nature, they have been challenging to investigate, with no clear mechanism found, but many theories have been proposed. Previous models for visual hallucinations considered them as cortical release phenomena, where spontaneous activity occurs in the absence of visual stimuli. Alternative models suggested that hallucinations arise due to incorrect binding of objects into visual scenes.
Advances in computational modelling and network neuroscience have opened up approaches to understanding the brain in new ways. Recent models suggest that Parkinsons hallucinations could arise due to a shift in dominance of difference networks. Specifically, there is thought to be a breakdown in those networks directed to attention and perception, and overactivity of the default mode network ,, a large-scale network that becomes activated during rest, and in day dreaming and mind-wandering. Indeed abnormal levels of default mode network activation are seen in patients with Parkinsons hallucinations.
Adapted from Zarkali A, Adams RA, Psarras S, Leyland LA, Rees G, Weil RS. Increased weighting on prior knowledge in Lewy body-associated visual hallucinations. Brain Commun. 2019 1:fcz007. doi:10.1093/braincomms/fcz007
Also Check: How Long Do Parkinsons Patients Live After Diagnosis
Don’t Miss: When Parkinson’s Gets Worse
Delusions From Parkinsons Disease
Delusions affect only about 8 percent of people living with PD. Delusions can be more complex than hallucinations. They may be more difficult to treat.
Delusions often start as confusion that develops into clear ideas that arent based on reality. Examples of the types of delusions people with PD experience include:
- Jealousy or possessiveness. The person believes someone in their life is being unfaithful or disloyal.
- Persecutory. They believe that someone is out to get them or harm them in some way.
- Somatic. They believe they have an injury or other medical problem.
- Guilt. The person with PD has feelings of guilt not based in real behaviors or actions.
- Mixed delusions. They experience multiple types of delusions.
Paranoia, jealousy, and persecution are the most commonly reported delusions. They can pose a safety risk to caregivers and to the person with PD themselves.
PD isnt fatal, though complications from the disease can contribute to a shorter expected life span.
Dementia and other psychosis symptoms like hallucinations and delusions do contribute to increased hospitalizations and increased rates of death .
One study from 2010 found that people with PD who experienced delusions, hallucinations, or other psychosis symptoms were about 50 percent more likely to die early than those without these symptoms.
But early prevention of the development of psychosis symptoms may help increase life expectancy in people with PD.
Section Header Managing Psychosis With Medication
Dont keep hallucinations or delusions a secret from your doctor. Medications — or changes to the medications you take — can help manage Parkinsons psychosis.
Streamlining your meds. The first thing your doctor may want to do is stop or lower your Parkinsons medication dose. They may boost dopamine levels in your brain. That improves motor symptoms but can also cause changes in your emotions or the way you act.
Antipsychotics. These medications balance your brain chemicals. Only a few are considered safe for people with Parkinsons disease. These include quetiapine and clozapine .
Pimavanserin . Another antipsychotic, this first-in-class drug was approved by the FDA in 2016 to treat hallucinations and delusions in Parkinsons disease linked with psychosis.
If you see a doctor who isnt part of your usual care team — say, in the emergency room or an urgent care setting — tell them you have Parkinsons disease and what medications you take for it.
Also Check: Is Essential Tremor Related To Parkinson’s Disease
Treatment Of Parkinsons Disease Psychosis
Andrew Schleisman, PharmD Candidate 2017
Mikayla Spangler, PharmD, BCPSAssociate Professor of Pharmacy Practice
Emily Knezevich, PharmD, BCPS, CDEAssociate Professor of Pharmacy PracticeCreighton University School of Pharmacy and Health ProfessionsOmaha, Nebraska
US Pharm. 2016 41:HS20-HS26.
ABSTRACT: Delusions and hallucinations in patients with Parkinsons disease, a condition known as Parkinsons disease psychosis , have historically been treated with clozapine and quetiapine because of their relatively low likelihood of worsening motor symptoms. Although clozapine is considered the drug of choice, it is underused in this population because of the need for frequent monitoring. Quetiapine, on the other hand, is generally first-line treatment despite its questionable efficacy. Consequently, in 2006, the American Academy of Neurology identified a need for the development of a novel antipsychotic with evidence of both safety and efficacy in patients with PDP. Pimavanserin, which has shown promise in clinical trials, recently became the first agent to receive FDA approval for the treatment of PDP.
Hallucinations And Rem Sleep Disorders In Parkinsons Disease
At timestamp 1:58 in this recording of Thrive: HAPS 2020 Caregiver Conference, you will find a one hour talk by neurologist Joohi Jimenez-Shahed, MD. In it she delves into what REM sleep behavior disorder is and is not, and the distinctions between hallucinations, delusions, and delirium. Managment options for RBD and hallucinations are included.
