Visual Perceptual Dysfunction And Hallucinations: Multiple Network Involvement
Patients with Parkinsons disease exhibit both subtle visuospatial deficits , and visuoperceptive deficits , in some patients from early in the disease . These deficits become more marked and more common with disease progression and show high sensitivity in detecting the transition to PDD . Indeed impairment on the Pentagon Copying Test from the MMSE at baseline has been shown to be predictive of PDD at 5-year follow-up .
Visual hallucinations are also well-recognized in Parkinsons disease and are typically complex, consisting of well-formed people, animals or objects . Although they can be induced by anti-parkinsonian drugs, correlations between use of these agents and presence of hallucinations are actually relatively weak, and instead cognitive impairment has been shown to be the major risk factor, indicating that they are a core symptom of the dementing process . Visual hallucinations generally occur in the latter stages of the disease course with a progressive nature . Their presence is a strong predictor of PDD and indeed the prevalence of hallucinations in PDD is 70% . Although insight is initially maintained in patients with PDD, 81% will lose insight over 3 years , which severely affects quality of life for both patients and caregivers .
Future Directions And Treatment Strategies
As this review has shown, the dysfunctional neural networks underlying the cognitive symptoms of PDD are diverse and distributed throughout the brain. There is overlap between network functions, each of which depend on differing primary neurotransmitters. In addition, evidence suggests that neurotransmitters can modulate the functional effects of one another , and thereby damage to one network during the pathogenesis of PDD may in turn influence dysfunction in another . Furthermore, as discussed in detail above, the cellular-level pathology causing damage to these networks in PDD is heterogeneous, while the effects of different genes on the pathophysiology of the disorder is only now being slowly unravelled.
Apda In Your Community
APDAParkinson’s Disease SymptomsLewy Bodies, Dementia, and Parkinsons What Does it all Mean?
Here are two common scenarios that may sound familiar:
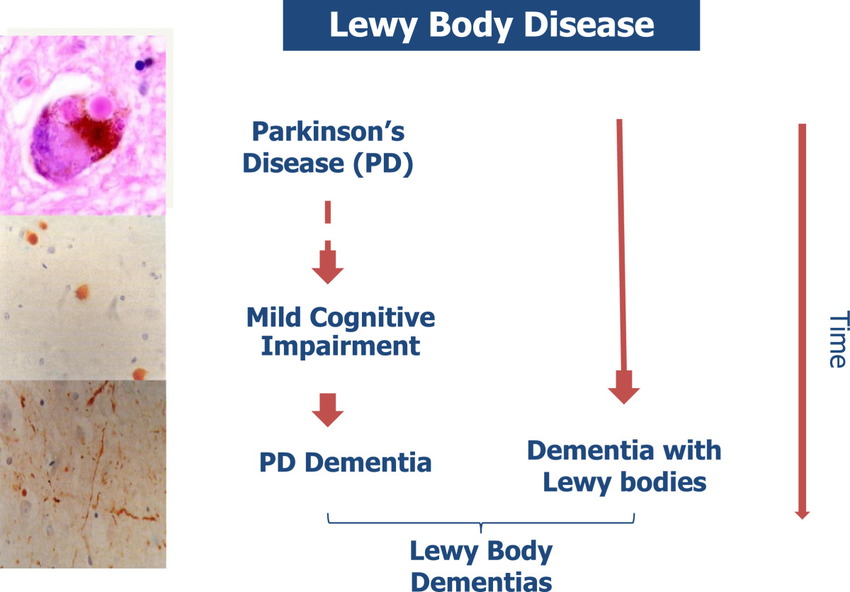
Scenario 1A patient develops a series of neurologic symptoms, is evaluated by a neurologist and is told that she has Parkinsons disease . She then visits another neurologist for a second opinion and is told she has Lewy Body Dementia .
Scenario 2A patient has his first visit with his neurologist and is told that he has PD, at a subsequent visit the diagnosis is changed to Parkinsons disease dementia , and at a follow up visit the diagnosis is changed yet again to Dementia with Lewy Bodies .
Both of these situations understandably cause great uncertainty and frustration.
Also Check: How Can You Test For Parkinson’s Disease
Conceptualization Of The Diseases Needs And Interventions
Both dementia and PD are incurable and progressive diseases with often complex problems and needs, for which tailored interventions are available . For dementia, experts agree that recognizing its eventual terminal nature is the basis for anticipating future problems and an impetus to the provision of adequate palliative care . Some advocate advanced dementia to be a terminal disease to support eligibility for palliative care. However, as about half of dementia patients never reach an advanced stage , it may be a late trigger to initiate palliative care. There is no consensus, however, at which stage palliative care in dementia should start .
