Three Advantages Of Mrgfus For Pd Tremor
MRgFUS is a noninvasive outpatient procedure. No scalpel is needed to cut skin, no drill is needed to bore a hole in the skull, and nothing is implanted in the brain. Its three main advantages for PD-related tremor are:
A few words of caution: MRgFUS is not effective in every case. As with MRgFUS for ET, treatment will be directed to the hand in which tremor is worse, since treating both hands increases the risk of side effects. Clinical studies show that some patients have short term side effect such as headaches, dizziness or nausea but these quickly resolve. However, the effect may not be durable. Patients who have suffered with significant tremor for years may experience less effective tremor control, or gradual recurrence of tremor. Finally, MRgFUS does not cure PD, nor will it have an effect on other PD-related problems.
However, the consensus among researchers is that MRgFUS is a very promising treatment for PD-related tremor, especially as an alternative to invasive surgical procedures. If you or a loved one suffers from severe PD tremors, contact the Sperling Medical Group for more information about MRgFUS.
- CATEGORY:
Recommended Reading: Sam Waterston Parkinsons
For Tremor Dominant Parkinson’s Disease
Parkinson’s disease is the second most common neurodegenerative condition, affecting about 1% of people over 60 years old. MR-guided focused ultrasound has become an attractive treatment option to improve tremor control for patients who do not respond to dopamine replacement medications.It is essential to recognize that focused ultrasound is not a cure for Parkinson’s disease, and it does not stop the progression of the disease. Some motor symptoms such as balance difficulties, speech problems, swallowing difficulties, and cognitive decline develop or worsen as Parkinson’s disease progresses and usually do not improve with focused ultrasound. Similarly, the non-motor complications of Parkinson’s disease, such as depression, problems with thinking or memory, constipation, or urinary changes do not improve after focused ultrasound.
What Happens During Mri
Before your procedure you will have an MRI, which your care team will use to pinpoint the area of your brain to be treated.
During the treatment, you will lie in an MRI scanner with your head fitted into a water-filled helmet. The helmet circulates cool water around your head to prevent overheating during the ultrasound. The energy is first applied at a low level and your doctor will ask you to provide feedback on the effect it has on your hand tremor.
You will be engaged throughout the process and may be asked to report the sensations you feel and to perform tasks such as writing or tracing lines to monitor improvement of your tremor. Your doctor will then adjust the focused ultrasound treatment in response to your input, increasing the energy level to perform the amount of ablation needed.
The focused ultrasound energy waves pass through the helmet to meet at the identified point in your brain. The energy makes a small lesion in the brain, targeting the tissue where the tremors originate.
After treatment, youll be moved to a recovery room for monitoring. Most patients go home the same day. Many return to work and other activities within a couple of days. You will receive specific discharge instructions from your doctor.
Also Check: Is Parkinson A Form Of Dementia
Patient Considerations For Gene Therapy
With genetic testing becoming more widely available, it is feasible to consider selecting patients for certain therapies based on their genotype. Patients with the advanced parkinsonian phenotype with motor fluctuations are expected to experience the greatest benefit from a gene therapy approach that aims to increase dopamine production. The unmodifiable nature of gene therapy must also be considered, particularly in patients with significantly advanced PD who are more susceptible to complications such as ICD and dopamine dysregulation syndrome. Studies investigating neurotrophic factors have emphasized the importance of targeting patients with earlier stages of PD when protecting and improving the health of dopaminergic neurons would be most beneficial .
Tremor Control Through Neurosurgery

Essential tremor is a movement disorder that most commonly affects the hands, head and voice. Since our hands are involved in practically every personal, professional and recreational task, the shakes create disabilities that range from annoying or frustrating to severely impairing. While medication is the first line of treatment, it is ineffective for about 50% of people among those who find it effective, a large number have to increase doses over time until eventually medication no longer works. When tremors resist drug treatment, it is called refractory ET.
Those who develop refractory ET are usually encouraged to consider a neurosurgery to control tremors. Such procedures intervene in the brains thalamus, a center that forwards abnormal tremor signals out to the body. There are two types of procedures:
Also Check: How Long Does Someone Live With Parkinson’s Dementia
Continuous Subcutaneous Apomorphine Infusion
Apomorphine is a dopamine agonist with a mixed affinity for D1 and D2 receptors and an affinity for serotonergic and alpha-adrenergic receptors . While the motor efficacy of apomorphine is similar to that of levodopa, apomorphine cannot be administered orally due to its low oral bioavailability . Subcutaneous infusions have a similar pharmacokinetic profile to the intravenous route. Compared with intermittent subcutaneous injections, CSAI has a longer apparent plasma half-life and simulates the physiological stimulation of striatal neurons .
