How Parkinsons Disease Affects The Brain
The Parkinson’s disease brain stops producing dopamine cells, which in turn causes problems with movement and coordination known as motor symptoms. We all have a basic understanding of how Parkinson’s disease affects the brain, but what really happens when someone has Parkinson’s disease? Let’s explore the facts surrounding the Parkinson’s disease brain and how it differs from a normal, “healthy” brain.
Preparing For A Parkinsons Mri
A Parkinsons MRI is completely painless, but you do have to lie still while being scanned. Some patients feel claustrophobic in this situation. If youre worried about that, talk with your doctor about the possibility of having an anti-anxiety medication before the procedure.
On the day of the appointment, follow any instructions provided to you by your doctor. Remove metal jewelry and dont wear make-up as that can also have metal in it. If you are in the advanced stages of Parkinsons or if you are taking a sedative, you should arrange transportation to and from the appointment.
So What Do We Know So Far
Location of the substantia nigra. FrozenManCC BY-SA 4.0
The substantia nigra is an area of the mid brain located at the top of the spinal cord, which has been the focus of much work into how Parkinsons affects the brain.
There are a right and a left substantia nigra, and often one side is affected before the other. Because of this, people with Parkinsons often experience symptoms primarily on one side of their body, particularly in the early stages. Indeed, this common feature of the condition often helps to distinguish Parkinsons from other similar conditions.
When it comes to confirming a diagnosis, it is the substantia nigra where pathologists look for changes at the end of life in brain tissue that has been donated to research. And the loss of the dopamine-producing cells in this area of the brain, accompanied by the presence of clumps of alpha-synuclein protein , has been the hallmark of Parkinsons for decades.
You can read more about the alpha-synuclein protein, and how it plays a role in the spread of Parkinsons, in a previous blog post:
Don’t Miss: Who Discovered Parkinson’s Disease
When People Talk About Parkinsons They May Mention The Effects It Has On The Substantia Nigra But Did You Know That There Are Other Areas Of The Brain That Are Affected By The Condition
Parkinsons is a condition that causes the gradual loss of the dopamine-producing brain cells of the substantia nigra an area of the brain located just above where the spinal cord meets the midbrain. It is these cells that produce and release the neurotransmitter dopamine, which has a key role in turning thought about movement into action.
While this definition of the condition is useful to briefly explain Parkinsons, the whole story is somewhat more complex. Over the last 30 years, it has become accepted that Parkinsons also causes a number of non-motor symptoms, such as changes in sleep, smell and even the way we think, which likely involve other areas of the brain.
Now scientists are looking at the broader effects of the condition on the brain in an attempt to better understand why people experience different symptoms. The finding could lead us to new treatments that tackle more than just the motor symptoms of the condition.
What Can You Detect With A Parkinsons Mri
Generally, you can receive a Parkinsons diagnosis in a clinical setting, but an MRI can help to assess various aspects of the disease and its progress. In particular, a Parkinsons MRI can do the following for patients who have or are suspected to have Parkinsons disease:
- Evaluate tissue loss and how the brain is atrophying
- Check for changes to the basal ganglia region of the brain
- Find out if there are abnormal iron deposits in the basal ganglia or brainstem
- Look at changes to white matter
- Examine the diffusion of restricted tissues in acute infarction and neurodegenerative diseases
- Help to diagnose atypical parkinsonism
- Exclude treatable causes of parkinsonism such as normal pressure hydrocephalus
You May Like: Parkinson’s Life Center Of Southern New Jersey
How Parkinsons Disease Affects The Autonomic Nervous System And The Heart
In PD, there are two major reasons why the automatic control of the cardiac system is impaired. First, areas of the brain that control this system often contain Lewy bodies and have undergone neurodegeneration. In addition, the autonomic nervous system itself is directly affected by Lewy body-like accumulations and neurodegeneration. This means, when the baroreceptors in the heart and carotid artery sense a drop in blood pressure and try to generate a signal to the heart and blood vessels to increase the blood pressure, the message may not get through. This results in neurogenic orthostatic hypotension , or drops in blood pressure upon standing due to autonomic nervous system dysfunction. There are no medications that can cure nOH by restoring the autonomic nervous system in PD. nOH however, can be treated. Read more about nOH and its treatments here.
