Medicines For Parkinson’s Disease
Medicines prescribed for Parkinson’s include:
- Drugs that increase the level of dopamine in the brain
- Drugs that affect other brain chemicals in the body
- Drugs that help control nonmotor symptoms
The main therapy for Parkinson’s is levodopa, also called L-dopa. Nerve cells use levodopa to make dopamine to replenish the brain’s dwindling supply. Usually, people take levodopa along with another medication called carbidopa. Carbidopa prevents or reduces some of the side effects of levodopa therapysuch as nausea, vomiting, low blood pressure, and restlessnessand reduces the amount of levodopa needed to improve symptoms.
People with Parkinson’s should never stop taking levodopa without telling their doctor. Suddenly stopping the drug may have serious side effects, such as being unable to move or having difficulty breathing.
Other medicines used to treat Parkinsons symptoms include:
- Dopamine agonists to mimic the role of dopamine in the brain
- MAO-B inhibitors to slow down an enzyme that breaks down dopamine in the brain
- COMT inhibitors to help break down dopamine
- Amantadine, an old antiviral drug, to reduce involuntary movements
- Anticholinergic drugs to reduce tremors and muscle rigidity
Behaviors Seen In Parkinsons Disease Dementia
As dementia progresses, managing disorientation, confusion, agitation, and impulsivity can be a key component of care.
Some patients experience hallucinations or delusions as a complication of Parkinsons disease. These may be frightening and debilitating. Approximately 50 percent of those with the disease may experience them.
The best thing to do when giving care to someone experiencing hallucinations or delusions from Parkinsons disease dementia is to keep them calm and reduce their stress.
Take note of their symptoms and what they were doing before they exhibited signs of hallucinating and then let their doctor know.