Clinical outcomes of CSAI
In the OPTIPUMP cohort study, the efficacy and safety of CSAI were assessed. The total UPDRS score showed significant improvement in all patients at 6 months. UPDRS-III decreased in the on-medication state by 16.3% . In the first prospective, randomized, placebo-controlled trial to investigate the efficacy and safety of apomorphine subcutaneous infusion in PD patients, a daily off time reduction of 1.89h from a baseline of 6.69h was seen in treated patients, while there was an increase of 1.97h in on time without TSD from a baseline of 8.52h . In a retrospective study, 230 patients were treated with CSAI over 10 years. In this cohort, the daily off hours were reduced from 5.4 to 1.2h .
Safety of CSAI
Patient considerations for CSAI
Focused Ultrasound For Essential Tremor And Parkinsons
OHSU is the only Oregon hospital to offer focused ultrasound for essential tremor and tremor-dominant Parkinsons disease. This life-changing treatment improves tremor symptoms for most patients right away. Benefits include:
Advanced technology thats safer for you. This treatment combines ultrasound with MRI. This means we can do surgery without an incision while youre awake. No cutting means no risk of problems like infection. Being awake means no anesthesia and you can see results in real time.
Improves your quality of life. Most patients have reduced tremor symptoms on one side right away. For more than 75% of patients, improvements were still there three years later.
Outpatient procedure. Most patients return to daily activities within a day. Temporary side effects of the treatment stop within a week.
To schedule an evaluation for focused ultrasound treatment for essential tremor or tremor-dominant Parkinsons disease, call our clinic at , or email us at .
Recommended Reading: Israeli Treatment Of Parkinson Disease
Clinical Outcomes And Adverse Events Of Mrgfus
Ventral intermediate
In a study by Bond et al., 20 patients were randomized to focus ultrasound unilateral VIM thalamotomy versus 7 patients to the sham procedure for patients with medically refractory tremor-dominant PD. Hand tremor, as measured with the Clinical Rating Scale for Tremor A+B subscores in the on-medication state, improved by 62% at 3 months. Total CRST scores improved by 44% at 3 months. The most common procedure-related AEs for all patients were finger and orofacial paresthesia. Two patients had persistent hemiparesis, and one patient had persistent mild ataxia .
Globus pallidus internus
A multicenter open-label trial investigated the efficacy and safety of MRgFUS ablation of the GPi for PD patients exhibiting levodopa responsiveness, motor fluctuations, and asymmetrical motor signs. There was a 44.5% improvement in the off-medication UPDRS-III score from baseline value at 3 months and a 45.2% improvement at 12 months. The UPDRS-IV score was used to assess the motor complications of PD. The baseline pretreatment value was reduced by 42% at 3 months, and this improvement was maintained at 12 months. Twenty persistent AEs were reported, including fine motor difficulties, dysarthria, and balance difficulties .
Subthalamic nucleus
Clinical Outcomes And Adverse Events
Gamma knife thalamotomy has been shown to improve motor function in patients with PD. The radiation dose used in GK thalamotomy ranges from 120 to 180Gy, and it appears that doses less than 120Gy do not provide clinical benefits . In a prospective study of unilateral gamma knife thalamotomy for patients with PD and essential tremor , Ohye et al. reported an improvement in tremor scores , with 81.1% of patients evaluated as having good or excellent results at 24-month follow-up . A more recent prospective, single-blind study of unilateral GK thalamotomy for patients PD and ET reported a 54.2% improvement in the upper limb tremor score . GK pallidotomy has also been performed to treat PD, although only a few reports have described the procedure . The GPi is considered a high-risk target for GK radiosurgery due to its proximity to the optic tract and the risk of optic neuropathy . Likewise, the STN is not an advised target due to the risk of neurologic complications including hemiparesis, dysarthria, and gait disturbances .
Also Check: Does Nick Nolte Have Parkinson’s Disease
Mrgfus Focused Brain Ultrasound
Watch this remarkable video of another one of our MRGFUS patients who has benefited from their treatment under the watchful eye of our team. His tremor is treated and you can see the control he now has over his shaking immediately post procedure.
MRI-guided Focused Ultrasound is noninvasive treatment, used primarily to treat essential tremor, tremor-dominant Parkinsons disease, and certain types of chronic pain.
After a single treatment, most patients report an immediate relief or significant improvement in their symptoms.
Focused ultrasound can penetrate the skull without the need to make an incision or drill holes in the skull.
Precision can offer short wait times for MRgFUS. We can see you within four weeks for a consultation and, if suitable, administer your treatment within three months of you contacting us.
If you have additional questions, please email .