Structural problems of the heart such as coronary artery disease or cardiomyopathy are not thought to be part of the pathology of PD, although of course, could co-exist with PD.
Read Also: Effect Of Exercise On Parkinsons Disease
What Causes Parkinsons Disease
We do not know what causes Parkinsons disease. There is some evidence to suggest that there is a genetic factor which increases the risk of Parkinsons disease within some families. Also, there might be an increased risk if people have come into contact with a particular toxin or toxins found in the environment via pesticides and other chemicals used in agriculture. The specific toxin or toxins have not yet been identified but there is ongoing research into this possible cause.
Recommended Reading: Alternative Treatment For Parkinson’s Disease
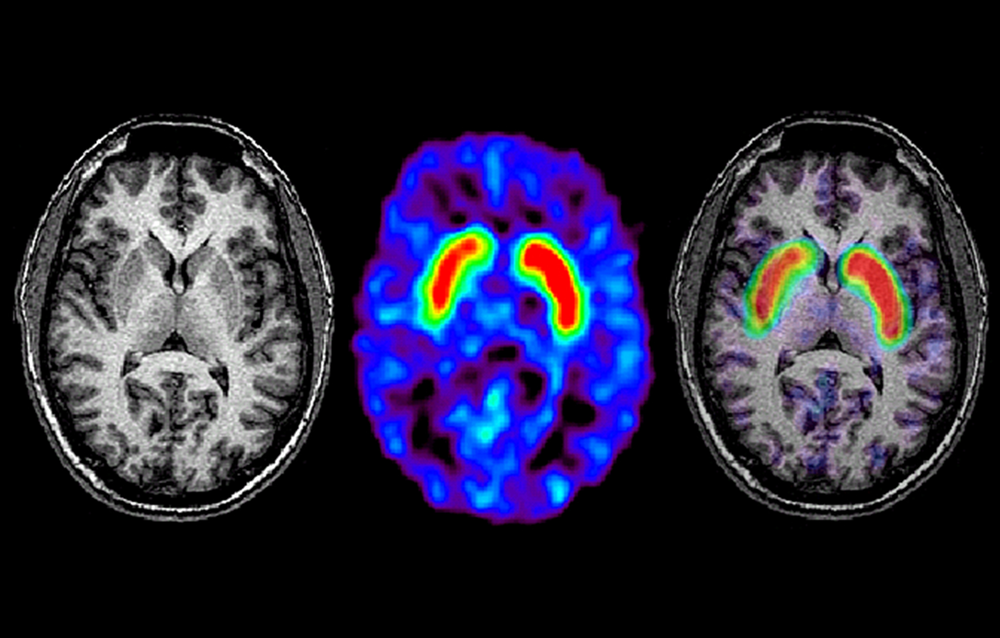
Structural And Functional Imaging
Traditional structural imaging modalities, such as X-ray computed tomography and brain MRI using anatomical T1 or T2-weighted sequences, are limited to use for identifying the dopaminergic deficits in the brain of patients with PD. However, MRI can be useful in the identification of structural lesions associated with other forms of parkinsonism, such as those underlined by vascular pathology or neoplasms. Structural MRI can also be useful for measuring the degree and distribution of brain atrophy. With regards to differential diagnosis, it has been shown that abnormal T2 MRI hypo-intensities in the putamen discriminate MSA-P from PD with 88% sensitivity and 89% specificity. Decreased putaminal signal intensities were higher using T2*-weighted gradient echo than T2-weighted fast-spin echo sequences and more useful in differentiating PD from MSA-P. Atrophy of the superior cerebellar peduncles and the frontal cortex also aid in discriminating PSP from PD with 74/94% and 95/91% specificity/sensitivity, respectively .
Diagnostic accuracy of MRI modalities.
