Screening For Cognitive Impairment In Parkinson’s Disease: Improving The Diagnostic Utility Of The Moca Through Subtest Weighting
-
Affiliations Department of Medical Psychology, Neuropsychology and Gender Studies, University Hospital Cologne, Cologne, Germany, Institute of Gerontology & Center for Neuropsychological Diagnostics and Intervention , University of Vechta, Vechta, Germany
-
Affiliation Department of Neurology, University Hospital Cologne, Cologne, Germany
-
Affiliation Department of Neurology, University Hospital Cologne, Cologne, Germany
-
Affiliation Department of Medical Psychology, Neuropsychology and Gender Studies, University Hospital Cologne, Cologne, Germany
-
Affiliation Department of Neurology, Center for Movement Disorders and Neuromodulation, University Hospital Düsseldorf, Düsseldorf, Germany
-
Affiliation Department of Neurology, Center for Movement Disorders and Neuromodulation, University Hospital Düsseldorf, Düsseldorf, Germany
-
Affiliation Department of Clinical and Developmental Neuropsychology, Faculty of Behavioural and Social Sciences, University of Groningen, Groningen, Netherlands
The Era Of Digital Cognitive Testing
The development of digital cognitive testing and the evolution of self-completed computerized assessments and wearable devices to assess cognitive functioning in daily life, provides an exciting opportunity to both improve clinical management and to obtain more sensitive outcome measures for clinical trials and will likely become a standard procedure in the future, given further technological improvements and increased access to the internet and digital devices. To reach this point, psychometric requirements , documentation and technical problems, as well as their relation to traditional tests, need to be well known.
How Are Cognitive Problems Treated
Much remains to be learned about the basic biology that underlies cognitive changes in PD. Researchers work towards the development of diagnostic tests to identify people who seem to be at greatest risk for cognitive changes and to differentiate cognitive problems in people with PD from those that occur in another disorder related but different known as dementia with Lewy bodies.
Read Also: Ten Steps To Identify Atypical Parkinsonism
Clinical Measures Of Cognition In Pd
Determining objective changes in cognitive function frequently involves neuropsychological testing. Test selection may depend on a number of factors such as age, education, and language. Test performance can be affected by motor function as well as physiological changes of aging . Therefore, neuropsychological testing in PD should include some measures that do not rely on manual dexterity or motor speed as these can be compromised and make it difficult to separate motor symptomatology from a given cognitive ability.
Many tests of global cognition have been studied or reviewed in PD, including the Mini-Mental State Examination, Montreal Cognitive Assessment , PD-Cognitive Rating Scale, Addenbrookes Cognitive Examination, among others.,,, Many tests covering different cognitive domains also have been used in PD. The Movement Disorder Society Task Forces for PDD and PD-MCI diagnostic criteria provide recommendations for assessments of cognitive domains and neuropsychological tests., Standardized protocols and PD-specific neuropsychological batteries may provide uniformity across multiple centers and research trials.
Cognition Deficits In Parkinsons Disease: Mechanisms And Treatment
1Department of Pediatrics, Renmin Hospital of Wuhan University, Wuhan, Hubei 430060, China
2Department of Neurology, Renmin Hospital of Wuhan University, Wuhan, Hubei 430060, China
3Department of Neurosurgery, Renmin Hospital of Wuhan University, Wuhan, Hubei 430060, China
Abstract
1. Introduction
As we know, the etiopathogenesis of PD characterized by irreversible disease progression is quite complicated and still lack of consensus to date, especially on the cognitive deficits of PD. A growing chorus of up-and-coming scholars ascribes the pathogenesis of PD to multineuropeptide dysfunction. Put another way, it is not only the progressive deterioration of dopaminergic neurons but defects in nondopaminergic systems that can lead to classical motor and nonmotor manifestations . Robust research component demonstrates that the early reduction of dopaminergic uptake in the frontal lobes is of crucial importance to cognitive impairment existing in PD patients . Accumulating lines of evidence suggest that the cholinergic disturbance within brainstem and corticostriatal pathways may be implicated in the pathophysiology of cognition deficits in PD . In addition, recent progress in PD has revealed that several genetic biomarkers and gene polymorphism may be connected with the generation and development of PD with cognition deficits.