This element of the disease can be particularly challenging for caregivers. Patients may become unable to care for themselves or be left alone.
Some ways to make caregiving easier include:
- sticking to a normal routine whenever possible
- being extra comforting after any medical procedures
- limiting distractions
- using curtains, nightlights, and clocks to help stick to a regular sleep schedule
- remembering that the behaviors are a factor of the disease and not the person
Tissue Changes Reflecting Poorer Cognition
We showed that cognition assessed with the MoCA correlated with magnetic susceptibility in hippocampus and thalami, as well as ventromedial prefrontal cortices, basal forebrain and rostral caudate nucleus. Previous studies using conventional structural measures report varying patterns of grey matter atrophy in patients with early cognitive change in PD with several showing no atrophy changes. Hippocampal atrophy is reported in cross-sectional studies in PD, and is the most consistently abnormal region in longitudinal structural MRI. Thalamic changes are also linked with cognition in PD. However, a significant relationship between MoCA and grey matter volume has not been shown in PD.
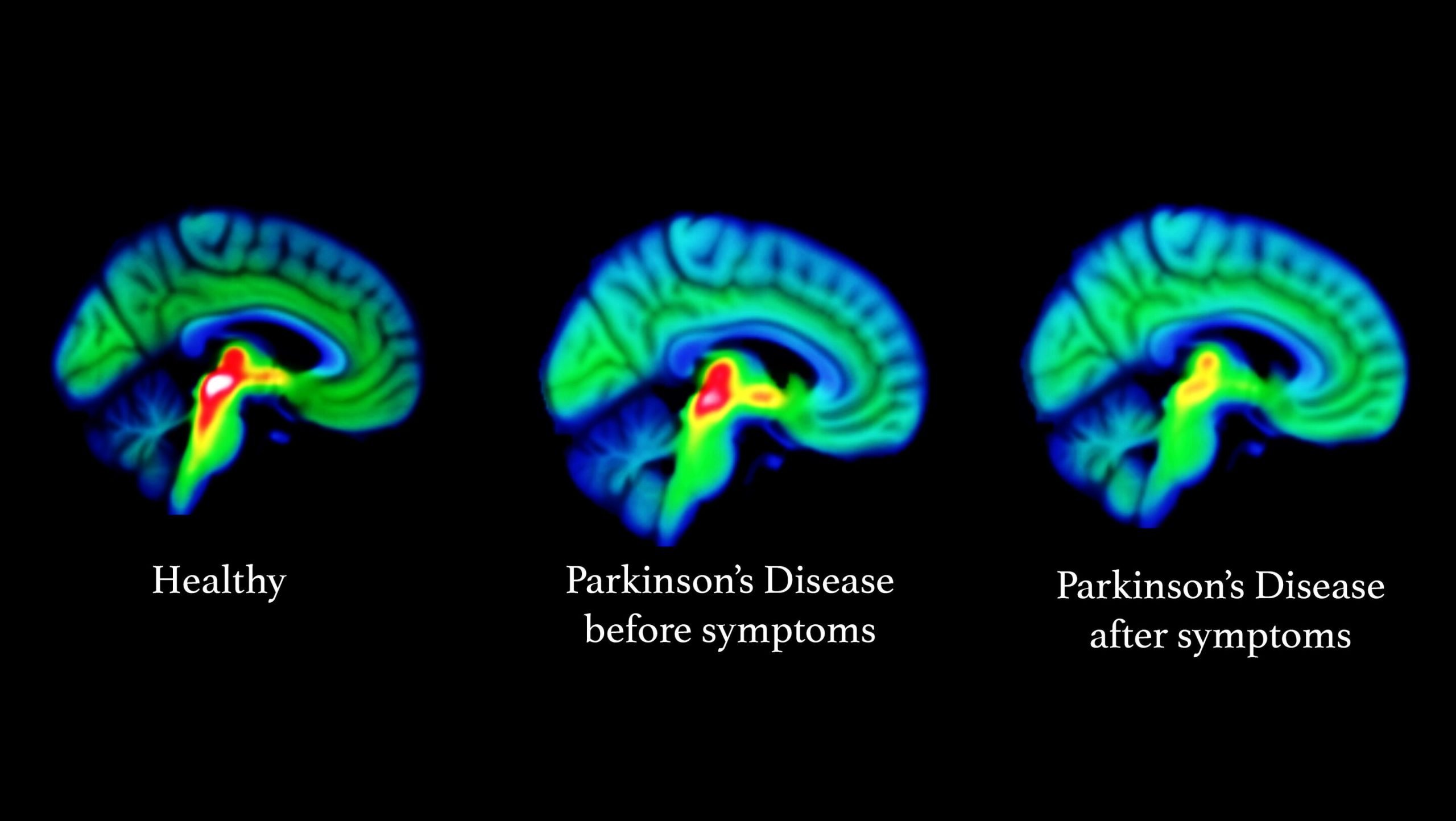
We also found QSM increases with lower MoCA scores in the caudate nucleus. This is consistent with findings in other modalities functional MRI caudate activation is reduced during memory tasks in PD-MCI and cognitive decline in PD is linked to lower caudate uptake in dopamine transporter single-photon emission computed tomography and positron emission tomography imaging. We found QSM increases in basal forebrain with lower MoCA scores, although not in the substantia innominata . The substantia innominata is the major source of cholinergic innervation to the cerebral cortex and shows post-mortem cell depletion and Lewy-related pathology in Parkinsons dementia. The lack of covariance here could suggest this is a later event in Parkinsons dementia.