Exclusion Of Alternative Diagnoses
Structural MRI with conventional MR sequences is usually normal in early PD patients limiting its application in clinical routine for the detection of early PD. Recent studies, however, identified imaging correlates of underlying neuropathology in PD patients through advanced MRI techniques. These imaging abnormalities will be discussed in detail later in this review. Nevertheless, cMRI was repetitively shown to be useful in discriminating PD from APDs such as MSA and PSP. Latter are characterized by disease-specific atrophy patterns and signal intensity changes. In addition, current operational diagnostic criteria require the exclusion of symptomatic causes of parkinsonism in the work-up of patients with PD .
Also Check: Parkinson’s Disease And Sleep
Brain Mri Tracks Parkinsons Progression
All Science News articles summarize a research study and are not an official opinion, endorsement or position of the Parkinsons Foundations.
Researchers at a Parkinsons Foundation Center of Excellence have found that a brain MRI that uses a special protocol can track changes that occur as Parkinsons disease progresses. This biomarker could be used in clinical trials, as an objective way to monitor whether the therapies being tested are effective. The study appears in the August 2017 issue of Brain.
Doctors currently diagnose PD based on a persons symptoms slowness, stiffness, tremor and balance difficulties. But these symptoms, and the rate at which they progress, differ from person to person. And there is no blood test, or biomarker, to definitively diagnose PD or objectively monitor underlying biological changes as PD progresses. Currently, a brain MRI may be ordered to rule out other conditions, but cannot diagnose PD or monitor its progression.
In earlier research, scientists led by David Vaillancourt, Ph.D., at the University of Florida in Gainesville a Parkinsons Foundation Center of Excellence, used a brain scanning technique called diffusion MRI to detect changes that happen only in the brains of people with PD. The scans showed an increase in free water water outside of brain cells in a part of the brain called the substantia nigra.
Results
What Does It Mean?
Approach To Imaging Interpretation: Multimodal Mri And Advanced Imaging Analysis
Recent research on PD and APD MRI markers has had prolific results. However, the discovery of a single perfect marker is unlikely. Therefore, a multimodal approach to image analysis emerges as the answer to overcoming single parameter limitations. For instance, combined evaluation of iron- and NM-sensitive MRIs may detect changes in the SN with higher sensitivity. Simultaneous measurement of volumes, T2* relaxation rates, and diffusion in nigrostriatal structures also seem better for separating PD, PSP, and MSA.-
Also Check: Exercise Class For Parkinson’s Disease
Differences Between Parkinsons Disease And Atypical Parkinsonism
The symptoms of Parkinsons disease and atypical parkinsonism overlap, and in a clinical setting, it can be hard to tell if a patient has one or the other. Atypical parkinsonism is diseases that present some of the signs and symptoms of Parkinsons Disease but do not respond well to drug treatment. With an MRI, your doctor can help to make the diagnosis more accurate, which is essential for quality treatment. Additionally, an MRI can also help your medical team to determine if you have a certain type of atypical parkinsonism. This can help to create a prognosis and guide your treatment options.