2. Cognition Deficits in Parkinsons Disease
2.1. PD-MCI
2.2. PDD
3. Mechanisms
3.1. Neurochemical Substrates
3.1.1. Dopamine and Its Receptors
You May Like: Signs Of Parkinson’s Disease
What Is Normal Cognitive Aging And How Does Pd Fit In
Many people attribute cognitive changes to aging, and a major concern expressed by people with PD and their care partners is whether cognitive deficits are related to aging or to PD. Cognitive changes in people with PD need to be benchmarked against normative data and age-related changes. Cognitive decline without dementia can occur in aging, perhaps because neuropathological processes such as neuronal loss, deposition of amyloid, tau, and -synuclein, and vascular changes, often found post-mortem, are common as we age. The progression of cognitive decline is a key element in attributing changes to underlying disease-related processes. In general, cognitive changes in normal aging should not interfere significantly with everyday activities that require cognitive abilities. If they do, however, this may suggest an abnormal process and signal an increased risk of developing MCI or dementia. Changes in functional abilities and everyday activities due to cognitive decline can be difficult to identify if they are mild. Distinguishing whether problems in everyday activities are due to cognitive or motor problems in PD, or a combination of both, can be challenging, and appropriate measures for determining this are needed.
Executive Dysfunction In Parkinsons
Executive functions in cognition are higher-order mental processes, including the ability to plan, organize, initiate and regulate behavior to meet goals. Executive functioning is present in activities such as multitasking, switching tasks, and solving problems. The prefrontal cortex of the brain and the dopamine system are responsible for executive function. As PD damages these areas, executive dysfunction occurs, and executive dysfunction is one of the most common cognitive impairments found in people with PD.3,4
Don’t Miss: What Is Parkinson’s Disease And How Do You Get It
Atomoxetine For Cognitive Impairment In Parkinsons Disease
Objective/Rationale:Parkinsons disease causes well known motor symptoms of tremor, slowness and stiffness, but also leads to cognitive impairment. Research has shown that early loss of cells in a brain structure called the norepinephrine-locus ceruleus in PD corresponds with the development of cognitive deficits and is a novel target for PD therapeutics. Atomoxetine is a specific norepinephrine reuptake inhibitor, which increases the availability of this critical neurotransmitter at the brain level. Researchers hypothesize that treatment with ATM will improve attention, set-shifting, information processing speed and working memory in cognitively impaired people with PD.
Project Description: This is an early Phase II trial to prove the concept that ATM can improve certain aspects of cognitive function in PD. Investigators will accomplish this with a double-blind, placebo-controlled trial of ATM in 30 cognitively impaired, non-demented people with PD. They hypothesize that ATM will improve attention, set-shifting, information processing speed and working memory without compromising motor function. Thirty study subjects will be randomized to receive either ATM or placebo. A carefully designed neuropsychological test will be administered at baseline and after 10 weeks of ATM treatment.
Anticipated Outcome:The proposed work is expected to demonstrate whether ATM is worth pursuing with a larger, definitive clinical trial.
Neurochemical Deficits In Pdd
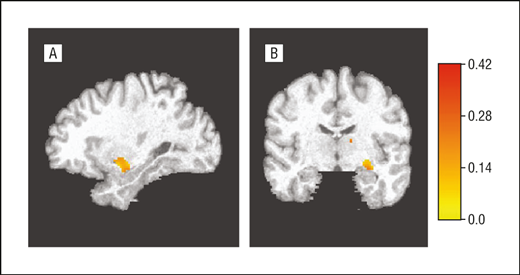
Degeneration of subcortical nuclei in PD leads to dopaminergic, cholinergic, noradrenergic, and serotoninergic deficits. Of them, cholinergic deficits due to degeneration of the nucleus basalis of Meynert have been the most involved in PDD. In early neuropathological studies, PDD patients showed more NMB cholinergic neuronal depletion when compared with AD and non-demented PD.33,34 A greater reduction of choline acetyltransferase activity in frontal and temporal cortex was found in PDD than in PD without dementia.35 Mattila et al reported reduced choline acetyltransferase activity in the hippocampus, prefrontal cortex, and temporal cortex in PD. Reduction in the frontal cortex correlated signicantly with the degree of cognitive impairment.36 Not only pathological studies but also neuroimaging studies have pointed out a role for a cholinergic deficit in cognition in PD. Both PD and PDD have cholinergic neuron decits with vesicular acetylcholine transporter and acetylcholinesterase 37,38 imaging being the decreased VAChT more important and extensive in the cerebral cortex of PDD subjects.39
There are not consistent findings supporting an association between dementia and other monoaminergic systems.
Recommended Reading: Arthritis And Parkinson’s Disease
Pd And Cognitive Impairment: Five New Things
-
Longitudinal studies show that the risk of dementia in PD increases with advancing age and that nearly all patients with PD develop dementia if they survive 20 years with the disease.
-
CSF biomarkers are beginning to define molecular signatures that may help to stratify risk of dementia in PD and track disease progression.
-
Genetic association studies have revealed links to other neurodegenerative diseases and implicate lysosomal dysfunction in the pathophysiology of PD dementia.