Recommended Reading: Is Massage Good For Parkinson’s
So What Do We Know So Far
Location of the substantia nigra. FrozenManCC BY-SA 4.0
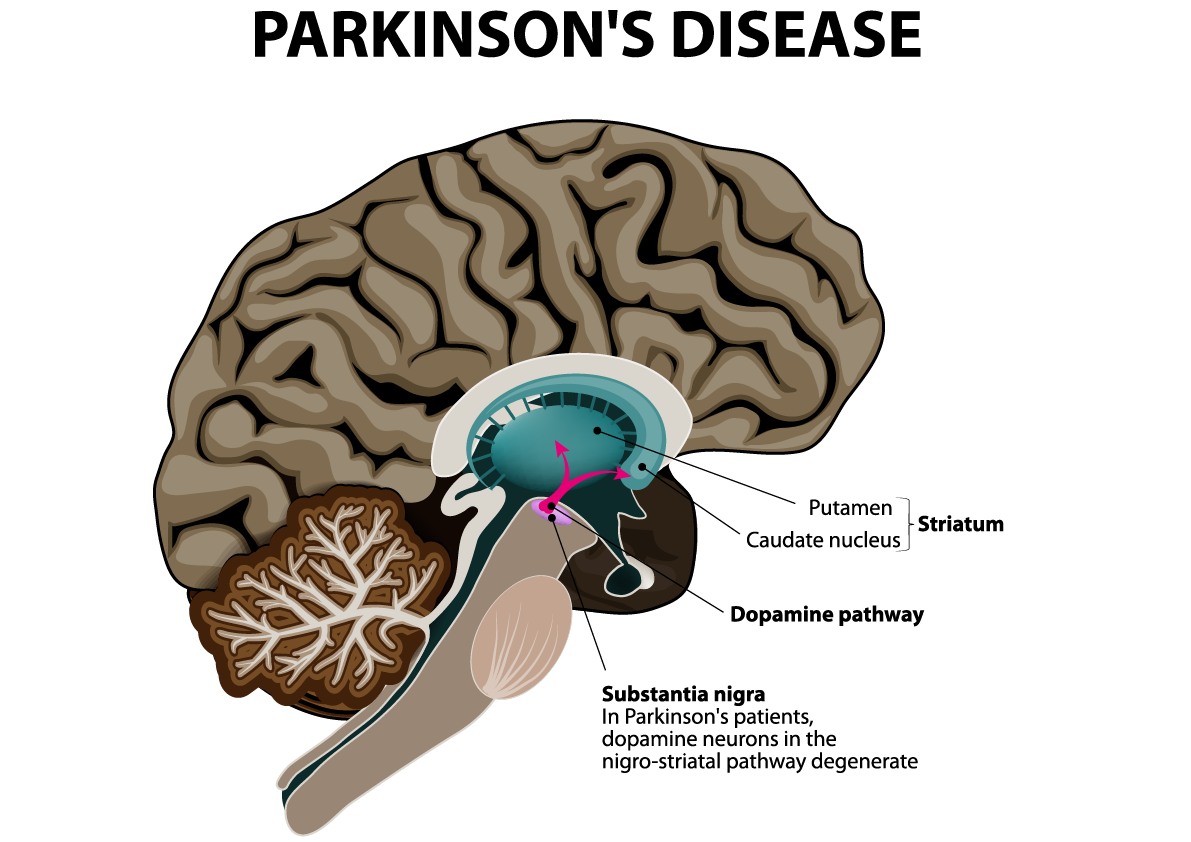
The substantia nigra is an area of the mid brain located at the top of the spinal cord, which has been the focus of much work into how Parkinsons affects the brain.
There are a right and a left substantia nigra, and often one side is affected before the other. Because of this, people with Parkinsons often experience symptoms primarily on one side of their body, particularly in the early stages. Indeed, this common feature of the condition often helps to distinguish Parkinsons from other similar conditions.
When it comes to confirming a diagnosis, it is the substantia nigra where pathologists look for changes at the end of life in brain tissue that has been donated to research. And the loss of the dopamine-producing cells in this area of the brain, accompanied by the presence of clumps of alpha-synuclein protein , has been the hallmark of Parkinsons for decades.
You can read more about the alpha-synuclein protein, and how it plays a role in the spread of Parkinsons, in a previous blog post:
Changes In Glial Cells In Parkinson’s Disease
All glial cells can influence the cognitive functions. Structural changes occur in astrocytes in response to physiological and pathological conditions may influence the neurons through nonsynaptic communication with neurons. Altered neuroglial interaction may be the underlying cause for many neurological diseases including PD. Glial response in PD offers both beneficial and hazardous effects.
