Assessing Frequency Of Orthostatic Hypotension In Patients With Parkinson Disease
Frequency of orthostatic hypotension among Ethiopian patients with Parkinson disease was shown to be higher than that among healthy controls, with a higher proportion of constipation, urinary urgency, and nocturia symptoms reported in those with PD.
Frequency of orthostatic hypotension in Ethiopian patients with Parkinson disease is higher than in the general population and comparable to other regions, according to study findings published in Ethiopian Journal of Health Sciences.
Considered the most incapacitating nonmotor symptom of PD, OH is highly prevalent among patients with the neurodegnerative condition and is an important morbidity factor in the elderly, leading to falls, fractures, and different types of traumas.
With prevalence of PD expected to double by the year 2030, risk of OH has been noted to be of significant importance among these patient populations as it may also be potentially caused by antiparkinsonian medications used to treat PD, such as levodopa and anticholinergic drugs.
Identifying presence of OH in early PD is a major diagnostic challenge as often the alternative diagnosis of multiple system atrophy is usually favored, noted lead study author Abenet Tafesse Mengesha, MD, MSc, associate professor of Neurology, Department of Neurology, College of Health Sciences, Addis Ababa University, in Addis Ababa, Ethiopia.
Mengesha concluded that larger prospective studies are warranted to consolidate the present study findings.
Reference
About This Crispr Gene Editing Research News
Abstract
An RNA-targeting CRISPRCas13d system alleviates disease-related phenotypes in Huntingtons disease models
Huntingtons disease is a fatal, dominantly inherited neurodegenerative disorder caused by CAG trinucleotide expansion in exon 1 of the huntingtin gene.
Since the reduction of pathogenic mutant HTT messenger RNA is therapeutic, we developed a mutant allele-sensitive CAGEX RNA-targeting CRISPRCas13d system that eliminates toxic CAGEX RNA in fibroblasts derived from patients with HD and induced pluripotent stem cell-derived neurons.
We show that intrastriatal delivery of Cas13dCAGEX via an adeno-associated viral vector selectively reduces mutant HTT mRNA and protein levels in the striatum of heterozygous zQ175 mice, a model of HD.
This also led to improved motor coordination, attenuated striatal atrophy and reduction of mutant HTT protein aggregates. These phenotypic improvements lasted for at least eight months without adverse effects and with minimal off-target transcriptomic effects.
Taken together, we demonstrate proof of principle of an RNA-targeting CRISPRCas13d system as a therapeutic approach for HD, a strategy with implications for the treatment of other dominantly inherited disorders.
Can An Off Episode Be Prevented
Eventually, most people with PD develop OFF episodes. Some people develop OFF episodes sooner than others.
Researchers have found evidence that taking high doses of levodopa may increase your risk of OFF episodes. It may cause greater fluctuations in your dopamine levels.
Its important for your doctor to prescribe the lowest dose of levodopa necessary to manage your symptoms. This may help limit fluctuations in dopamine and reduce your risk of OFF episodes.
If you think you might be experiencing OFF episodes, let your doctor know. They may adjust your prescribed dose or formulation of levodopa/carbidopa. They may also prescribe other treatments to manage OFF episodes.
If youre experiencing OFF episodes, your doctor may recommend one or more changes to your treatment plan.
They may:
In some cases, your doctor may recommend deep brain stimulation . In this procedure, a surgeon implants electrodes in the brain and a small internal pulse generator in the chest or abdomen. The internal pulse generator sends electrical signals to the brain to help control symptoms of DB.
Each treatment option carries a different risk of side effects. Ask your doctor about the potential benefits and risks of different treatment approaches.
You May Like: Drugs Used For Parkinson’s Disease
What Helps On/off Episodes
There are a few different steps you can consider taking to increase your symptom-free hours during the day.
Change the dosage or timing of your carbidopa/levodopa: Taking your medication at different times, or increasing your dose, may help reduce your off time.
Try a different medication: Your doctor may suggest another medication to add to your regimen, or a new carbidopa/levodopa option, to help reduce off episodes. You may also consider newer treatments for off time. For example, an inhaled levodopa powder for off episodes was approved by the FDA in 2018.