Focused ultrasound is an innovative neurosurgical platform which delivers ultrasound energy deep in the brain with incredible precision.
This deliberately creates a small scar or lesion in the brain without incisions.
This procedure is carried out without anaesthetic or incisions.
The neurosurgeon and neuroradiologist sit at a computer console in the MRI control room, using a computer and mouse instead of a surgical scalpel.
But, at the focal point, the multiple beams of focused ultrasound energy converge, and this results in many important biological effects.
Have a question? Email your referral or enquiry to .
Fda Approves Focused Ultrasound For Parkinsons Symptoms
Jeff Elias, MD, pioneered the use of focused ultrasound for the treatment of essential tremor and Parkinson’s disease.
The federal Food and Drug Administration has approved an incisionless form of brain surgery to treat advanced Parkinsons disease after successful testing at the School of Medicine and other sites.
The authorization allows the use of Insightecs Exablate Neuro focused ultrasound device to treat problems with mobility, rigidity and involuntary movements known as dyskinesias that are common in Parkinsons. UVA is one of only 37 medical centers in the country with the capacity to offer this minimally invasive treatment, according to the Charlottesville-based Focused Ultrasound Foundation, a longtime supporter of UVAs pioneering research into the many potential applications of the technology.
Prior to the approval, available treatments for the Parkinsons symptoms included drugs, which not all patients respond to, and invasive deep-brain surgeries. Focused ultrasound, in comparison, does not require incisions or cutting into the skull. Instead, the technology focuses sound waves inside the brain to interrupt faulty brain circuits, much like a magnifying glass can focus light to create heat. During the focused ultrasound procedure, doctors use magnetic-resonance imaging to peer inside the brain in real-time before making any permanent changes, helping ensure patients get the best possible outcomes.
Read Also: Parkinson Voice Project Speak Out
Focused Ultrasound Shows Promise For Parkinsons Disease
Jeff Elias, MD, pioneered the use of focused ultrasound for the treatment of essential tremor and Parkinsons disease.
A scalpel-free alternative to brain surgery has the potential to benefit people with Parkinsons disease symptoms that are much more severe on one side of the body, new research suggests.
More testing is needed, but the approach, which uses a technology called focused ultrasound, could offer a new option for patients whose symptoms are poorly controlled by medications and those who cannot or do not wish to undergo traditional brain surgery.
This small brain region, the subthalamic nucleus, had a very strong and potent effect on Parkinsonian symptoms when we targeted it with precise, focused ultrasound energy, said researcher Jeff Elias, MD, a neurosurgeon at UVA Health and a pioneer in the field of focused ultrasound. The key for the ultimate adoption of this new procedure will be further refinements of the technology to ensure reliability and safety.
Who Can Have Mri
MRI-guided focused ultrasound may be a treatment option for people with essential tremor or with Parkinsons disease when hand tremor is the primary symptom and medications have not worked. Patients with essential tremor must be at least 22 years old and patients with tremor-dominant Parkinsons disease must be at least 30 years old to receive this treatment.
MRI-guided focused ultrasound is not suitable for all patients. You may not be eligible if you have:
- Metallic implants such as a pacemaker, neurostimulator, spine or bone fixation device, total joint replacement, metal clips, screws or cochlear implants
- Heart or spine issues that may make it difficult to tolerate the treatment or lie still for about 3 hours
- Extensive scarring on your scalp
- Tumors inside your skull
What is the Neuravive treatment? Neuravive is a new treatment for essential tremor where sound waves are focused through the skull to a target without the need for incisions, brain implants or radiation. It is based on high intensity focused ultrasound guided by MR imaging. During the procedure ultrasound waves pass through the skull and are focused on a specific target in the brain. The temperature at the target rises high enough to create a tiny ablation or burn and provide a therapeutic effect, reducing the hand tremor. The MRI scanner provides images for the physician to clearly see the treatment area and provides images that show changes in temperature at the target.
Read Also: Does Parkinson’s Affect Heart Rate
Ventral Intermediate Nucleus Thalamotomy
Adverse events that transiently occurred during sonication in PD patients included the following: short lasting vertigo , headache , dizziness , nausea , burning scalp sensation , and lip paresthesia . Adverse events that lasted after the procedure included the following: asthenia , gait ataxia , unsteady feeling , unilateral taste disturbances , and hand ataxia . No adverse event lasted beyond 3 months. For a complete list of adverse events reported in this paper which also included essential tremor patients, see .
