What Are The Symptoms Of Parkinson Disease
Parkinson disease symptoms usually start out mild, and then progressively get much worse. The first signs are often so subtle that many people don’t seek medical attention at first. These are common symptoms of Parkinson disease:
- Tremors that affect the face and jaw, legs, arms, and hands
- Slow, stiff walking
How Is It Treated And Is There A Cure
For now, Parkinsons disease is not curable, but there are multiple ways to manage its symptoms. The treatments can also vary from person to person, depending on their specific symptoms and how well certain treatments work. Medications are the primary way to treat this condition.
A secondary treatment option is a surgery to implant a device that will deliver a mild electrical current to part of your brain . There are also some experimental options, such as stem cell-based treatments, but their availability often varies, and many aren’t an option for people with Parkinsons disease.
Medicines For Parkinsons Disease
Medicines can help treat the symptoms of Parkinsons by:
- Increasing the level of dopamine in the brain
- Having an effect on other brain chemicals, such as neurotransmitters, which transfer information between brain cells
- Helping control non-movement symptoms
The main therapy for Parkinsons is levodopa. Nerve cells use levodopa to make dopamine to replenish the brains dwindling supply. Usually, people take levodopa along with another medication called carbidopa. Carbidopa prevents or reduces some of the side effects of levodopa therapy such as nausea, vomiting, low blood pressure, and restlessness and reduces the amount of levodopa needed to improve symptoms.
People living with Parkinsons disease should never stop taking levodopa without telling their doctor. Suddenly stopping the drug may have serious side effects, like being unable to move or having difficulty breathing.
The doctor may prescribe other medicines to treat Parkinsons symptoms, including:
- Dopamine agonists to stimulate the production of dopamine in the brain
- Enzyme inhibitors to increase the amount of dopamine by slowing down the enzymes that break down dopamine in the brain
- Amantadine to help reduce involuntary movements
- Anticholinergic drugs to reduce tremors and muscle rigidity
Don’t Miss: How Does Parkinson’s Medication Work
What Will A Cure For Parkinson’s Look Like
Parkinson’s varies so much from person to person. There are over 40 symptoms of Parkinsons. Tremor. Pain. Hallucinations. Everyones experience is different.
Because of this, there may not be a single ‘cure’.
Instead, we may need a range of different therapies to meet the needs of the individual and their specific form of the condition.
This mix may include treatments, therapies and strategies that can:
- slow or stop the progression of the condition
- replace or repair lost or damaged brain cells
- control and manage particular symptoms
- diagnose Parkinson’s at the earliest possible stage.
And this could involve medical treatments, such as drugs and surgical approaches, as well as lifestyle changes, for example to diet and exercise.
Dopaminergic Features And Their Treatment
Patients with PD usually present with features indicative of degeneration of nigrostriatal pathways. A useful clinical definition for PD is asymmetric onset of an akinetic rigid syndrome with resting tremor and a good response to levodopa. When applied by neurologists with an interest in movement disorders, this definition has a pathological correlation exceeding 98%. When treatment is considered appropriate, and this is a topic discussed in detail below, a variety of options is available. The use of dopaminergic drugs improves motor function, significantly reduces both the morbidity and mortality of PD, and improves quality of life.
Levodopa remains the drug most commonly used in PD. It is very effective in improving bradykinesia and rigidity, and in practice remains the gold standard against which other drugs are judged. Some studies, predominantly in vitro, have suggested that levodopa may be toxic. However, such data are conflicting, and some laboratory studies have suggested a growth factor-like effect for levodopa. Overall, the pre-clinical evidence for levodopa toxicity is not convincing and there are no data to indicate that any toxic action is of clinical relevance.
Table 1
Percentage of patients remaining on dopamine agonist monotherapy at years 14 and years 15 during treatment trials
Recommended Reading: Management Of Parkinson’s Disease
When To Contact A Doctor
If you have a family history of Parkinsons disease, you may wish to talk with a doctor about your potential risks or even explore genetic testing. However, its important to remember that not all people with a family history of Parkinsons disease will be affected.
Signs of Parkinsons disease can be different for every person. Parkinsons is usually separated into premotor, motor, and cognitive stages. These dont necessarily occur in a particular order, and not everyone will experience them all.