Also Check: Music Therapy For Parkinson’s
What Is Alzheimer’s Disease
Alzheimer’s disease , the most common form of dementia among older adults, is an irreversible degeneration of the brain that causes disruptions in memory, cognition, personality, and other functions that eventually lead to death from complete brain failure. Genetic and environmental factors including diet, activity, smoking, traumatic brain injury, diabetes, and other medical diseases contribute to the risk of developing this form of the disease. The hallmarks of Alzheimer’s disease are the accumulation of beta-amyloid plaques between nerve cells in the brain and neurofibrillary tangles, which are twisted fibers found inside the brain’s cells). These tangles consist primarily of a protein called tau.
Ascension Sacred Heart Offers Brain Stimulation Procedure To Treat Parkinson’s Disease
Dr. Deborah Boland, a neurologist specializing in movement disorders at Ascension Sacred Heart in Pensacola, Florida
Ascension Sacred Heart Pensacola is now offering the most advanced technology for deep brain stimulation, a neurosurgical procedure to improve tremors and other symptoms of Parkinson’s disease. The surgical team was led by Dr. Deborah Boland, a neurologist specializing in movement disorders, and Dr. Ann Carr, a neurosurgeon.
“Deep brain stimulation isn’t a cure for Parkinson’s but it can reduce several of the debilitating symptoms and significantly improve daily function and quality of life for many patients,” Dr. Boland said. “We are pleased to bring the latest DBS technology and therapy to eligible patients across Northwest Florida.”
The first surgery at Ascension Sacred Heart ‘s Advanced Brain and Spine Institute was performed successfully on Oct. 13. DBS delivers mild electrical impulses to a targeted area of the brain that is responsible for the movement symptoms caused by Parkinsons disease. The electrical impulses can block or change the abnormal nerve activity that triggers symptoms.
In the multi-stage procedure, electrodes are positioned in the brain and then a device that sends the electrical pulses to the electrodes is implanted under the collarbone. A thin wire is placed underneath the skin to connect the stimulator device to the electrodes.
For more information, visit ascension.org/sacredheartneuro.
Read Also: Signs Of Parkinson’s Disease
Living Well With Parkinson’s
While medication and DBS surgery are the most effective treatments for PD, individuals often choose to delay these treatments because of their adverse side effects. Until a therapy is developed that can halt the progression of PD, there is a significant need for strategies that provide symptom relief without causing negative side effects.
Diet, Exercise, and Stress Reduction
Findings from several studies suggest that exercise has the potential to provide relief from certain PD symptoms. Anecdotally, people with Parkinsons disease who exercise typically do better. However, many questions remain. Among them is whether exercise provides a conditioning effect by strengthening muscles and improving flexibility or whether it has a direct effect on the brain.
In an NINDS-funded trial comparing the benefits of tai chi, resistance training, and stretching, tai chi was found to reduce balance impairments in people with mild-to-moderate PD. People in the tai chi group also experienced significantly fewer falls and greater improvements in their functional capacity.
Technologies that Improve Quality of Life
Brain Iron And Other Dementias
Brain tissue iron has previously been examined in patients with Alzheimers disease, using QSM, with higher levels seen in putamen as well as in amygdala and caudate and also in hippocampus, amygdala, precuneus and thalamus. An inverse correlation was also seen with poorer cognitive performance in the caudate, in a recent region of interest analysis. The distribution of susceptibility change, particularly in relation to cognitive performance, differs from that seen in our cohort, suggesting that the relationship to cognition that we found may not be entirely explained by Alzheimers pathology in our cohort. Similarly, patients with vascular dementia showed higher levels of brain susceptibility in the caudate and putamen, in a region of interest analysis. In patients with subcortical vascular mild cognitive impairment, higher susceptibility values were found in bilateral hippocampus, and right putamen compared with controls, with an inverse relationship between these susceptibility values and cognitive test scores. Whether common mechanisms underlie the susceptibility changes in vascular dementia, Alzheimers dementia and in early stages of Parkinsons dementia will need to be specifically examined in future studies that include histological analyses, or concurrent radio-ligand imaging.