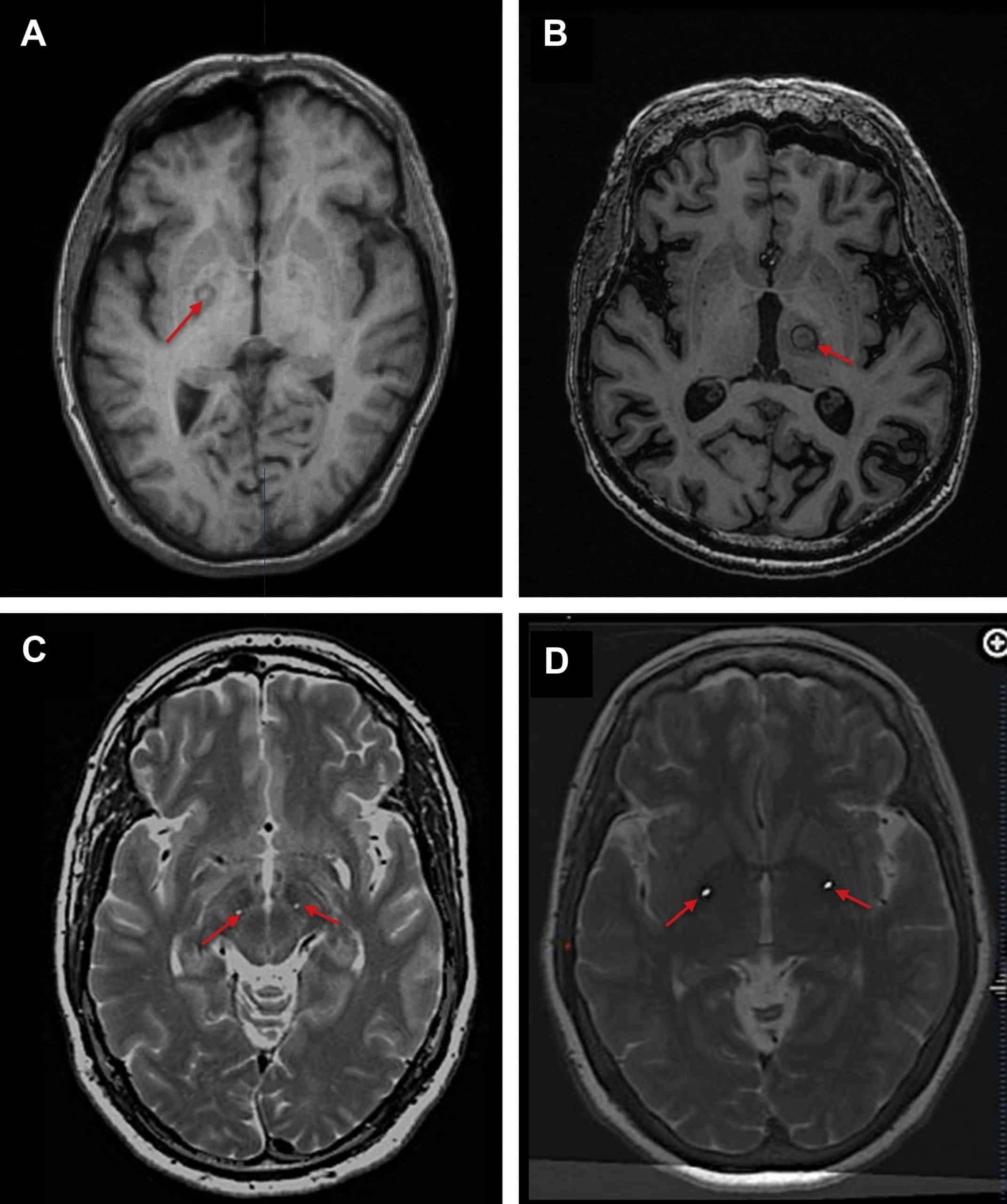
Lesions in the planned target were close to spherical with a diameter of 49mm . We observed mild edema one day after the procedure with increased edema one week after the procedure. The edema lasted for 35 weeks following the procedure. At 3 months, the edema resolved and lesion decreased in size.
The mean maximal temperature at the target was 56.5 ± 2.2°C . Patients underwent on average 21.1 ± 8.3 sonication with an average maximal sonication time of 16.2 ± 3.0 seconds . The mean maximal energy reached was 12,750 ± 4385 Joules .
Recently, Bond et al. reported in abstract form preliminary results of their double-blinded, randomized controlled trial to investigate the effectiveness of MRgFUS thalamotomy in tremor-dominant PD. They found that MRgFUS showed a trend toward improvement in hand tremor and a clinically significant reduction in mean UPDRS. They also noted a significant placebo response. Further information regarding this study is not yet available.
What Is The Treatment Process
If you have additional questions, please email .
Most patients experience a significant improvement to their tremor through the treatment process.
You May Like: Parkinson’s Plus Syndrome Icd 10