What Is Parkinson’s And How Can Mri Help
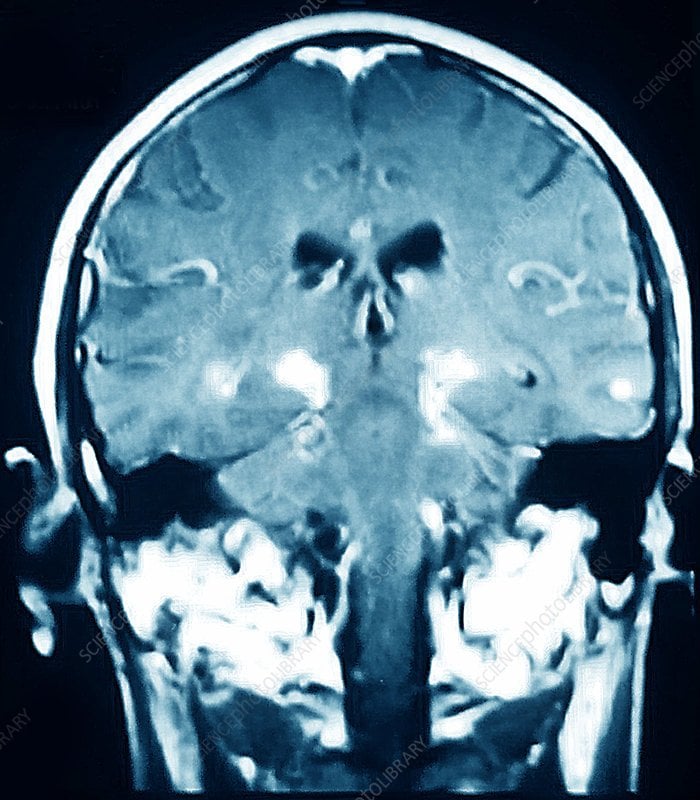
More than ten million people are living with Parkinson’s disease worldwide, with about one million cases expected to be in the United States by 2020.1 This is more than the number of people with multiple sclerosis, muscular dystrophy and Lou Gehrig’s disease combined.1 With the rising prevalence of Parkinson’s disease, its important to understand the signs and symptoms of the disease. Likewise, physicians and radiology departments may need to know what role magnetic resonance imaging may play.
You May Like: Is Parkinson’s Disease Related To Alzheimer’s
Is The Imaging Metric Appropriate For The Question Being Asked
Neuroanatomy Relevant to Parkinsons Disease
A. Braak staging of -synuclein pathology. At death, PD patients exhibit the following stages of -Syn pathology: stage I olfactory bulb only , Stage IIa brainstem predominant , stage IIb limbic predominant , stage III brainstem and limbic and stage IV neocortical . While not all patients with pathology will exhibit clinical symptoms , the progression of neuropathology generally corresponds to the progression of both motor and non-motor symptoms . B. The SN is subdivided into the ventral pars reticulata and the dorsal pars compacta , the latter is composed of dopaminergic neurons. The SNc is further divided into the dorsal and ventral tier, with the loss of dopaminergic neurons occurring first in the caudal and ventrolateral tier . Within A9, there are five nigrosomes , with N1 exhibiting the earliest loss of dopaminergic neurons . Dopaminergic neuronal loss typically spreads to neighboring groups from the N1 in PD . C. Fronto-subcortical loops comprise the motor, associative, and limbic domains, which respectively transit through the posterior, anterior, and ventral striatum, thus segregated functionally and anatomically. GPe = globus pallidus externa. GPi = globus pallidus interna. STN = subthalamic nucleus. SNc = substantia nigra pars compacta. SNr = substantia nigra pars reticulata. Adapted with permission from: .
Is Parkinson’s Diagnosed In The Brain
Parkinson’s disease is one of the most challenging neurological disorders to diagnose and treat. If your doctor suspects you have Parkinson’s disease, you will usually be referred to a neurologist for further tests. These tests will involve certain movements and exercises to check your symptoms.
A neurologist will look for motor symptoms such as:
- A tremor that occurs at rest
- Slowed movement
- Muscle stiffness
If you have two or more of these symptoms and your doctor has taken blood tests to rule out other causes, it’s likely you will be diagnosed with Parkinson’s disease. Your symptoms will be closely monitored to see any progression of Parkinson’s disease, which can take years.
Recommended Reading: Clinical Trials On Parkinson’s Disease
Group Differences In Dat Neuromelanin And Iron
Group differences in striatal DaT levels. Functional subregions in the striatum. Left and right panels show the results of the statistical comparison between groups in the clinically most and least affected brain hemispheres, respectively. Each panel has three columns, representing the intergroup comparison between Parkinsons disease patients and healthy control subjects , Parkinsons disease patients and iRBD patients or iRBD patients and healthy control subjects . Rows correspond to the group differences at visit 1 visit 2 and the inter-visit differences in longitudinal subjects. Results were adjusted for age and sex and corrected for multiple comparisons using Tukeys test at the P< 0.05 level. For improved clarity in the visual representation of statistical differences, P-values were converted into z-scores. Cd = caudate nucleus NAc = nucleus accumbens Pu = putamen
Scatter box plots of DaT-SBR measurements in the striatum and neuromelanin SNR and QSM measurements in the SNc are shown in Supplementary Figs 113.