As explained by the Parkinsons Foundation, common early symptoms include:
- tremor, or involuntary shaking of the hands
Human Umbilical Cord Blood Cells And Plasma
Saneron CCEL Therapeutics, Inc. supplied the frozen hUCB cells and plasma. The Sepax 2 full-automated cell processing system separated the hUCB cells and plasma for use. Before freezing, the BacT/ALERT Microbial detection system was used to examine the hUCB cells and plasma units as aseptic. The hUCB units were purchased commercially from GenCure by Saneron CCELTherapeutics, Inc. for research purposes under USF IRB# 131111. The de-identified hUCB units were processed by Saneron CCEL Therapeutics, Inc. using the Sepax 2 full-automated cell processing system which allowed for the sterile collection of both hUCB cells and plasma. Results for infectious disease testing of maternal blood samples, collected shortly after birth, was provided by GenCure, for infectious disease markers of HIV, hepatitis B and C, syphilis, CMV, and HTLV I& II. Each hUCB unit in the study was negative for all infectious disease markers. Saneron CCEL Therapeutics, Inc. supplied all the processed, cryopreserved, hUCB cells and plasma that was used in this study.
Read Also: Parkinson’s And Loss Of Appetite
When Should I See My Healthcare Provider Or When Should I Seek Care
You should see your healthcare provider as recommended, or if you notice changes in your symptoms or the effectiveness of your medication. Adjustments to medications and dosages can make a huge difference in how Parkinsons affects your life.
When should I go to ER?
Your healthcare provider can give you guidance and information on signs or symptoms that mean you should go to the hospital or seek medical care. In general, you should seek care if you fall, especially when you lose consciousness or might have an injury to your head, neck, chest, back or abdomen.
Symptoms Of Parkinsons Disease
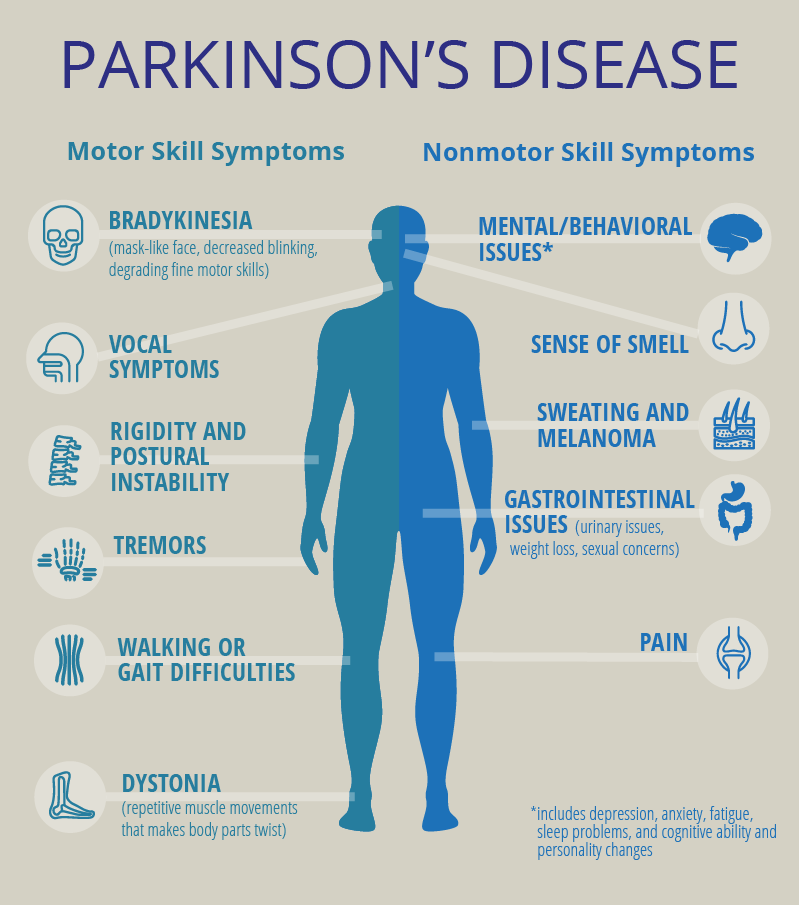
Parkinsons has four main symptoms:
- Tremor in hands, arms, legs, jaw, or head
- Muscle stiffness, where muscle remains contracted for a long time
- Slowness of movement
- Impaired balance and coordination, sometimes leading to falls
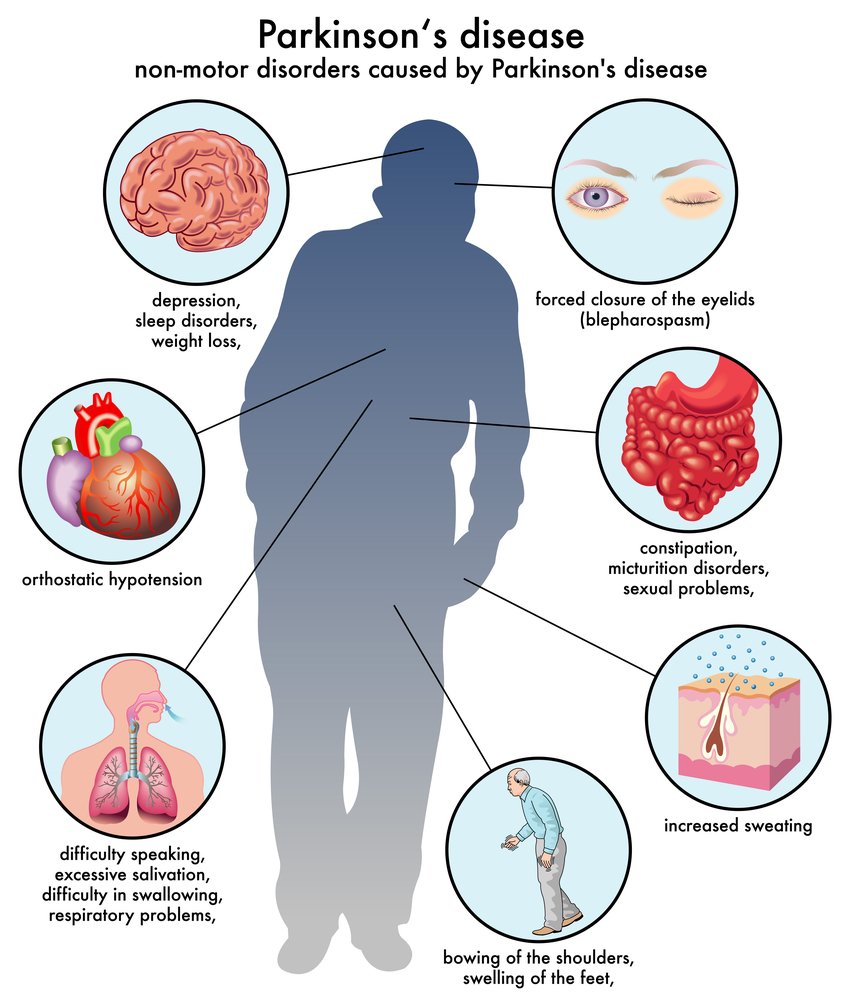
Other symptoms may include:
The symptoms of Parkinsons and the rate of progression differ among individuals. Early symptoms of this disease are subtle and occur gradually. For example, people may feel mild tremors or have difficulty getting out of a chair. They may notice that they speak too softly, or that their handwriting is slow and looks cramped or small. Friends or family members may be the first to notice changes in someone with early Parkinsons. They may see that the persons face lacks expression and animation, or that the person does not move an arm or leg normally.
People with Parkinson’s disease often develop a parkinsonian gait that includes a tendency to lean forward take small, quick steps and reduce swinging their arms. They also may have trouble initiating or continuing movement.
Symptoms often begin on one side of the body or even in one limb on one side of the body. As the disease progresses, it eventually affects both sides. However, the symptoms may still be more severe on one side than on the other.
Also Check: What Are Some Early Signs Of Parkinson’s Disease
Complementary And Alternative Medicine
There isn’t strong evidence that massage is beneficial for Parkinson’s disease, but it might help reduce muscle tension and can help you relax.
Acupuncture and dietary supplements have not been found to be effective in controlling the symptoms of Parkinson’s disease. In particular, research has shown coenzyme Q-10 and creatine had no effects beyond that of placebos. Vitamin E supplements raised concerns that they could be harmful in Parkinson’s disease.
Some patients find that medical marijuana or CBD oil helps with symptoms of pain and may help improve sleep, but there is no specific evidence supporting benefits.