Recommended Reading: Parkinson’s Big Movement Exercises
How Is Parkinsons Disease Treated
There is no cure for Parkinsons disease. However, medications and other treatments can help relieve some of your symptoms. Exercise can help your Parkinsons symptoms significantly. In addition, physical therapy, occupational therapy and speech-language therapy can help with walking and balance problems, eating and swallowing challenges and speech problems. Surgery is an option for some patients.
Literature Search And Study Selection
We conducted a search on PubMed using the identical search strings as in our previous metaanalysis: AND . The final search was conducted on June 30, 2020, and resulted in 3841 studies. We did not find any additional articles through review articles and reference tracing. We only screened studies using fMRI or H2O15PET during motor paradigms that were written in the English language, resulting in 170 studies that were further assessed by reading the abstract and/or main text. The following exclusion criteria were then applied for all experiments:
Review articles reporting no original data or PET studies other than H2O15PET .
Studies testing passive movements, eye movements , speech, motor learning, or executive control, for example, task switching .
Motor tasks were tested against each other rather than against baseline or a nonmotor control task, for example, fixation .
Neither of the contrasts PD OFF medication versus healthy controls,, PD ON medication versus healthy controls, or PD ON medication versus PD OFF medication were statistically compared .
Multivariate analyses or covariance analyses .
Fewer than 6 PD patients were included .
Studies in which PD patients were treated with deep brain stimulation or received acute challenges with drugs other than levodopa , because these treatments induce distinct effects on the sensorimotor system in PD, .
Don’t Miss: Why Does Parkinson’s Cause Hallucinations
Cholinergic Pathology In Parkinson Disease And Parkinsonian Dementia
A key pathologic hallmark of PD is loss of midbrain dopaminergic neurons of the substantia nigra, pars compacta, and of their terminals in the striatum. In addition to the well-known reductions in dopamine, there is convergent evidence for early alterations in cholinergic neurotransmission in PD. Braak et al. note early accumulation of a-synuclein deposition within basal forebrain cholinergic neurons in PD, apparently coincident with the occurrence of Lewy bodies and neuronal loss in the substantia nigra .
2.3.1. Cholinergic forebrain pathology
Significant loss of nbM cholinergic neurons is reported in PD brains . Arendt et al. found greater neuronal loss of nbM neurons in PD compared to AD , suggesting that cholinergic deficits may be at least as prominent in PD as in AD. Dysfunction of the basal forebrain cholinergic system is accompanied by a consistent loss of presynaptic cholinergic markers in cortex, sometimes accompanied by loss of muscarinic receptor binding sites. For example, muscarinic binding and ChAT activity are reduced in the pars compacta of the substantia nigra , hippocampus, and especially in the neocortex in PD .
2.3.2. Cholinergic brainstem pathology
Changes In Thalamus In Parkinson’s Disease
Thalamic lesions are found to impair cognitive functions such as language, memory, and attention. Thalamic stimulation was effective in enhancement of cognition through activation of neocortex and hippocampus and modulating gene expression. Approximately 30%-40% loss was reported in the thalamus in PD. It was reported that volume of the thalamus decreases in PD. In contrast, it was reported that thalamic shape but not volume changes in PD. As specific nuclei of the thalamus are involved in PD, atrophy of the caudal intralaminar nucleus and hypertrophy of rest of the nucleus result in altered shape of the thalamus. Further, changes in white matter of the mediodorsal thalamus lead to depression in most of the PD patients. Significant reduction in fractional anisotropy was reported in anterior nucleus, dorsomedial nucleus, and ventral anterior nucleus of the thalamus.
Don’t Miss: Is Thumb Twitching A Sign Of Parkinson’s
Sidebar: Advances In Circuitry Research
The brain contains numerous connections among neurons known as neural circuits.