Adjust your diet: Because levodopa is a protein building block, it competes for absorption in the brain with other proteins. Its best not to eat a high-protein meal before taking your medication. For example, you may save fish, meat, and cheese for dinner and eat more carbs and vegetables during the day.
Consider a clinical trial: If youre interested, there are also several treatments in development for off time in Parkinsons disease.
Participating in clinical trials helps create the treatments of tomorrow. Start your search for a local Parkinsons disease clinical trial opportunity.
When Do You Get Dyskinesia
Most people are on levodopa for 5 to 10 years before they notice dyskinesia. And it usually starts when Parkinson’s is under good control. This is called peak dyskinesia because it happens when your dopamine levels are highest. After a while, symptoms may start sooner and last longer than this peak time.
But they still happen when levodopa is keeping your symptoms in check. Your doctor may call this being âonâ with dyskinesia.
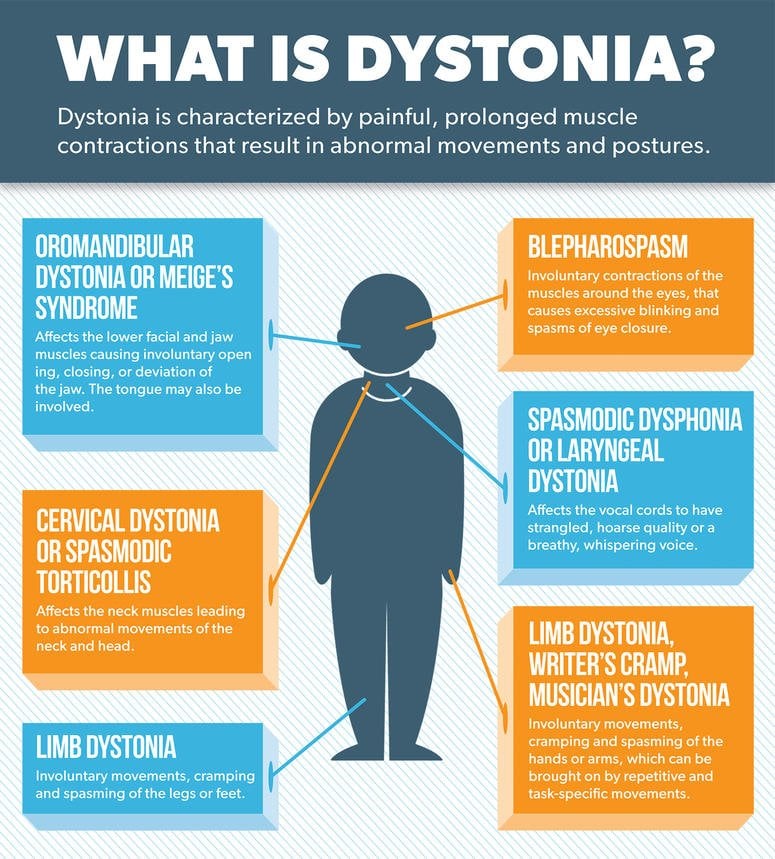
Dyskinesia is sometimes lumped together with a problem called motor fluctuations. But theyâre not the same thing. Motor fluctuations are when Parkinson’s symptoms come back during times your meds arenât working. This can happen if levodopa wears off before you take your next dose or a new dose doesnât kick in right away.
You May Like: What Causes Shaking In Parkinson’s Disease
When Should I See My Healthcare Provider Or When Should I Seek Care
You should see your healthcare provider as recommended, or if you notice changes in your symptoms or the effectiveness of your medication. Adjustments to medications and dosages can make a huge difference in how Parkinsons affects your life.
When should I go to ER?
Your healthcare provider can give you guidance and information on signs or symptoms that mean you should go to the hospital or seek medical care. In general, you should seek care if you fall, especially when you lose consciousness or might have an injury to your head, neck, chest, back or abdomen.
What Causes On/off Episodes In Parkinsons Disease
On/off episodes, also known as off time, typically happen more often as Parkinsons disease progresses, and levodopa becomes less effective.