Living With Parkinson Disease
These measures can help you live well with Parkinson disease:
- An exercise routine can help keep muscles flexible and mobile. Exercise also releases natural brain chemicals that can improve emotional well-being.
- High protein meals can benefit your brain chemistry
- Physical, occupational, and speech therapy can help your ability to care for yourself and communicate with others
- If you or your family has questions about Parkinson disease, want information about treatment, or need to find support, you can contact the American Parkinson Disease Association.
Don’t Miss: De Que Mueren Los Enfermos De Parkinson
Physical Occupational And Speech Therapy
Physical, occupational and speech therapists can be important partners in the treatment of Parkinsons disease. Physical therapy can improve your gait and direct you to the right exercise regimen. Occupational therapy can be helpful to maximize your fine motor skills. Speech therapy can be useful to address speech and language barriers that may arise with Parkinsons disease.
Managing The Social And Emotional Impact
The effects of PD are broad and impact on the social and economic life of the person and their family from the time of diagnosis in a variety of ways.
Coping and adjusting to the diagnosis, facing increasing challenges at work and planning for the future can be a daunting undertaking.
Navigating this newfound uncertainty requires careful consideration and appropriate specialised support.
As the disorder progresses, caregiver burden also increases and quality of life can decrease.
A social worker specialised in movement disorders such as PD can assist the person with PD, their caregiver and family negotiate the challenges faced across the life time of the persons PD.
Social workers are highly skilled professionals who can assist you and your loved ones by:
- providing a range of different therapys like counselling
- assistance with linking to other support services
- directing you to financial support services
- information provision of entitlements for care packages
- help to facilitate suitable respite arrangements for the caregiver
- assistance and support with navigating the pathway to permanent residential care if the need arises.
After receiving a diagnosis of PD it is normal to experience a change in mood. A social worker has the appropriate specialised skills to help you deal with the reaction to your diagnosis.
Social workers are specifically trained to support you in understanding how best to manage such symptoms.
Recommended Reading: Beginning Of Parkinson’s Symptoms
/6preventing Parkinsons Disease Symptoms
Parkinsons disease is a neurological movement disorder triggered by a loss of dopamine. Dopamines role is to send messages to the part of your brain that controls movement and coordination. Symptoms start slowly at first, but as the disease progresses, it can greatly impact your routine activities. The disease usually develops in middle or late life, most commonly around age 60 or older.
Even though the risk increases with time, a new study has identified an activity that could help halt symptoms and modify the associated risks.
Clinical Neurosciences, University of Turku and Neurocenter, Turku University Hospital, Turku, Finland
Correspondence to: Dr. Tomi Kuusimäki, Division of Clinical Neurosciences, Turku University Hospital, Hämeentie 11, POB 52, FIN-20521, Turku, Finland E-mail:
Haidar Al-Abdulrasul MD
Clinical Neurosciences, University of Turku and Neurocenter, Turku University Hospital, Turku, Finland
Department of Neurology, Helsinki University Hospital and Department of Clinical Neurosciences , University of Helsinki, Helsinki, Finland
School of Pharmacy, University of Eastern Finland, Kuopio, Finland
Kuopio Research Centre of Geriatric Care, School of Pharmacy, University of Eastern Finland, Kuopio, Finland
School of Pharmacy, University of Eastern Finland, Kuopio, Finland
Kuopio Research Centre of Geriatric Care, School of Pharmacy, University of Eastern Finland, Kuopio, Finland
Haidar Al-Abdulrasul MD
How Is Parkinsons Disease Diagnosed
No single test exists to diagnose Parkinsons disease. Doctors rely on a physical examination and your symptom history to help make a diagnosis. They will look specifically for motor-related symptoms, such as how you walk.
Your doctor may run some tests to rule out other potential causes of your symptoms, like stroke. Tests could include imaging tests, blood tests, and more. Doctors may even prescribe Parkinsons disease medications to see if a persons symptoms improve.
If a person has a considerable family history of Parkinsons disease, its possible that doctors may be able to conduct genetic testing. But this is costly and uncommon.
Don’t Miss: Cardinal Signs Of Parkinson’s
How Soon After Treatment Will I Feel Better And How Long Will It Take To Recover
The time it takes to recover and see the effects of Parkinson’s disease treatments depends strongly on the type of treatments, the severity of the condition and other factors. Your healthcare provider is the best person to offer more information about what you can expect from treatment. The information they give you can consider any unique factors that might affect what you experience.
