What Inspired You To Start Looking At This
We were inspired by studies from Heiko Braak in the early 2000s. He proposed that Parkinsons disease may start in the gastrointestinal tract and ascend up the vagus nerve. He based his hypothesis on patterns of brain damage he observed in autopsies of the brains of people with Parkinsons disease. Weve now created an animal model to directly test his hypothesis.
The Polyvagal Theory: Neurophysiological Foundations Of Emotions Attachment Communication And Self
The Vagus Nerve includes a more primitive set of fibers which evolved with ancient, extinct reptiles: the Dorsal Vagus .
The Vagus Nerve also includes a more advanced set of fibers which evolved with appearance of mammals: the Ventral Vagus .
One in six of the Vagus Nerve fibers are of the mylinated type.
Most of the unmylinated fibers regulate organs below the diaphragm such as the gut.
The Dorsal Vagus fibers connect the gut to the brain , and is responsible for gut motility and neuropeptides.
The Dorsal Vagus is activated, but with the Ventral Vagus inhibited, when the Nervous System is in Survival mode, and is responsible for the freeze/shutdown/death feigning response of mammals to life-threatening dangers.
This Enteric Nervous System is optimal when functioning with Ventral Vagus active and in control, such that Dorsal Vagus is not in defensive mode.
People who experience immobilization almost invariably experience gut problems: the two are not independent because both are functions of the Dorsal Vagus.
When the Dorsal Vagus is activated for a immobilization defence, gut and gastric problems will occur.
Problems also occur when fight/flight the defence system is activated chronically, and the activated sympathetic nervous system also dampens the Dorsal and Ventral Vagus Nerve’s ability to support healthy digestive functions.
Extensive Connections Between The Nts With Visceral Organs And Other Brain Structures
The NTS in the brainstem carries and receives visceral primary afferent signals from a variety of visceral regions and organs. Neurons that synapse in the NTS participate into the autonomic reflexes, with a result to regulate the autonomic function. Outputs that go from the NTS are transferred to a large number of other regions of the brain including the paraventricular nucleus of the hypothalamus and the central nucleus of the amygdala as well as to other nuclei in the brainstem . Perhaps, extensive connections between the NTS with visceral organs and other brain structures may elucidate the mechanism of auricular acupuncture.
Therefore, we proposed the auriculovagal afferent pathway both the autonomic and the central nervous system could be modified by auricular vagal stimulation via projections from the ABVN to the NTS .
Auriculovagal afferent pathway : both the autonomic and the central nervous system could be modified by auricular vagal stimulation via projections from the ABVN at the auricular concha to the NTS . NTS: nucleus of the solitary tract DMN: dorsal motor nucleus of the vagus AP: area postrema RVM: rostral ventrolateral medulla LC: locus coeruleus.
You May Like: What Kills A Person With Parkinsons Disease
Read Also: Senator Susan Collins Parkinson’s Disease
Vagus Nerve Stimulation Techniques
Given all of the above, how do these new understandings help us? Well, the good news is the research tells us we can, after all, do something to help ourselves and to improve our condition/minimize our symptoms. This is because, like muscles, an atrophied Vagus Nerve can be strengthened once more through appropriately exercising and stimulating it. In short, we can improve our Vagal Tone to help us begin to escape from being stuck in the “freeze” stress response. In other words, we can learn how to relax our way out of the symptoms of PD.
I first learned about this when I found Cheryl Townsley‘s video on “Sparking” the Vagus Nerve:
I do this exercise daily, using a standard “Pain Gone” pen. This “re-setting” technique demonstrated by Cheryl, shows just how quick and easy VN stimulation techniques can be – I spend just 30 seconds a day on this method.
I also quickly learned that deep breathing exercises are integral to VN stimulation, and practising diaphragmatic breathing for a few minutes a day can end up making a large cumulative difference. I particular recommend the method demonstrated by Ellie Drake:
The next video gives a more in depth explanation about the therapeutic values of VN stimulation in tackling illnesses, and suggests coffee enemas as a method for this
The Vital Need To Encourage Relaxation In People With Parkinsons Disease
for background information on the autonomic nervous systems. The VN regulates the relaxed state of the body and brain, promoting rest, digestion, higher emotionality and sociability. It is responsible for discharging the system from excited states caused by automatic fight or flight responses to perceived threats, as governed by the sympathetic nervous system, and also, when the system perceives extreme threat, recovery from the freeze or playing dead response.