Read Also: Can Restless Leg Syndrome Be A Sign Of Parkinson’s
New Drug Shows Promise In Treating Parkinson’s Disease Psychosis
Off-label drugs have been used to manage psychotic-related symptoms in Parkinson’s disease patients, but they worsen motor symptoms by reducing dopamine levels. Nuplazid is the only FDA-approved drug that treats Parkinson’s disease psychosis without impairing motor function.
Parkinson’s disease is a progressive neurodegenerative condition marked by bradykinesia, rigidity, tremor, and postural instability. While therapeutic advances have been made to improve motor-related symptoms, many older adults affected by this disease also develop Parkinson’s disease psychosis . Psychotic symptoms such as hallucinations and delusions develop in more than 50% of PD patients and can lead to severe impairments in cognitive, behavioral, and emotional function.1
PDP Drives Nursing Home Placement According to the Parkinson’s Disease Foundation, 1 million people have been diagnosed with PD in the United States, and between 7 million and 10 million people worldwide have the condition. Hallucinations and delusions drive the nursing home placement and hospitalization of patients diagnosed with PDP, says Jason Kellogg, MD, chief of staff at Newport Bay Hospital in Newport Beach, California.
He adds that the delusions and hallucinations observed in PDP tend to be more dramatic in nature. For instance, these patients are usually high-functioning, well-dressed men and women. But their hallucinations are quite striking because they have delusions of persecution and visual hallucinations.
Practical Tips For Caregivers Of People With Parkinson’s Psychosis
This 2-page tip sheet has bullet point suggestions for what to do if the person you care for experiences hallucination, delusions or confusion, or becomes agitated or aggressive. In addition, there are tips for how to best be prepared for a doctors appointment when you bring this behavior to the attention of your medical team.
Read Also: How To Test For Early Onset Parkinson’s
New Drug Shows Promise In Treating Parkinsons Disease Psychosis
Off-label drugs have been used to manage psychotic-related symptoms in Parkinsons disease patients, but they worsen motor symptoms by reducing dopamine levels. Nuplazid is the only FDA-approved drug that treats Parkinsons disease psychosis without impairing motor function.
Parkinsons disease is a progressive neurodegenerative condition marked by bradykinesia, rigidity, tremor, and postural instability. While therapeutic advances have been made to improve motor-related symptoms, many older adults affected by this disease also develop Parkinsons disease psychosis . Psychotic symptoms such as hallucinations and delusions develop in more than 50% of PD patients and can lead to severe impairments in cognitive, behavioral, and emotional function.1
PDP Drives Nursing Home Placement According to the Parkinsons Disease Foundation, 1 million people have been diagnosed with PD in the United States, and between 7 million and 10 million people worldwide have the condition. Hallucinations and delusions drive the nursing home placement and hospitalization of patients diagnosed with PDP, says Jason Kellogg, MD, chief of staff at Newport Bay Hospital in Newport Beach, California.
He adds that the delusions and hallucinations observed in PDP tend to be more dramatic in nature. For instance, these patients are usually high-functioning, well-dressed men and women. But their hallucinations are quite striking because they have delusions of persecution and visual hallucinations.
Management Of Visual Hallucinations In Pd
Understanding the complex interactions between neurotransmitter systems in the context of neurodegeneration secondary to PD assists in efforts to treat psychotic symptoms as they arise. Management is complex and varies between patients. The first consideration should most obviously be prevention. When these symptoms occur acutely, systemic illness should be considered and treated. When symptoms persist, an increasing array of treatment options are available and can be tailored to the individual patient. A treatment algorithm is presented in .
FIGURE 1. Management flow chart for visual hallucinations in Parkinsons diseasea
a COMT=catechol-O-methyltransferase.
Also Check: Is Constipation A Symptom Of Parkinson’s
Risk Factors For Parkinsons Psychosis
Understanding the risk factors for hallucinations and delusions can help you recognize symptoms of Parkinsons psychosis. The following factors may increase the likelihood of experiencing hallucinations and delusions:
- Advancing cognitive impairment, including worsening memory loss
- History of depression
- Sleep disorders and sleep disturbances
- Changes to medications
- Worsening medical conditions outside of Parkinsons
We have noticed that when my father had delusions, its been when his general health is not good, or when he has been in the hospital for PD-related issues, a MyParkinsonsTeam member commented.
Questionnaires used in a clinical setting can help assess the risk of developing hallucinations or delusions, or establish that they are occuring. These include:
- PD nonmotor symptom scale
- Parkinson Psychosis Questionnaire
- Scale for Evaluation of Neuropsychiatric Disorders in Parkinsons Disease
Individuals with Parkinsons or their caregivers can speak with a neurologist to understand if any of these tools would be helpful in their particular situation.
You May Like: What Happens To You When You Have Parkinsons Disease
Treatment And Management Of Hallucinations
You should discuss any hallucinations or delusions with your doctor, or Parkinsons nurse if you have one, so that all treatment options can be considered.
In mild cases no specific action may be required and simple reassurance that the images, sensations or sounds are harmless may be all that is needed.
Also Check: Parkinson’s How Fast Does It Progress