Orthostatic Hypotension And Parkinsons Disease
One of my fellow boxers at the Rock Steady Boxing affiliate in Hilton Head/Bluffton, SC has been having issues of dizziness and brain fog/light headedness. Hes not alone, as 1 in 5 people with Parkinsons are also diagnosed with Orthostatic Hypotension. Ive been collecting some information to help him prepare for his next doctors appointment, and thought this may be helpful to share with others.
Most of us are familiar with the term hypertension, which refers to high blood pressure. Hypotension refers too low blood pressure. Orthostatic is a medical adjective that indicates a condition relating to or caused by an upright posture. Orthostatic hypotension is a condition in which your blood pressure falls significantly when you stand up quickly.
Blood pressure is written as two numbers for example, 120 over 80 mm Hg. The first number is the systolic pressure. This is the pressure in the arteries when the heart beats and fills them with blood. The second number is the diastolic pressure. This is the pressure in the arteries when the heart rests between beats.
Low blood pressure causes the feeling of light headedness and can lead to fainting. This condition contributes significantly to the risk of falling and injury .
OH can be caused by multiple conditions:
- Dehydration
- Endocrine Problems
- Nervous Systems Disorders, such as Parkinsons Disease
Theres no real magic bullet for treating OH, but there are some strategies to help manage it.
Continuous Dopaminergic Stimulation Therapies
Deep brain stimulation
Cross-sectional studies have suggested a positive effect of subthalamic Deep Brain Stimulation on autonomous responses of PD subjects . In one of this analysis, including 14 patients, there was a mean general decrease on blood pressure in on and off stimulation status ,1), but the baroreflex responses were preserved only when the stimulation was on, suggesting, therefore, a positive influence of the DBS in BP mediated by its influence on central autonomous nervous system pathways . In another study comparing subthalamic DBS with a pharmacotherapy-only group, no positive correlation was found between the on-stimulation state and the decrease in blood pressure but this occurred in the only medicated group. Based on this finding it was suggested that subthalamic DBS did not affect cardiovascular autonomous responses . Noteworthy, in a previous longitudinal study, the initial differences of blood pressure were not found after 1years follow-up, with a similar mean blood-pressure decrease for the subthalamic DBS and the only medicated groups . Additionally, two other studies could not find differences in the cardiovascular responses of the treated subjects .
Apomorphine pump/apomorphine injections
Continuous duodenal L-DOPA infusions
Normal Ans Response To Standing
Postural change induces gravitational redistribution of blood volume, leading to changes in blood pressure. Upon standing, pooling of venous blood in the legs is countered by the normal sympathetic ANS to maintain standing blood pressure. Lying supine also causes gravitational redistribution of blood volume, and the normal ANS minimizes blood pressure from rising too high. Norepinephrine is the major neurotransmitter in the ANS regulation of blood pressure in response to postural changes. Sympathetic activation in response to standing leads to: venoconstriction with increased venous return an increase in heart rate and myocardial contractility with increased cardiac output and vasoconstriction with increased blood pressure. Normal activation of the intact ANS, along with sufficient circulating blood volume, prevents the gravity-induced fall in standing systolic blood pressure , maintaining cerebral perfusion and of other vital organs.
You May Like: What Is An Off Period In Parkinson’s
What Is Neurogenic Orthostatic Hypotension
OH is a sustained fall in blood pressure that happens within 3 minutes of standing. OH can reduce blood flow to organs above the heart, most notably the brain, and its symptoms can have a profound impact on your quality of life. OH is more common in the elderly, and certain medications, dehydration, varicose veins, severe anemia and conditions such as heart disease can lead to OH. OH can also be related to the nervous system. Parkinsons, pure autonomic failure, multiple system atrophy and other types of autonomic dysfunction can all cause OH.
OH can be caused by the body not releasing enough of the neurotransmitter, norepinephrine. When your body doesnt release enough norepinephrine, your blood vessels dont constrict when they need to, lowering your blood pressure and causing you to feel faint when you stand or sit up. When OH is caused by problems in the release of norepinephrine, it is referred to as neurogenic orthostatic hypotension .
Orthostatic Hypotension In Parkinsons Disease Multiple System Atrophy And Lewy Body Dementia
Movement disorder specialist, Dr. Veronica Santini spoke for a half hour on orthostatic hypotension, a common symptom of Parkinsons disease, Multiple System Atrophy and Lewy Body Dementia. Following her talk, moderator Candy Welch, Brain Support Networks MSA caregiver support group leader, presented Dr. Santini with questions from webinar participants for another half hour.