The role of the VN in health should not be understated. When our nervous systems are startled into fight-flight-or-freeze responses, the body quickly becomes inflamed and pain signals result. The ability to rapidly discharge from such a state, once the perceived dangers pass, or not to be hypersensitized to the perception of dangers in the first place, is largely determined by the strength of the VN or Vagal Tone. The VN and its functions therefore have major and primary roles in addressing inflammation and detoxifying the body, and in pain reduction.
In fact, all the major symptoms of Parkinsons can be mapped easily and directly onto a malfunction of one or more of the cranial nerves. Therefore, I suggest that the disease can now be readily and most succinctly understood through the concept that PwP are stuck in freeze and their cranial nerves are critically weak.
Recommended Reading: Robert Wood Johnson Parkinson’s Disease Center
Ultrasonography Of The Vagus Nerve
The USVN imaging was performed using a Voluson 730 Expert ultrasound device with a linear 612 MHz transducer probe, in a depth of 3.5cm. The imaging was performed with the patients resting on their back, with their head bent backward. The probe was placed in the transverse plane several centimetres above the medial ridge of the sternocleidomastoid muscle. The VN can be seen in ultrasound B-mode near the bifurcation of the carotid artery, dorsal to the internal and common carotid arteries, surrounded by a sheet of connective tissue as a structure that is hypoechogenic in the centre and more hyperechogenic in the periphery . VN diameter was measured in the sagittal plane in millimetres proximal to the carotid bulbus, at the level of the distal end of the common carotid artery.
Ultrasonography scan of the vagus nerves in a healthy control subject. Vagus nerve marked with an arrow in an axial image of the neurovascular bundle. Vagus nerve marked with arrows in a sagittal projection. IJV, internal jugular vein CCA, common carotid artery.
Lack Of Oxygen To The Brain In Parkinsons Disease
This mechanism also explains why medicated people with PD seem to deflate as a dose of drugs where off our necks can visibly shorten, our heads move forward and down, our shoulders slump. On the other hand, some people with PD can get symptom relief by exaggerating the head position, and tucking their chin tightly against their chest, opening up the vertebrae at the back of the neck, as exampled in the following video of Michael J. Fox playing the guitar.
Interventions can release imbalances in the tension of the small muscles that hold the skull and the first two vertebrae in relation to each other, and this repositions the atlas and the occiput. Improved alignment of the vertebrae, especially C1 and C2, improves blood flow to the brain and usually brings a rapid improvement in the function of the five nerves necessary for the state of social engagement.
If we can give the body the right information with a soft touch at the right place, the body will balance itself. Because we cannot put C1 and C2 into place and expect them to stay that way permanently, we should repeat balancing techniques frequently, or as needed. Since there is no such thing as a fixed state of balance, it is more useful to think of balancing, an ongoing process.
You May Like: Sam Waterston Tremor
You May Like: Sound Therapy For Parkinson’s Disease
Prevention And Treatment Of Diseases Via Vagal Regulation Of Auricular Acupuncture
The nuclei of the vagus nerve in the brainstem have been implicated as one of the earliest regions in the pathophysiological process of both Alzheimers and Parkinsons diseases. Far-field potentials from brainstem after transcutaneous vagus nerve stimulation at the auricle have been utilized as a noninvasive method in the early diagnosis of neurodegenerative disorders . We suggest that further study is needed on whether auricular acupuncture plays a role in the prevention and treatment of these neurodegenerative disorders via activating the vagal nuclei in the brainstem.
Vagus nerve stimulation has been approved by FDA as an alternative treatment for neuropsychiatric diseases such as epilepsy and depression. In order to avoid the disadvantages of cervical vagus nerve stimulation, less invasive methods including transcutaneous vagus nerve stimulation and electrical auricula-vagus stimulation to stimulate vagal afferences have been proposed. In a pilot study, an overall reduction of seizure frequency was observed in five of seven patients after 9 months of electrical stimulation of the ABVN. It is also found that the electrical stimulation of the ABVN is safe and well tolerated . As a complementary method, it is also proposed that auricular acupuncture may suppress epileptic seizures via activating the parasympathetic nervous system .
Dont Miss: What Is The Difference Between Alzheimers And Parkinsons Disease
Semiquantitation Of Staining Density
For analysis of the each of the immunohistochemical markers, the analyzer was blinded to treatment conditions.