Research on such connections and networks within the brain have advanced rapidly in the past few years. A wide spectrum of tools and techniques can now map connections between neural circuits. Using animal models, scientists have shown how circuits in the brain can be turned on and off. For example, researchers can see correlations between the firing patterns of neurons in a zebrafishs brain and precise behavioral responses such as seeking and capturing food.
Potential opportunities to influence the brains circuitry are starting to emerge. Optogenetics is an experimental technique that involves the delivery of light-sensitive proteins to specific populations of brain cells. Once in place, these light-sensitive proteins can be inhibited or stimulated by exposure to light delivered via fiber optics. Optogenetics has never been used in people, however the success of the approach in animal models demonstrates a proof of principal: A neural network can be precisely targeted.
Thanks in part to the BRAIN Initiative, research on neural circuitry is gaining momentum. The Brain Research through Advancing Innovative Neurotechnologies Initiative is accelerating the development and application of new technologies that enable researchers to produce dynamic pictures of the brain that show how individual brain cells and complex neural circuits interact at the speed of thought.
NIH Publication No. 15-5595
Exercise To Change The Brain
A novel exercise modality to improve motor learning in PD
For someone with Parkinsons disease, the simple desire to grasp a glass of water can become an insurmountable task, made impossible by the tremors in their hand or arm. Finding strategies to improve these movement impairments is one of the major goals of rehabilitating people with Parkinsons disease.
At McGill University, Marc Roig, an assistant professor in the School of Physical and Occupational Therapy, is studying the effects of using high-intensity exercise to stimulate the brains ability to learn and change with repeated experiences.
Roig and his team are working with people who have Parkinsons disease, to see if they can improve their ability to move and to complete tasks like grabbing an object. The team is using high-intensity cardiovascular exercise to provoke changes in the brain that make it easier to train itself to relearn motor tasks.
One of the main problems with people with Parkinsons is they lose their ability to do very simple motor tasks, says Roig, a neuroscientist. We want to understand why this happens and try to find interventions to improve that.
After they exercise, the people enrolled in Roigs study will also have to complete a task involving the application of force in a computer game, to measure whether the exercise and the burst of brain chemicals it stimulates also improves their motor ability.
Search
Read Also: Parkinson’s Disease Advocacy Groups
Changes In Limbic System In Parkinson’s Disease
Influence of limbic structures on cognition was well documented. Atrophy of gray matter was observed in Parkinson’s patients with dementia. Dopamine dysfunction in the limbic system leads to change in the creativity and emotional dysfunction in PD patients. In amygdala, accessory cortical and central nuclei are affected more by PD, and cortical, accessory basal, and granular nuclei are least affected areas. Posterior cingulum is the important structure in the papez circuit which is involved in processing of episodic memory. It was reported that neuronal loss, gliosis, or demyelination in the white matter and metabolic changes occurs in the cingulum of PD patients. Change in the spontaneous resting-state neural activity is reported in prefrontal cortex, which was considered as a factor for cognitive decline in PD. Further, regional atrophy in the hippocampus contributes to impaired verbal learning memory and visuospatial processing.
What Causes Personality Changes
Because the brain substantially affects our personality, changes to it can influence who we are. How one thinks, experiences emotions, and enacts certain habits can be seen as demonstrations of their personality. As Parkinsons disease progresses, it frequently affects memory and movement, which can change how a person functions.
Many caregivers note that their loved one with Parkinsons experiences heightened anxiety and depression throughout the course of their disease progression, and its possible that these feelings can contribute to personality changes. My dad has experienced changes in his anxiety levels, and I suspect there have been chapters of depression as well. But I dont think his personality has changed because of his battles with these symptoms. Hes his same old comedic self, passing time by telling jokes and watching local wildlife.
Im not sure hes the same person he was before diagnosis, but I dont know if thats due to DBS or Parkinsons disease. Were all fluid. We change with the tides and adapt over time. Who is to say that the changes my dad sees are a result of his disease?
Recommended Reading: What Can Mimic Parkinson’s Disease