Table 2. Conceptualization of the disease, needs of patients and family caregivers, and interventions.
For PD there are no curative treatments either, but the success of dopaminergic replacement therapy and deep brain stimulation has enabled the majority of patients to live independently with a relatively low symptom burden for the first 10 years after diagnosis-when they live up to a decade . This may contribute to PD generally not being recognized as an illness for which a palliative approach may be helpful . A US patient and caregivers council recommends palliative care to be available from diagnosis of PD . This is also the ideal of the European Parkinson’s Disease Association although they emphasize that when to start palliative care is an individual decision.
Types And Symptoms Of Dementia
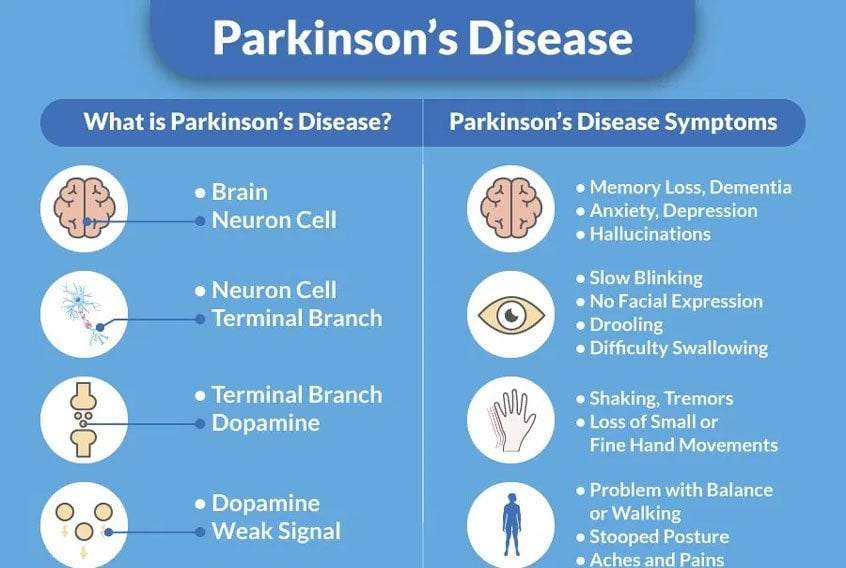
Changes in the structure and chemistry of the brain cause memory and thinking problems in Parkinsons disease . The protein alpha-synuclein is central to Parkinsons. This protein forms sticky clumps, called Lewy bodies, that disrupt normal brain functioning. Parkinsons dementia is thought to be related to Lewy bodies.
Also Check: Nursing Home Care For Parkinson’s Patients
Treatments For Parkinsons Disease Dementia And Dementia With Lewy Bodies
Treatments for DLB are similar to PDD and are aimed at symptom control. The motor symptoms of slowness, stiffness and walking difficulties can be treated with Levodopa. However, Levodopa can cause or exacerbate hallucinations, making it difficult to use it as a treatment for patients who have or are at risk of having hallucinations. Sometimes, clinicians will need to treat the hallucinations more aggressively in order for a patient to tolerate Levodopa given to help the motor symptoms. On the flipside, anti-psychotic medications to control hallucinations can worsen motor symptoms, so treating all the symptoms of LBD simultaneously can be a tricky balancing act.
What Is Lewy Body Dementia
Lewy body dementia is not a single disorder but rather a spectrum of closely-related disorders involving disturbances of cognition, behavior, sleep, movement and autonomic function.
In these progressive disorders, Lewy bodies build up in the brain. Lewy bodies in the brain stem cause a disruption in the production of chemical messengers called dopamine. Too little dopamine can cause parkinsonism, a clinical syndrome thats characterized by tremor, bradykinesia , rigidity and postural instability. Parkinsonism can be caused by Parkinsons disease itself as well as by other underlying neurological conditions such as LBD. These Lewy bodies are also found throughout other areas of the brain, including the cerebral cortex. The neurotransmitter acetylcholine is also depleted, causing disruption of perception, thinking and behavior.
A German neurologist, Friederich H. Lewy, first discovered the abnormal protein deposits in the early 1900s as he was conducting research on Parkinsons disease.