Density measures of TH-immunoreactivity in the striatum and Iba-1-ir in the LC and SN , were conducted as previously described using a QImage R3 camera system with Image J software that measured optical density on a scale from 0 to 1.0 . Measures were obtained by subtracting background from mean staining intensity using every 12th section through the striatum, every 3rd section through the LC, and every 6th section through the SN.
VNS effects on TH in the LC, striatum, and SN of lesioned ratsIba-1-ir was reduced by VNS in the LC and SN of lesioned rats
The measurement area for microglia density analysis is outlined for the LC and the SN . Photomicrographs of LC and SN . VNS had no effect on Iba-1-ir in the LC of saline rats , but resulted in reduced Iba-1-ir in the SN . Lesioned rats had significantly higher Iba-1-ir . VNS reduced Iba-1-ir in lesioned rats . Quantification of results in I and J .
Using an Olympus Fluoview confocal setup, four sections through the SN were imaged to create TH/-synuclein Z-stacks for density analysis in ImageJ. By scrolling through the TRITC channel of each Z-stack, fifteen TH-positive cells were outlined , and density measurements were taken from the corresponding cells in the FITC channel to obtain an individual average for each animal. Data are reported as a percentage of saline non-VNS control rats.
Read Also: Drugs For Parkinson’s Psychosis
Relationship Between The Abvn And The Nucleus Of The Solitary Tract
The anatomical relationship between the ABVN and the nucleus of the solitary tract has been investigated. After applying horseradish peroxidase to the central cut end of the ABVN in the cat, some labeled neuronal terminals were seen in the interstitial, dorsal, dorsolateral, and commissural subnuclei of the NTS some of these terminals may be connected monosynaptically with solitary nucleus neurons which send their axons to visceromotor centers in the brainstem .
The auricular concha is mainly innervated by the ABVN. The relationship between the acupuncture stimulation at auricular concha and the NTS has also been investigated. In an animal study, acupuncture stimulation at auricular concha induced the hypoglycemic effect by activating the firing activities of the neurons in NTS . It is also found that acupuncture-like stimulation at auricular acupoint CO15 activates the cardiac-related neurons in the NTS to evoke cardiovascular inhibition, whereas the inactivation of the NTS with local anesthetics decreased the cardiovascular inhibitory responses evoked by auricular acupuncture .
The Overlaps Between Stress And Parkinsons Disease Part 2
However, the details of this are quite involved, so in this first article on the subject, I shall concentrate on the role of the more evolved, or mammilian, branch of the VN, but for more information on its Polyvagal nature, please see the pioneering research of Dr Stephen Porges.
The Vagus Nerve is one of the Cranial Nerves, and is by far the largest part of the parasympathetic nervous system see
Also Check: Judy Woodruff Health Problems
You May Like: Is Peripheral Neuropathy A Symptom Of Parkinson’s Disease
What Is The Importance Of Having An Animal Model
Prior to this animal model, we were limited to studying the motor features of Parkinsons disease: the slowness of movement, rigidity and tremor. We now have a model that exhibits almost all of the features of Parkinsons disease observed in humans, ranging from gastrointestinal dysfunction to motor dysfunction to anxiety and depression.
How Is Vagus Nerve Stimulation Used
The neurologist programs the strength and timing of the impulses according to each patients individual needs. The settings can be programmed and changed without entering the body, just by using a programming wand connected to a laptop computer. For all patients, the device is programmed to go on for a certain period and then to go off for another period . The device runs continuously, usually with 30 seconds of stimulation alternating with 5 minutes of no stimulation. The patient is usually not aware that its operating. Holding a special magnet near the implanted device causes the device to become active outside of the programmed interval. For people with warnings before their seizures, activating the stimulator with the magnet when the warning occurs may help to stop the seizure. Many patients without auras also experience improved seizure control, however. Settings set by the neurologist typically include a stimulation amplitude of 1.0 to 3.0 mA , a stimulation frequency of 30 Hz , and a pulse width of 500 microseconds. By adjusting these settings, the doctor not only may be able to control more of the patients seizures, but often can also relieve side effects. One study, for instance, found that changing the pulse width eliminated pain that some patients were experiencing. The battery for the stimulator lasts approximately 5-10 years.
Also Check: Sleepiness And Parkinson’s Disease
Neural Exercises And Parkinson’s Disease
for more details and lists of specific exercises which I have found have helped me, based on this concept.