Carbidopa/levodopa is considered the gold standard in Parkinsons disease treatment, meaning its the most effective for treating motor symptoms, such as tremor, rigidity, and bradykinesia . Levodopa works by crossing the blood-brain barrier and converting into dopamine, low levels of which are believed to be the cause of Parkinsons symptoms. Adding carbidopa to levodopa helps prevent levodopa from breaking down before it crosses into the brain, which helps reduce side effects like nausea and vomiting.
Some people who have Parkinsons start taking levodopa at around three doses per day. If you start experiencing off episodes, your doctor may increase your dose to four or more times per day.
Off time is common: According to patient surveys, around half of patients who take levodopa report experiencing wearing off periods. Of those patients, 25% experience it 3 to 6 hours per day, and 52% have symptoms for 1 to 3 hours a day.
Dont Miss: What Are Some Signs Of Parkinsons Disease
Don’t Miss: Big Physical Therapy For Parkinson’s
How Do Treatments Differ
MS treatments can ease your symptoms during an attack or slow down the diseaseâs effects on your body.
Steroids like prednisone calm the inflammation that damages your nerves.
Plasma exchange is another therapy if steroids donât work. Your doctor will use a machine to remove the plasma portion of your blood. The plasma gets mixed with a protein solution and put back into your body.
Some people with both diseases who take anti-inflammatory medicines like steroids see their Parkinsonâs symptoms get better.
Disease-modifying treatments slow down MS nerve damage and disability. They include:
Medications to treat Parkinsonâs either raise your dopamine levels or offer a substitute. They can ease Parkinsonâs symptoms like tremors. Over time, they may become less effective.
Medicines used to treat Parkinsonâs include:
Deep-brain stimulation is another treatment for Parkinsonâs. A doctor places electrodes into your brain. They send out electric pulses that ease symptoms in your body.
Show Sources
How Soon After Treatment Will I Feel Better And How Long Will It Take To Recover
The time it takes to recover and see the effects of Parkinson’s disease treatments depends strongly on the type of treatments, the severity of the condition and other factors. Your healthcare provider is the best person to offer more information about what you can expect from treatment. The information they give you can consider any unique factors that might affect what you experience.
You May Like: Traumatic Brain Injury And Parkinson’s Disease
Exploring The Clinical Burden Of Off Periods In Parkinson Disease
Supplements and Featured Publications
ABSTRACT
Parkinson disease, the second-most-common neurodegenerative disorder, affects approximately 1 million individuals in the United States, and this number is projected to increase to 1.2 million by 2030. Characterized pathologically by degeneration of dopaminergic neurons, with widespread pathology in nondopaminergic systems, Parkinson disease leads to an array of motor and nonmotor symptoms that can significantly impact an affected individuals quality of life. Treatments for Parkinson disease typically focus on controlling the motor symptoms of the disease, including treating OFF periods when motor symptoms return. OFF periods can occur for many individuals with Parkinson disease, especially as the disease progresses, and can pose a substantial burden to those with the disease and their caregivers. Available treatments for OFF periods may help alleviate this burden.
Am J Manag Care. 2020 26:S255-S264.
For author information and disclosures, see end of text.
Introduction
Diagnosis of PD usually occurs after age 50 years, and incidence rises with increasing age.1 In most populations, incidence of PD is twice as common in men as in women.1 In a population-based study conducted in Olmsted County, Minnesota, incidence was observed to increase over a 30-year period, particularly in men 70 years or older .4
Etiology
Diagnosis of Parkinson Disease
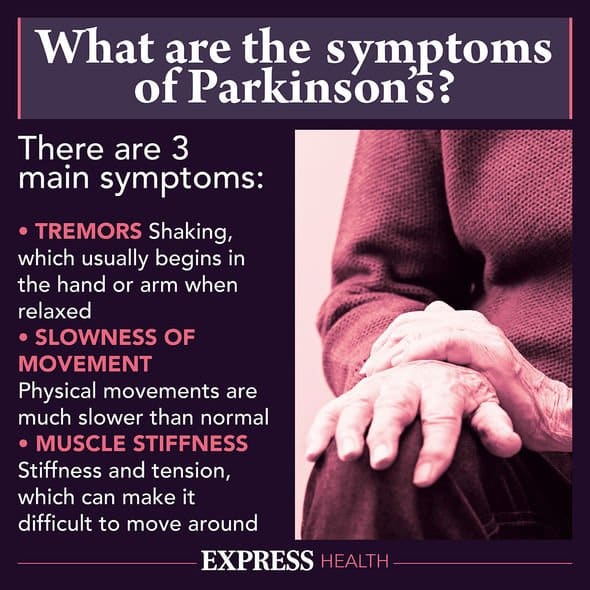
Symptoms of Parkinson Disease
Nonmotor Symptoms
What Medications And Treatments Are Used
Medication treatments for Parkinsons disease fall into two categories: Direct treatments and symptom treatments. Direct treatments target Parkinsons itself. Symptom treatments only treat certain effects of the disease.