Brain Mri Advances For Parkinsons Disease
In Parkinsons disease, the damage to brain cells begins long before any symptoms develop. Therefore, at-risk patients can benefit from early diagnosis, and efforts to slow the progression of the disease can start early.
Researchers are working on newer MRI approaches to precisely detect Parkinsons disease-related structural and metabolic activity in the brain and correlate it to the function of the organ. For example, scientists from Oxford University used a technique called the resting-state functional MRI to assess the strength of nerve cells in the a region of the brain called the basal ganglia to send and receive information. Because the physical signs of brain cell damage in Parkinsons disease are not recognizable by conventional MRI, this approach may help visualize the impact of the damage on the activity of brain cells and aid in early diagnosis.
Similarly, MRI is used to identify Parkinsons disease-specific biomarkers. Tracking the biomarkers using high-field and ultra-high field MRI can identify Parkinsons disease patients and help follow the progression of the condition.
Although many of these advancements are yet to be implemented in the clinical setting, such adaptations may help better understand the disease and develop new treatments.
Read Also: How Hereditary Is Parkinson’s Disease
What Is Parkinsons Disease
Parkinsons disease is a chronic neurological condition. It is progressive and symptoms worsen over time. It is named after Dr James Parkinson who first described the condition in 1817.
People with Parkinsons disease experience a loss of nerve cells in the part of their brains responsible for controlling voluntary movements. This part of the brain is called the substantia nigra . The nerve cells in the substantia nigra usually produce a chemical called dopamine which helps transmit messages from the brain to the rest of the body via the central nervous system . As these cells are lost, people with Parkinsons disease experience a loss of dopamine and the messages controlling movement stop being transmitted efficiently.
Parkinsons disease is more common as people get older but it can affect younger adults. Men tend to be affected in slightly higher numbers than women.
The Cerebellum And Parkinsonian Akinesia/rigidity
Parkinsons disease is not a homogenous disease and has two predominant forms: akinesia and rigidity and prominent resting tremor . Akinesia can be defined as a delay or a failure in movement initiation , particularly for self-initiated movements. Functional neuroimaging studies using PET or blood oxygen leveldependent functional MRI frequently demonstrated increased activation in the cerebellum in patients with Parkinsons disease during performance of various upper limb movements . For example, during externally or internally timed simple finger movements , motor timing , complex sequential movements , bimanual two-hand coordinated tasks or two different motor tasks simultaneously , patients with Parkinsons disease OFF medication showed hyperactivation in the cerebellum.
Brain areas more activated in patients with Parkinsons disease than in normal subjects during automatic execution of sequential movements. Modified from, with permission from Oxford University Press.
The neurodegenerative process in Parkinsons disease begins several years before the onset of any clinical symptoms . The motor symptoms of Parkinsons disease usually present after 70% of dopaminergic neurons have degenerated . Presumably, the compensatory effect in the cerebellum and other brain regions accounts for delaying the onset of motor symptoms and preserving relatively normal function.
Read Also: Can Parkinson’s Psychosis Be Reversed
Role Of Imaging In Parkinsonian Syndromes
Despite well-established Parkinson’s disease diagnostic criteria, diagnosis can still be challenging, with a high rate of misdiagnosis in atypical cases, especially in early disease stages., The majority of misdiagnoses are related to the differential diagnosis of PD with atypical parkinsonian disorders , such as multiple system atrophyparkinsonian type , progressive supranuclear palsy , or corticobasal degeneration, as well as essential tremor and other forms of parkinsonism .
Early diagnosis is of crucial importance for both individual patients in clinical practice and for research purposes, as it enables not only the implementation of adequate therapeutic plans and a definition of prognosis, but also a more appropriate selection of patients for clinical trials, particularly with the increase of disease-modifying trials for PD, MSA, and PSP.,