-
Sleep disturbance appears to exacerbate cognitive impairment in PD in particular, REM behavior disorder shares an overlapping pattern of cognitive impairment with PD and increases the risk of dementia.
-
Cognitive training may help improve outcomes when incorporated in a multidisciplinary therapy program.
Screening For Mild Cognitive Impairment In Parkinsons Disease: Comparison Of The Italian Versions Of Three Neuropsychological Tests
Stefano Tamburin
1Department of Neurological and Movement Sciences, University of Verona, Piazzale Scuro 10, 37134 Verona, Italy
2Department of General Psychology, University of Padova, Via Venezia 8, 35100 Padua, Italy
3Human Inspired Technologies Research Center, University of Padova, Via Venezia 8, 35100 Padua, Italy
4Neurology Unit Pederzoli Hospital, Via Monte Baldo 24, 37019 Peschiera del Garda, Italy
5Neuromotor and Cognitive Rehabilitation Research Centre, University of Verona, Piazzale Scuro 10, 37134 Verona, Italy
Abstract
1. Introduction
Cognitive impairment is frequent in Parkinsons disease , and the spectrum of cognitive dysfunction ranges from mild cognitive impairment to PD dementia . The diagnosis of PD-D may to some extent be straightforward , but recognizing MCI in PD is more difficult. Cognitive deficits may occur early in PD course, and they can be documented in up to a quarter of newly diagnosed PD patients . The biological validity of PD-MCI as a clinical entity is supported by converging morphological, functional neuroimaging, neurophysiological, genetic, and cerebrospinal fluid and histological data showing an association between a number of neuropathophysiological variables and cognitive impairment or cognitive decline in nondemented PD patients .
2. Materials and Methods
2.1. Subjects
After screening for inclusion criteria , 43 patients were included in the study. Demographic and clinical characteristics of patients are reported in Table 1.
You May Like: Fda Approved Parkinson’s Drugs
Contributions From Longitudinal Cohort Studies To Understanding Clinical Heterogeneity
Most studies investigating the nature of cognitive dysfunction in PD employ prevalent cross-sectional cohorts of patients, usually screened for the presence of dementia using the Mini-Mental State Examination . Such studies are thus inherently biased in terms of patient selection, which limits their potential to investigate more severe cognitive impairment in the form of dementia.
Large cohort studies have been instrumental in efforts to systematically address this aspect of cognitive heterogeneity. Using a community-based epidemiological approach in a population of approximately 700,000 over a 25-month incidence period, the CamPaIGN study was the first to assess the incidence of PD and parkinsonism, and the extent and natural history of cognitive deficits in the ensuing patient cohort . We identified five subgroups of patients at disease presentation, who were impaired on ToL, indicating fronto-striatal deficits, visual pattern recognition memory, indicating temporal lobe dysfunction, both ToL and pattern recognition memory, as well as a cognitively preserved subgroup and a group of patients who demonstrated marked cognitive impairment and had an MMSE score < 24, indicating dementia.
Memory Difficulties In Parkinsons
The most common difficulty for people with PD is remembering information that has previously been learned. Memory has several different processes and types, and people with PD have trouble recalling information but their long-term memory function generally remains intact. Memory cues or choices can help people with PD to retrieve information from the brains long-term storage.3,4
Also Check: Golf Therapy For Parkinson’s
Practical Management Of Pd
Geriatricians are likely to be managing increasing numbers of patients with PD-MCI in the future. Most will not have immediate access to full-neuropsychological assessment in a clinic setting, and it is the authors’ opinion that the MoCA is the most useful screening tool, with published screening cut-offs for both MCI and PDD , and the advantage of an administration time of just 10 min. Further investigations are generally not required, although a routine dementia screen for reversible causes is warranted. Dopamine agonists for motor control and anticholinergic drugs for non-motor symptoms should be used with caution, or not at all. An explanation to the patient and their family that the prognosis of PD-MCI is uncertain but that in some cases it may be progressive is justified if the patient wishes to know this may prompt further discussion about future advanced care planning.
Testing For Cognitive Deficits
There is no clear consensus about the best cognitive tools to use in early PD. This is likely to contribute to the heterogeneity of impairments reported in this field. Neuropsychological tests can be divided into global screening instruments, including those used across a range of disorders as well as those specific to PD, and tests which are designed to probe particular neuropsychological domains.