Don’t Miss: Effect Of Exercise On Parkinson’s Disease
Number Of People Affected
Parkinsons disease is thought to affect about 2 percent of Americans over 65. Of those, about 50 to 80 percent will go on to develop Parkinsons-related dementia.1 The Parkinsons Foundation estimates that nearly 1 million Americans will be living with Parkinsons by 2020. The disease affects 1.5 times more men than women.7
Approximately 5.8 million Americans are currently living with Alzheimers disease. That number is expected to increase to 14 million by 2050.8 There is little difference between numbers of men and women who develop Alzheimers, but there are more women with the disease, because women tend to live longer than men.3
Lewy Bodies: More Than Lbd
LBD is characterized by the presence of Lewy bodies in the nerve cells of the brain, meaning that LBD patients have Lewy bodies in the brain.2 However, Lewy bodies are also common with other conditions, such as Alzheimer’s and Parkinsons disease. In fact, most people with PD also have Lewy bodies in their brain. However, even if they have Lewy bodies, not all Parkinsons patients will also develop LBD.2
Read Also: What Is A Pull Test For Parkinson Disease
Executive Dysfunction Is Due To Disruption Of The Fronto
The prefrontal cortices are implicated in executive function , and distinct areas of prefrontal cortex have strong functional connections with the striatum via parallel dopamine-dependent cortico-striatal loops . Functional MRI imaging in patients with Parkinsons disease relates executive impairments on set shifting and working memory tasks to hypo-activation within the fronto-striatal loops connecting dorsolateral and ventrolateral prefrontal cortices, striatum and thalamus . However, such hypo-activation was only present during task phases that specifically required co-activation with the striatum in controls, indicating that striatal dysfunction was the determining factor in executive impairment in Parkinsons disease rather than frontal dysfunction. Both the globus pallidus internus and caudate are heavily affected by dopaminergic degeneration , and PET studies have specifically implicated dysfunction of these two structures in interruption of normal processing in the fronto-striatal network for example, patients with Parkinsons disease demonstrating executive impairments on tasks involving planning or random number generation show significantly altered outflow activity from the pallidum to the frontal cortices. In addition, other studies have shown strong correlations between dopamine depletion in the head of the caudate and deficits on executive tasks such as object alternation and the Stroop Test .
Prognostic Factors For Development Of Parkinsons Disease Dementia
In the clinic the diagnosis of PDD is based upon the Movement Disorders Society Task Force criteria , which incorporates detection of the cognitive features described above. However, it is recognized that early identification of patients at risk of developing PDD is useful in order to monitor them more closely so that therapeutic and supportive strategies can be implemented at a stage of the disease when they are likely to have greatest efficacy. Detailed neuropsychological testing, although able to detect early subclinical deficits, is not widely available, and therefore identification of clinical features with high predictive value for PDD has pragmatic value for clinicians. Large longitudinal cohort studies have demonstrated that inability to copy the intersecting pentagons figure on the MMSE, impairments of semantic verbal fluency and recognition memory, and development of a postural instability and gait difficulty motor phenotype are significant predictors for PDD . Errors on the Pill Questionnaire and presence of REM sleep behavioural disorder are also associated with later development of PDD, although their positive predictive values are lower .
Don’t Miss: Dealing With Parkinson’s Dementia
Living With Parkinson Disease
These measures can help you live well with Parkinson disease:
- An exercise routine can help keep muscles flexible and mobile. Exercise also releases natural brain chemicals that can improve emotional well-being.
- High protein meals can benefit your brain chemistry
- Physical, occupational, and speech therapy can help your ability to care for yourself and communicate with others
- If you or your family has questions about Parkinson disease, want information about treatment, or need to find support, you can contact the American Parkinson Disease Association.
Memory And Thinking Problems
You may experience forgetfulness, slowed thinking and difficulty concentrating. You might find it harder to follow conversations, and remember some words and names. This can make communication difficult.
You may also find it increasingly difficult to make decisions, plan activities and solve problems. This can make everyday activities harder.
Don’t Miss: What Kills A Person With Parkinson’s Disease
Treatment Of Pdd And Dlb
Unfortunately, since both types of Lewy Body Dementia often display similar symptoms, patients suffering from either PDD of DLB can get misdiagnosed and subsequently prescribed the incorrect medication and method of treatment. Caregivers and medical professionals alike can increase their understanding of symptoms for each disease to help them more quickly and accurately diagnose and treat each one.