Medications
Medications that treat Parkinsons disease do so in multiple ways. Because of that, drugs that do one or more of the following are most likely:
Several medications treat specific symptoms of Parkinson’s disease. Symptoms treated often include the following:
- Erectile and sexual dysfunction.
- Hallucinations and other psychosis symptoms.
Deep brain stimulation
In years past, surgery was an option to intentionally damage and scar a part of your brain that was malfunctioning because of Parkinsons disease. Today, that same effect is possible using deep-brain stimulation, which uses an implanted device to deliver a mild electrical current to those same areas.
The major advantage is that deep-brain stimulation is reversible, while intentional scarring damage is not. This treatment approach is almost always an option in later stages of Parkinson’s disease when levodopa therapy becomes less effective, and in people who have tremor that doesnt seem to respond to the usual medications.
Experimental treatments
Researchers are exploring other possible treatments that could help with Parkinsons disease. While these arent widely available, they do offer hope to people with this condition. Some of the experimental treatment approaches include:
Also Check: When Do You Stop Driving With Parkinson’s
Comparison Between Clinician Assessments And Patient Self
CWOQ-9 corresponded with clinician identification of WO in 734 of 763 patients clinicians disagreed with the CWOQ-9 considering the presence of WO in 337 of 1,071 cases. Considering the clinician identification as a gold standard, the sensitivity of CWOQ-9 was 96.2% , the specificity of CWOQ-9 was 45.8% . We further compared the patients of clinician identification and CWOQ-9 to the patients of clinicians identification and CWOQ-9 . Results showed that patients of clinician identification and CWOQ-9 were characterized by a younger age at onset , a longer disease duration , a higher H& Y staging , a higher CWOQ-9 score, and higher frequencies in most of the motor and non-motor symptoms, compared with patients of clinician identification and CWOQ-9 .
Table 3. Comparison of the characteristics between WO patients of different assessment methods.
How Is It Diagnosed
Diagnosing Parkinson’s disease is mostly a clinical process, meaning it relies heavily on a healthcare provider examining your symptoms, asking you questions and reviewing your medical history. Some diagnostic and lab tests are possible, but these are usually needed to rule out other conditions or certain causes. However, most lab tests aren’t necessary unless you don’t respond to treatment for Parkinson’s disease, which can indicate you have another condition.
Recommended Reading: Supplements For Parkinson’s Tremors
Management Of The Return Of Symptoms In Parkinson’s Disease
Thanks for joining us at the OFF Talk Podcast series where we discuss Parkinson’s disease, managing OFF periods and the use of on-demand therapies. Each podcast will be a one-on-one discussion with a leading Movement Disorder specialist. These podcasts also include important safety information. This podcast, “Management of the Return of Symptoms in Parkinson’s Disease,” is intended for US healthcare professionals and is brought to you by Acorda Therapeutics. My name is Julia Overman and I’m a Medical Science Liaison for Acorda Therapeutics. I have the great pleasure of introducing Dr. Jennifer Durphy, Associate Professor of Neurology at Albany Medical Center. Dr. Durphy, thank you so much for joining us today.
It’s my pleasure to be here.
Let’s start out by discussing OFF episodes, or the return of symptoms in patients with Parkinson’s disease. Dr. Durphy, can you give us a little bit of background on how and why OFF periods occur in Parkinson’s disease?