Recommended Reading: What Are The Environmental Causes Of Parkinson Disease
Effects Of Parkinsons Disease On Blood Pressure
This short web page explains the physical operation of blood pressure in the body, symptoms of low blood pressure and when they are most likely to occur, why low blood pressure is dangerous, medical treatments and lifestyle strategies to cope with low blood pressure, and a reminder that low blood pressure can affect the ability to drive safely.
Temporal Variants Of Orthostatic Hypotension
In addition to OH defined as a BP drop within 3 min of standing , thereare two other temporally defined forms of OH that can be identified by clinicalBP measurements. Initial OH is a transient drop in BP that occurs immediatelyupon standing and resolves within 3060 s of active standing, and delayed OH isa sustained drop in BP that occurs beyond 3 min of standing . One large study of delayedOH monitored BP during 45 min of head-up tilt however, there is currently noaccepted standard for the length of time to test in the upright position forthis condition .
Initial OH differs from classical and delayed OH in several ways.Initial OH is defined by a greater magnitude of BP decrease within 15 s of active standing, withrestoration of normotensive BP within 3060 s . Signs and symptoms ofinitial OH are similar to those of the classical form of OH . However, initial OH is notassociated with a particular disease state or with autonomic failure, and theprevalence of initial OH in patients with PD is currently unknown .
Delayed OH occurs in some patients with PD and is thought to be related to, or aprecursor of, classical OH . In one study, more than half ofpatients with delayed OH developed classical OH during 10 years of follow-up. Delayed OH may be a mildor early form of sympathetic adrenergic failure and has been associated with thedevelopment of neurodegenerative disorders andincreased mortality .
Read Also: How To Test Yourself For Parkinson’s
Stay Informed On Your Parkinsons Journey
Would you like to learn more about nOH and living well with Parkinsons?
Our Every Victory Counts® manual gives people living with Parkinsons, their care partners and their family members the tools they need to take control of their own Parkinsons treatment through a proactive approach to self-care.
a powerful new print edition
Its jam-packed with up-to-date information about everything Parkinsons, plus an expanded worksheets and resources section to help you put what youve learned into action. Color coding and engaging graphics help guide you through the written material and point you to complementary videos, podcasts and other materials on the Every Victory Counts companion website. And, it is still free of charge thanks to the generosity of our sponsors.
Request your copy of the new Every Victory Counts manual by clicking the button below.
Dr. Jose-Alberto Palma is Assistant Professor of Neurology and Assistant Director of the Dysautonomia Center at New York University. His work over the past years has been focused on the diagnosis, management and understanding on autonomic disorders in patients with autonomic synucleinopathies, such as Parkinson disease and multiple system atrophy, as well as in the search for biomarkers for early diagnosis of these disorders. He has been involved in several studies and clinical trials to develop new treatments for autonomic dysfunction, and to describe the premotor phase of Parkinson disease.
Management Of Orthostatic Hypotension In Parkinsons Disease
Issue title: Special Issue: Clinical management of Parkinsons disease: Essentials and new developments
Guest editors: Bastiaan R. Bloem and Patrik Brundin
Article type: Review Article
Authors: Fanciulli, Alessandraa * | Leys, Fabiana | Falup-Pecurariu, Cristianb | Thijs, Rolandc d | Wenning, Gregor K.a
Affiliations: Department of Neurology, Medical University of Innsbruck Innsbruck, Austria | Department of Neurology, Transilvania University, Faculty of Medicine Brasov, Romania | Department of Neurology, Leiden University Medical Centre, Leiden, The Netherlands | Stichting Epilepsie Instellingen Nederland , Heemstede, The Netherlands
Correspondence: Correspondence to: Alessandra Fanciulli, MD, PhD, Department of Neurology, Medical University of Innsbruck, Anichstraße 35, A-6020 Innsbruck, Austria. Tel.: +43 512 504 83238 E-mail: .
Keywords: Parkinsons disease, orthostatic hypotension, post-prandial hypotension, supine hypertension, nocturnal hypertension
DOI: 10.3233/JPD-202036
Journal: Journal of Parkinson’s Disease, vol. 10, no. s1, pp. S57-S64, 2020
Abstract
You May Like: Non Tremor Parkinson’s Disease
Impaired Ans Response To Standing In Noh
In patients with PD and nOH, autonomic dysfunction causes blood pressure to fall upon standing, due to an inappropriate NE response to postural change. Orthostatic hypotension has been defined as a drop in SBP of at least 20 mmHg or a drop in diastolic blood pressure of at least 10 mmHg after 3 minutes of standing. There is often a loss of the cardioacceleratory response too. Non-neurogenic causes of orthostatic hypotension are also common in patients with PD, and contribute to blood pressure drop. These non-neurogenic causes of orthostatic hypotension should be identified first, and include dehydration, medications, and cardiac pump failure. A clinical diagnosis of nOH can be made when these non-neurogenic causes of persistent orthostatic hypotension are excluded, and can be confirmed through autonomic testing and plasma NE levels.