The Lewy Body Dementia Resource Center provides literature, support groups, and help for caregivers grappling with care and treatment of a loved one who has Lewy Body Dementia. Our helpline is available 12 hours a day, 7 days a week for caregivers who have questions or are in need of support. Our online resource center seeks to bring awareness and support to caregivers of those suffering with Lewy Body Dementia. Please dont hesitate to reach out to us.
Thanks For Signing Up
We are proud to have you as a part of our community. To ensure you receive the latest Parkinsons news, research updates and more, please check your email for a message from us. If you do not see our email, it may be in your spam folder. Just mark as not spam and you should receive our emails as expected.
Don’t Miss: Foods To Help With Parkinson’s Disease
How Is Parkinson Disease Treated
Parkinson disease can’t be cured. But there are different therapies that can help control symptoms. Many of the medicines used to treat Parkinson disease help to offset the loss of the chemical dopamine in the brain. Most of these medicines help manage symptoms quite successfully.
A procedure called deep brain stimulation may also be used to treat Parkinson disease. It sends electrical impulses into the brain to help control tremors and twitching movements. Some people may need surgery to manage Parkinson disease symptoms. Surgery may involve destroying small areas of brain tissue responsible for the symptoms. However, these surgeries are rarely done since deep brain stimulation is now available.
Clinical Variables And Covariates
A movement disorder specialist assessed severity of motor symptoms using Part III of the Movement Disorder Society revision of the Unified Parkinson Disease Rating Scale and the Modified Hoehn and Yahr scale. Age, education, sex, disease duration , total LEDD, and GDS-15 were included as covariates. Site differences were seen at baseline with regard to education, motor severity, and cognitive severity/status , and thus site was also included as a covariate. Differences in time between visits for participants was accounted for by including age in all analytic models.
Also Check: Stem Cells For Parkinson’s Disease Therapy
Theres A Spectrum Of Pathologies
Scientists have been examining this linkand how the two diseases often overlapfor some time, but still arent completely certain how they contribute to one another. As a result, physicians sometimes group the diseases into different combinations when making diagnoses.
Dementia in Parkinsons patients can present itself in varying forms. In some cases, the Parkinsons pathology can trigger the dementia pathologya situation that results in whats known as Parkinsons disease dementia, says Dr. Aaron Ritter, Director of the Clinical Research Program at the Cleveland Clinic Lou Ruvo Center for Brain Health.
A substantial subset of folks with Parkinsons who live long enough, will develop dementia, Ritter said.Its separate from Alzheimers, but its likely related to Parkinsons pathology, a sort of spreading of Parkinsons.
In other cases, patients may develop a form of dementia like Alzheimers separately from their Parkinsons disease, though this isnt visible until after death, through an autopsy.
Many people with Parkinsons may also develop Lewy body dementia shortly after their diagnosis. When you have Parkinsons, and see cognitive declineor things like hallucinations and delusionsup to a year after your Parkinsons diagnosis, you may have Lewy body dementia, Oguh said.
Degeneration In The Mesocortical Dopamine Network Contributes To Executive Dysfunction
However, dopamine-dependent neural circuitry underlying executive deficits in Parkinsons disease may not be limited to the fronto-striatal network alone. The mesocortical dopamine network originates in the midbrain ventral tegmental area and projects diffusely to neocortical areas, particularly prefrontal, insular and cingulate cortices . Release of dopamine from this network modulates prefrontal D2 receptors and thereby facilitates cognitive flexibility, a core feature of executive processing . Insular cortex in particular is considered to mediate such flexibility, acting as a hub to recruit other cognitive circuits such as the fronto-parietal network . In support of this, insular lesions in human patients have been shown to impair performance on tasks requiring cognitive flexibility .
Also Check: Hoarse Voice Parkinson’s Disease
How Can We Support The Sleep/wake Cycle Of Pdd
For people with PDD who are confused about the day-night cycle, some daily strategies can be helpful. At night, starting a lights out routine that happens at the same hour every day, where all curtains are closed and lights are turned off, can help the person understand that it is sleep time. During the day, opening the curtains, allowing the person with PDD to spend as much time in the daylight as possible, avoiding naps, and organizing stimulating activities, can be helpful. Having lots of calendars and clocks in every room might also help a person with PDD be less confused about the time of day.