Recommended Reading: Parkinson’s Disease Prognosis In The Elderly
Epidemiology Predictors And Outcome
Approximately 30%40% of PD patients show cognitive impairment . Prevalence of PD-MCI may be an artifact of application methods of the criteria used for diagnosis . In the article depicting PD-MCI diagnostic criteria and assessment levels , the mean prevalence of such a category was estimated at 27%. By considering cut-off scores of neurocognitive testing, Yarnall et al. reported a variable mean prevalence of PD-MCI of 65.8% , 42.5% and 22.4% below the normative values. Then, two cross-sectional studies estimated the prevalence of PD-MCI at 33% and 64%, respectively . In the Parkinsons Disease Cognitive impairment Study , including 659 non-demented PD patients, the prevalence of PD-MCI was 39.6% in the whole sample. Few longitudinal studies have assessed the incidence of PD-MCI according to the MDS Level II criteria . The most recent study by Nicoletti et al. reported an incidence rate of PD-MCI of 184.0/1000 Pyar.
Although it is difficult to compare among studies, a considerable amount of PD-MCI patients progress to PDD when they are followed from 2 to 5 years after diagnosis . Recently, conversion rates from PD-MCI to PDD have been reported by one study more precisely as from 39% to 50% at a 5-years follow-up . Moreover, findings from longitudinal studies also documented significant rates of reversion to normal cognition of PD-MCI patients ranging from 11% to 27.8% at the same follow-up period .
Genetics: Renewed Importance Of Apoe Gba Variants And Potential Role Of Lysosomal Dysfunction
Given the overlap in clinical symptoms and neuropathologic features among PDD, AD, and DLB, genetic association studies represent a powerful tool to identify areas of potential divergence in molecular mechanism and to highlight shared genetic risk factors that may represent common neurodegenerative pathways. A recent multicenter study of neuropathologically confirmed DLB cases reported 3 genetic loci with significant associations with the DLB phenotype, corresponding to the genes for APOE , Syn , and SCARB2 , a lysosomal protein previously linked to PD. Another study found that the APOE4 allele associated with DLB regardless of the presence of A pathology, suggesting that APOE may have an A-independent effect on DLB and PDD pathogenesis. The importance of APOE was further underscored by the finding that the APOE4 variant was associated with poorer cognitive performance in a study of more than 1,000 patients with PD across multiple centers. Interestingly, the authors noted that the MAPT H1 haplotype, while associated with overall PD risk, did not predict cognitive performance in this dataset. Other recent studies have been mixed with respect to association of the MAPT H1 haplotype and rate of cognitive decline in PD.,
Read Also: Best Parkinson’s Doctors In Nj
Managing Cognitive Impairments In Parkinsons
After a thorough evaluation to rule out other causes of cognitive impairment, patients with PD may be treated with medication, occupational therapy, and/or speech therapy. The medications used to treat cognitive impairments in people with PD are based on treatments used for Alzheimers disease. Occupational therapy can help a person with PD by providing adaptive strategies for daily activities. Speech therapy can help with language functions, as well as information processing. 3,4
Attention And Frontalexecutive Functions
In the human brain, the prefrontal cortex occupies a large portion of the cortical mantle and has extensive connections to most brain regions. It is not surprising then that the prefrontal cortex regulates the flow of information that determines how an individual will behave. The prefrontal cortex allows an individual to pay attention to one event or phenomenon to the exclusion of others, as well as switch among them. It allows one to act automatically or even override automatic actions, and act in a fashion counter to biological or environmental programming. Furthermore, the prefrontal cortex facilitates reasoning. Together, these cognitive abilities are frequently grouped together as frontalexecutive functions. Damage to the prefrontal cortex can substantially disrupt everyday functioning, while leaving many cognitive functions intact, as emphasized by the wellknown case of Phineas Gage .
Also Check: Nocturnal Leg Cramps Parkinson’s
Box 2 Diagnostic Procedure Movement Disorder Society Pdd Criteria8144
Level I Parkinson disease dementia
-
A diagnosis of Parkinson disease based on the UK Brain Bank criteria for PD
-
PD developed prior to the onset of dementia
-
Mini-Mental State Examination below 26
-
Cognitive deficits severe enough to impact daily living independent of motor symptoms
-
Impairment in more than one cognitive domain, that is, at least two of the following aspects:
-
Months Reversed or Seven Backward
-
Lexical Fluency or Clock Drawing
-
MMSE Pentagons
-
Absence of other abnormalities that obscure diagnosis
Level II Comprehensive assessment for characterizing PDD
The level II evaluation assesses four domains:
-
Psychosis
Computerized cognitive testing
Digital computerized cognitive testing, which can be carried out remotely from patients homes, has become an interesting alternative to traditional pen-and-paper testing. Benefits of computerized testing include the opportunity for frequent testing with less learning effects, which increases the sensitivity to detect decline, cost-efficiency and the availability of large normative databases. Opportunities for conducting both remote functional assessments and digital interventions on the same online platform are being studied,.