The Dorsal Vagus Nerve framework, however, also sets on us on the path towards exploring and understanding the role of trauma in Parkinson’s Disease, and therefore to seek the connections with other conditions such as Post-Traumatic Stress Disorder and Dystonia. in which Dorsal Vagus activation have a role.. Indeed, in speaking to very many people affected by PD around the world about their history before diagnosis, I’ve found that there is almost universally a major physical or emotional trauma lurking in the background.
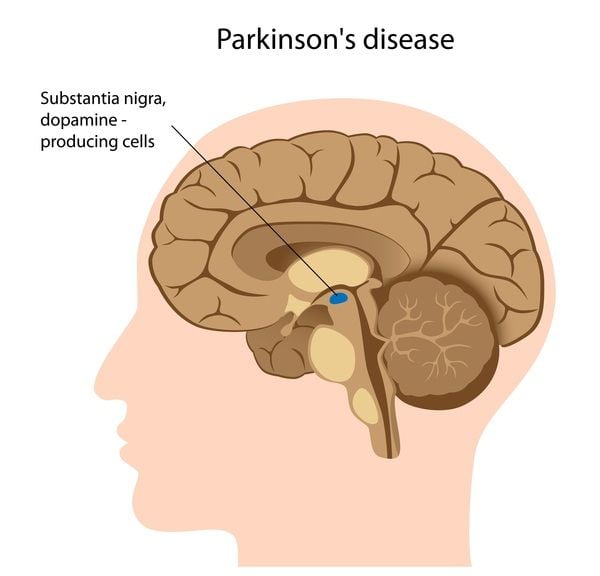
For more of the supporting science behind this explanation for PD, including how signalling from the gut to the brain via the Dorsal Vagus nerve influence dopamine production in the Substantia Nigra, see
Differential Effects Of Vagus Nerve Stimulation Paradigms Guide Clinical Development For Parkinsons Disease
Microburst VNS best reduces motor deficits in a Parkinsons disease lesion model.
-
All VNS treatment paradigms yield greater norepinephrine content in LC targets.
-
SN and LC TH-positive cell loss are best attenuated after microburst VNS.
-
Microburst VNS reduces neuroinflammation and intrasomal -synuclein in the SN.
-
Biomimetic VNS at higher frequencies provides great therapeutic potential for PD.
Read Also: Who Is The Best Parkinson Doctor
Accessing The Healing Power Of The Vagus Nerve: Self
“Social engagement is not a fixed state, nor should the position of C1 and C2 stay fixed. These bones move the instant that our psychological state shifts in moments of happiness, satisfaction, fear, anger, or withdrawal, or when our physiological state shifts among social engagement, dorsal vagus activation, or spinal sympathetic chain activation. A rotation of C1 and C2 can put pressure on the vertebral artery, which supplies the frontal lobes and the brainstem, where the five nerves necessary for social engagement originate.”
This helps explain why people with Parkinson’s Disease faces go blank, and their voices diminish, when symptomatic: the arteries/nerves supplying the head get pinched.
“It only takes one negative thought to bring C1 and C2 out of joint, affecting our posture and physiology. Our nervous system is quick to be upset, it takes a longer time to settle down when we are safe again. Ten small muscles connect the occipital bone at the base of the skull with C1 and C2. Inappropriate tensions in any of these ten muscles are enough to shift and hold C1 and C2 out of joint.”
This also helps to explain why people with Parkinson’s Disease do indeed suffer from lack of oxygen to the brain when symptomatic, and indeed ties together various threads of research I discovered previously in:
The Vagus Nerve And Parkinson’s Disease
I introduced the Vagus Nerve in the context of its role in Parkinson’s Disease. There, I noted that
“…there are actually two major branches of the Vagus Nerve, and this ‘polyvagal’ feature of the nerve in humans is incredibly important for understanding Parkinson’s Disease. This is because the more primitive, or ‘reptilian’, branch of the VN governs ‘playing dead’ – the ‘Freeze’ stress response – which is the state in which people with PD appear to be stuck. However, the details of this are quite involved, so in this first article on the subject, I shall concentrate on the role of the more evolved, or ‘mammilian’, branch of the VN…”
and then, like virtually every other article you will find on the subject, including the vast majority of those I cite in the above article, I proceeded to describe ways to stimulate “the” Vagus Nerve, and espoused its benefits.
I subsequently expanded on the polyvagal characteristics of the Vagal system in
Recommended Reading: The Progression Of Parkinson’s