Whats The Connection Between Parkinsons And Infections
Some severe viral and bacterial infections lead to encephalitis, which is a dangerous condition that causes inflammation in the brain. Encephalitis can cause Parkinson-like symptoms. This has led researchers to explore the connections between viral infections and Parkinsonism.
To date, this research has been limited. Its possible that infections play a role in the development of Parkinsons disease, but researchers have yet to find any clear connections.
Viruses being investigated include:
To be clear, getting one of these viruses does not mean that you will get Parkinsons disease. Researchers are trying to determine if infectious illnesses may change something in a persons body that makes them more vulnerable to the condition.
Researchers are trying to see if there are connections between illnesses in earlier life and increased risks for Parkinsons disease.
According to a 2019 review of studies , there is some evidence suggesting that:
- People who get the flu vaccination may be less likely to get Parkinsons disease than people who dont.
- People with higher levels of the herpes simplex virus in their bodies may have more severe Parkinsons disease symptoms.
- People with Parkinsons are more likely to have had the Epstein-Barr virus than the general population.
- People with a history of hepatitis C may be more likely to get Parkinsons disease than others.
Risk factors for Parkinsons disease include:
Recommended Reading: Best Cbd Oil For Parkinson’s
How Is It Diagnosed
Diagnosing Parkinson’s disease is mostly a clinical process, meaning it relies heavily on a healthcare provider examining your symptoms, asking you questions and reviewing your medical history. Some diagnostic and lab tests are possible, but these are usually needed to rule out other conditions or certain causes. However, most lab tests aren’t necessary unless you don’t respond to treatment for Parkinson’s disease, which can indicate you have another condition.
New Medications For Off Time
A number of new medications approved recently are designed to reduce OFF time. These medications fall into two major categories:
- Medications that lengthen the effect of a carbidopa/levodopa dose
- Medications that are used as needed if medication effects wear off
Well give specific examples below. In general, new medications that extend the length of a carbidopa/levodopa dose are used if OFF time is somewhat predictable and occurs prior to next dose. New medications that are used as needed are most beneficial when OFF time is not predictable.
New medications that lengthen the effect of a dose of carbidopa/levodopa
- Istradefylline is an adenosine A2A receptor antagonist which was approved in the US in 2019 as an add-on therapy to levodopa for treatment of OFF time in PD. Unlike many of the other medications, it has a novel mechanism of action and is the first medication in its class to be approved for PD. It acts on the adenosine receptor, which modulates the dopaminergic system, but is not directly dopaminergic. The drug was developed in Japan and underwent clinical trials both in Japan and in the US.
- Opicapone is a catechol-O-methyltransferase inhibitor that is taken once a day. It was approved in the US in 2020 as an add-on therapy to levodopa for motor fluctuations.
New formulations of levodopa designed to be used as needed if medication effects wear off
Other medications used as needed if medication effects wear off
You May Like: Boyd Gaines Parkinson’s Disease
Animal Preparation And Transplantation
All experimental procedures were approved by the University of South Florida Institutional Animal Care and Use Committee and followed the ARRIVE 2.0 guidelines . All investigators were blind to the treatment condition until after completion of all data analyses. This study used 14 months-old male C57BL/6NJ and C57BL/6N-Tg 15Mjff/J mice . The Tg mice overexpressed the wild type human -synuclein, with validated phenotypic PD-like progressive nigrostriatal dopamine depletion and motor deficits . All mice were included in the study, had free access to food and water, and housed under normal conditions . Mice were randomly assigned by a staff not involved in the study to one group: Wt Con , Wt+P , Wt + hUCB+P , Tg Con , Tg + P and Tg+hUCB+P . 0.4×106 hUCB cells in 50L of hUCB plasma or only 50L of hUCB plasma were intravenously injected using the jugular vein to the treatment group . Sample size ensured adequate power to detect 25% treatment effect size.
Fig. 6: Treatment timeline.
Behavioral tests at baseline were performed on Day 0 prior to transplantation. On Day 1, intravenous transplantation with P or hUCB+P was performed. Behavioral tests were conducted again on day 1, 3, and 7 post transplantation. Animals were sacrificed on day 7 for brain and gut for fluorescent insitu hybridization and immunohistochemistry to assess PD histopathology.
You can also search for this author inPubMed