I see. Thank you for that overview of OFF periods.
Could you tell us a little bit about how OFF periods are managed in patients with Parkinson’s disease? And has this changed over time?
So it sounds like there are a variety of options to treat a patient’s return of symptoms.
When managing a patient’s OFF periods, what might the clinic visit look like to determine if an as-needed treatment like INBRIJA is an appropriate option? How has the option to use INBRIJA impacted your patient care?
Is There A Link
Some people have MS and Parkinsonâs.
Research suggests that the damage that MS causes to your brain can lead some people to develop Parkinsonâs later on.
If you have MS, your immune system triggers ongoing inflammation. This can create lesions in your brain that cause Parkinsonâs disease. If lesions form in certain spots in your brain, they can affect how it makes dopamine.
You May Like: Does Botox Help Parkinson’s
New Formulation Of Old Drug Shows Promise For Off Episodes
Administering an approved drug, apomorphine, by a new method dissolving it under the tongue can relieve wearing off episodes for people with Parkinsons disease , according to the results of a small, phase II clinical trial. The study appears in the July 19 online edition of Movement Disorders.
Levodopa, usually given as Sinemet®, is the gold-standard therapy for PD movement symptoms. But most people who take the drug for several years eventually experience fluctuations in its effectiveness, known as off periods, when movement symptoms return. While medication adjustments can help in the long term, the only approved therapy to rapidly address or rescue someone from such off periods is apomorphine, a drug that is injected under the skin. Although it is effective, injectable apomorphine is not widely used.
Seeking a more convenient way of giving the drug, Cynapsus Therapeutics, Inc., a company based in Toronto, Canada, developed APL-130277. It is a thin strip, about the width of a penny and very similar in appearance to a Listerine® breath strip, and is infused with apomorphine and a substance to prevent skin irritation. Holding the strip under the tongue quickly releases the drug.
Results:
What Does It Mean?
Reference
Hauser RA, Olanow CW, Dzyngel B, et al. . Sublingual Apomorphine for the Acute Conversion of OFF to ON in Parkinsons Disease. Movement Disorders DOI: 10.1002/mds.26697
Read Also: Big Physical Therapy For Parkinsonâs
The Symptom Spectrum Of Wearing
In a satellite symposium held at the 2019 EAN Congress, the speakers discussed the spectrum of motor and non-motor fluctuations associated with the wearing-off of levodopa treatment for Parkinsons disease, and steps to prevent and manage these troublesome symptoms.
Impact of wearing-off on motor symptoms
As Parkinsons disease progresses over time from a stable treated disease to an advanced state there is a recurrence of motor symptoms during wearing-off including tremor, dystonia, muscle spasms, postural instability, slowness and gait difficulties. Wearing-off occurs frequently in about 80% of patients within 4 years from therapy initiation .1-3
Wearing-off during levodopa treatment may be detected even at the early stages of PD and is underestimated by routine neurological clinical evaluation. The number of symptoms, both motor and nonmotor, increases along with disease duration and unsurprisingly has a negative impact on patients quality of life.4
Patients with PD rate wearing-off as the greatest challenge with their levodopa therapy. Activities of daily living are rated as most bothersome by patients, because they are most limited during OFF time.5 Patients would prefer treatments that increase the amount of ON time, and for which they are able to predict the occurrence of OFF time to within 30 minutes.
Wearing-off is the greatest challenge of levodopa therapy, which occurs within 4 years of therapy initiation, and may be detected even earlier
Recommended Reading: What To Do For Parkinson’s Cough
What Is The On/off Phenomenon In Parkinsons
The ON/OFF phenomenon in PD happens when someone experiences flares of symptoms between regularly scheduled doses of levodopa.
During an ON episode, the levodopa is working well and symptoms improve. During an OFF episode, the levodopa isnt working and symptoms return or get worse.
A 2018 review found that 25 to 50 percent of people with PD developed OFF episodes within 2 years of beginning treatment with levodopa. Within 10 years of starting treatment, most people with PD had OFF episodes.
OFF episodes can affect different people in different ways. They may follow a predictable pattern or occur unpredictably. They may set in suddenly or gradually.
The researchers behind a