Dementia And Parkinsons Disease
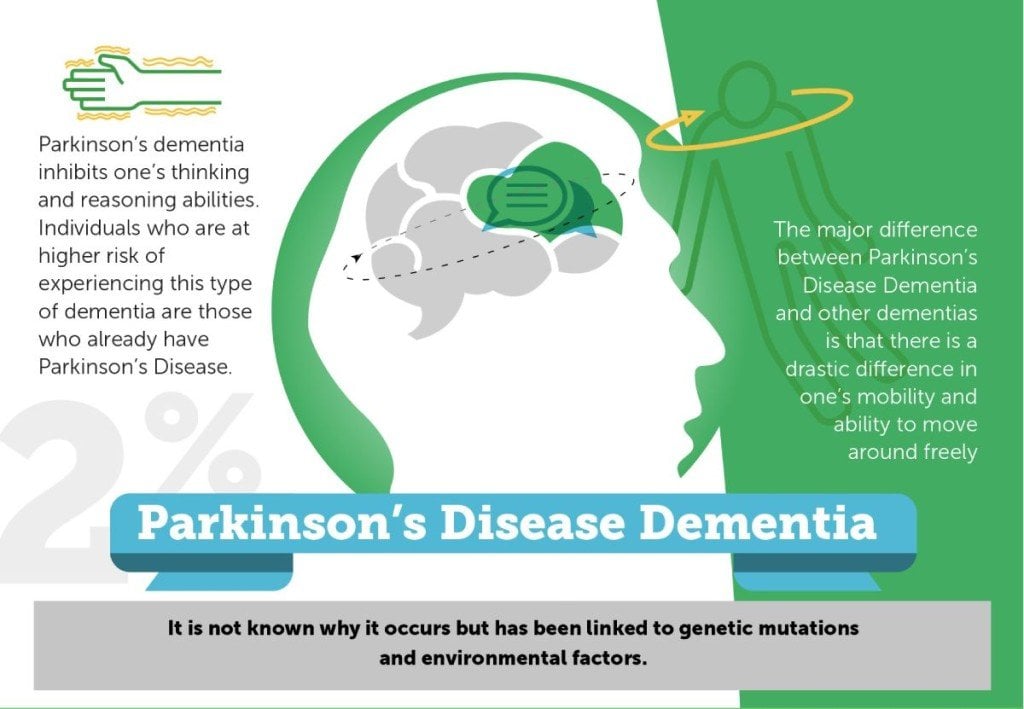
The most recognizable symptom of Parkinsons disease is muscle rigidity that makes walking and mobility difficult. Tremors are also seen frequently in people with PD, and cognitive issues can develop later as the disease progresses. As symptoms begin to worsen, changes in memory, concentration, and focus may also occur. Dementia often appears 10-15 years after diagnosis as a seniors cognitive function declines. This memory loss can cause problems with the ability to communicate verbally, inhibit problem solving skills and abstract reasoning, reduce your loved ones attention span, and hinder his or her ability to relate to other people.
Recommended Reading: What Are The Signs Of Parkinson’s Disease
Clinical And Neuropathological Differences Between Parkinson’s Disease Parkinson’s Disease Dementia And Dementia With Lewy Bodies Current Issues And Future Directions
Institute of Neuroscience, Campus for Ageing and Vitality, Newcastle University, Newcastle-upon-Tyne, UK
First Department of Neurology, National and Kapodistrian University of Athens Medical School, Athens, Greece
Biomedical Research Foundation of the Academy of Athens, Athens, Greece
Institute of Neuroscience, Campus for Ageing and Vitality, Newcastle University, Newcastle-upon-Tyne, UK
First Department of Neurology, National and Kapodistrian University of Athens Medical School, Athens, Greece
Biomedical Research Foundation of the Academy of Athens, Athens, Greece
See A Doctor If Youre Noticing Symptoms Beyond Parkinsons
Sometimes the mood or memory changes a person experiences cannot entirely be explained just by Parkinsons. If this is the case, the caregiver should explore other diagnoses, because if something cannot be explained by Parkinsons, theres certainly a risk of it being dementia, Oguh said.
She added that some signs to look for include increased memory and behavioral problems, like mood swings, anxiety or depression. Psychiatric behaviors, like hallucinations, delusions or paranoia, cannot just be explained by Parkinsons, and are more likely to be caused by a form of dementia like Lewy body dementia.
Oguh urged caregivers to be aware of changing symptoms like these.
I think sometimes family members are able to realize sooner than the patient, Oguh said. Often the patient might lack insight as to what is happening. I would encourage family members to seek expert opinion and treatment options.
You May Like: How Is Parkinson’s Disease Associated With Headaches