In PD, autonomic dysfunction is mainly a result of cardiac sympathetic denervation with inadequate activation of NE pathways, and also baroreflex failure. This can emerge during the course of PD or can occur early in its course. Parkinsonism due to multiple system atrophy is also accompanied by prominent autonomic dysfunction, but nOH results from failure of central NE pathways.,
Orthostatic Hypotension: A Prodromal Marker Of Parkinson’s Disease
Department of Epidemiology, Erasmus MC University Medical Center, Rotterdam, the Netherlands
Department of Neurology, Erasmus MC University Medical Center, Rotterdam, the Netherlands
Francesco U.S. Mattace Raso PhD
Department of Geriatric Medicine, Erasmus MC University Medical Center, Rotterdam, the Netherlands
Department of Epidemiology, Erasmus MC University Medical Center, Rotterdam, the Netherlands
Department of Neurology, Erasmus MC University Medical Center, Rotterdam, the Netherlands
Correspondence to: Dr. M. Kamran Ikram, Erasmus MC University Medical Center, P.O. Box 2040, 3000 CA Rotterdam, the Netherlands E-mail:
Department of Epidemiology, Erasmus MC University Medical Center, Rotterdam, the Netherlands
Department of Neurology, Erasmus MC University Medical Center, Rotterdam, the Netherlands
Francesco U.S. Mattace Raso PhD
Department of Geriatric Medicine, Erasmus MC University Medical Center, Rotterdam, the Netherlands
Department of Epidemiology, Erasmus MC University Medical Center, Rotterdam, the Netherlands
Department of Neurology, Erasmus MC University Medical Center, Rotterdam, the Netherlands
Correspondence to: Dr. M. Kamran Ikram, Erasmus MC University Medical Center, P.O. Box 2040, 3000 CA Rotterdam, the Netherlands E-mail:
Lisanne J. Dommershuijsen and Alis Heshmatollah contributed equally to this article.
Relevant conflicts of interests/financial disclosures:: Nothing to report.
You May Like: Physical Symptoms Of Parkinson’s Disease
Whats Hot In Pd If You Are Dizzy Or Passing Out It Could Be Your Parkinsons Disease Or Parkinsons Disease Medications
This 3-page article, with references, is a personal statement by Dr. Okun describing the mis-diagnoses Parkinsons patients can be given when visiting the ER for symptoms of dizziness or syncope outlining what defines a proper diagnosis of orthostatic hypotension, its frequency in people with Parkinsons, medication and lifestyle changes that can help.
What Are The Symptoms Of Noh
nOH can appear with or without symptoms. The typical symptoms of nOH are lightheadedness, dizziness, blurry vision and, when theres a significant drop in blood pressure upon standing up, fainting. Symptoms almost always occur when standing up, less frequently when moving from standing to sitting and abate when lying down. People with nOH may also experience weakness, fatigue, leg buckling, headaches, neck and shoulder discomfort and shortness of breath. Severity of symptoms varies from day to day and fluctuates throughout the day. Often, mornings tend to be most difficult since nOH symptoms are aggravated by overnight urination, which is common in people with Parkinsons. Meals, particularly those rich in carbohydrates and sugars, also cause drops in blood pressure.
In people with Parkinsons, symptoms of nOH can also be non-specific, including fatigue and difficultly concentrating, and may sometimes mimic a levodopa off state. Its easy to miss nOH unless your physician measures your blood pressure while you are in a standing position. Conversely, it is important to realize people with Parkinsons can experience lightheadedness that mimics nOH, but may instead be caused by balance problems or other issues. For this reason, careful evaluation of your symptoms by a movement disorder specialist is strongly advised.
Also Check: List Of Parkinson’s Drugs
Full Financial Disclosures For The Last 12 Months
Alessandra Fanciulli: Dr. Fanciulli reports royalties from Springer Nature Publishing Group, speaker fees and honoraria from the Austrian Autonomic Society, Austrian Parkinson Society, Ordensklinikum Linz, International Parkinson Disease and Movement Disorders Society and Theravance Biopharma and research grants from the Stichting ParkinsonFond and the Österreichischer Austausch Dienst, outside of the submitted work.
Fabian Leys: Dr. Leys reports no disclosures.
Cristian Falup-Pecurariu: Dr. Falup-Pecurariu reports royalties from Springer Nature Publishing Group, speaker fees and honoraria from the International Parkinson and Movement Disorders Society, outside of the submitted work.
Roland Thijs: Dr. Thijs reports speaker fees from Novartis, consultancy fees from Theravance Biopharma and research support from the Dutch Epilepsy Foundation Dutch, the Netherlands Organization for Health Research and Development and De Christelijke Vereniging voor de Verpleging van Lijders aan Epilepsie, outside of the submitted work.
Gregor K. Wenning: Dr. Wenning reports consultancy fees from Biogen, Biohaven, Lundbeck, Minoryx, Takeda, Theravance and research support from the Austrian Science Fund, International Parkinson Disease and Movement Disorders Society and the Medical University Innsbruck, outside of the submitted work.
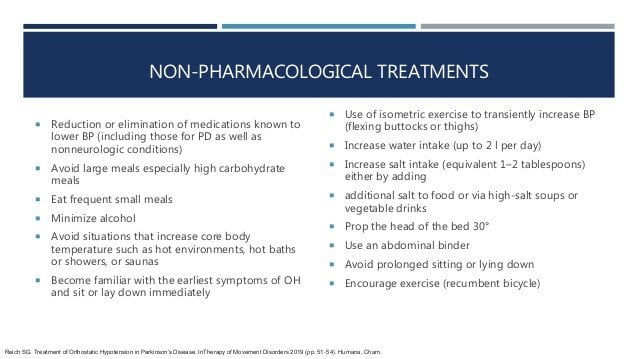
Managing Orthostatic Hypotension For Your Safety
Orthostatic hypotension also known as postural hypotension is a form of low blood pressure.
It happens when the blood vessels do not constrict as you stand up from a sitting or lying position.
It can also be experienced as a side-effect of medication taken for Parkinsons, or when a person is taking anti-hypertensive medications when they are no longer required. Orthostatic hypotension can also be a pointer to a Parkinsons diagnosis.
Its symptoms include:
- Feeling dizzy or light- headed
- Blurred vision
How to manage orthostatic hypotension:
- Do not sit or stand or be inactive for long periods
- Avoid activity in the heat
- Stay cool
- Prior to getting up, move your toes around and adjust your heels and calf muscles
- Allow your feet to dangle on the floor for a short time if getting out of bed
- Gentle marching leg movements may also help
- Get up slowly, stand for a short time and monitor for steadiness
- If feeling dizzy or faint, sit with your legs elevated until the feeling passes
- Ensure that you are well hydrated drink a glass of water prior to getting up
- If feeling dizzy at the end of a meal, try having a glass of water then
- Reach over slowly and find a hand-hold to prevent over balancing
- Eat smaller meals more frequently
- Avoid straining whilst having bowels open
- Avoid vigorous exercise
Recommended Reading: What Age Can Parkinson’s Disease Start
Postural Adjustments And Countermeasures
- Avoid rising to a standing position too quickly.
- When getting out of bed, start by moving to a seated position first. Wait some period of time before slowly leaning into a stand.
- Similarly, when getting out of a car, keep your body supported and slowly rise out of the car.
- Many sources recommend elevating the head of your bed by 10 to 20 degrees or 4 inches to decrease nighttime hypertension , which should reduce the degree of blood pressure drop when rising.
- Physical countermeasures are techniques to contract the muscles below the waist for about 30 seconds at a time, which reduces blood volume in lower body peripheral vessels and encourages blood flow return to the heart. These countermeasures can help maintain blood pressure during daily activities and should be considered at the first symptoms of orthostatic hypotension symptoms or when standing for prolonged periods of time:
- Toe-raising
- Bending at the waist
- Slow marching in place
- Leg elevation
The Effect Of The Anti
One of the initial steps required when assessing a patient who is going to receive any anti-parkinsonian medication/treatment or who needs a dose adjustment is to anticipate the potential effect on his blood pressure, as it is one of the commonly related factors to the appearance of OH .
Several actions could help to improve the detection of this complication, either by the physician or the subject. It seems reasonable to instruct the patient about OH symptoms , although many cases go unnoticed . An initial pressor response assessment could be valuable to have a simple measurement to monitor future changes, as this measurement is one of the easiest ways to appraise OH in various healthcare settings.
Many caveats should be considered prior to establishing the real influence of PD medications on OH. First, there are different diagnostic criteria for defining OH. Additionally, much evidence is based on cross-sectional analyses and other confounding effects, as disease duration or previous autonomous nervous system damage , have not always been considered.
We present the current evidence to estimate the potential role of current PD treatments on OH. The influence of other drugs, such as antidepressants, diuretics, and antihypertensives, is not reviewed here. Nevertheless, they should be considered when dealing with this complication and decreasing the dose or stopping the responsible medication might be advisable.
Also Check: Hypothyroidism Misdiagnosed As Parkinson’s