If You Experience Stiffness In Your Shoulder It May Be Due To Parkinsons
While those with Parkinsons may experience stiffness in several body parts, experts say that having frozen shoulder, also known as adhesive capsulitis or periarthritis, is particularly linked with PD. Shoulder stiffness is, in fact, one of the conditions associated with Parkinsons disease, a neurodegenerative disorder caused by a lack of dopamine in the brain, explains Very Well Health.
When a patient develops frozen shoulder, the connective tissues that encase the bones, ligaments, and tendons in that area thicken and tighten around the shoulder joint. When this happens, movement becomes restricted, causing pain and stiffness.
According to the Mayo Clinic, symptoms of frozen shouldertypically begin gradually, worsen over time and then resolve, usually within one to three years. The health authority says this often occurs in three distinct stages: the freezing stage, the frozen stage, and the thawing stage. In the freezing stage, the patient typically experiences reduced range of motion along with joint pain in one shoulder. The frozen stage is typically less painful, but as the shoulder becomes stiffer, many people lose most or all function in the affected shoulder. In the thawing stage, the patient begins to regain range of motion.
Dont Miss: Diseases Similar To Parkinsons
Practical Pain Management Interviewed Jori E Fleisher Md Msce Assistant Professor Of Neurology And Population Health At The Marlene And Paolo Fresco Institute For Parkinsons And Movement Disorders At Nyu Langone Medical Center A Parkinsons Foundation Center Of Excellence About The Challenges Facing Women With Parkinson’s Disease
Della Volpe K. Pain in Parkinsons Disease: A Spotlight on Women. Pract Pain Manag. 2017 17.
Chronic pain occurs in 30% to 85% of patients with Parkinsons disease , particularly in women, and is one of the strongest predictors of poor quality of life in patients with this disease.¹² Dr. Fleisher responds to questions that offer clinicians insights into the pain experienced by women who have Parkinson’s disease.
Multiple Regression Analysis Of Qol Improvements
Multivariate regression analysis was used to adjust for confounding factors between the two groups, and absolute changes in QOL were taken as results . Preoperative EQ-5D and PD were important independent predictors of EQ-5D changes. After adjusting for confounding demographic, comorbid, and unilateral or bilateral TKA, PD predicted a decrease in EQ-5D improvement at the LFU .
Table 3 Multiple regression model for improvement of QOL
The data confirmed that PD was not an important independent predictor of changes in PDQ, while preoperative PDQ and unilateral or bilateral TKA were proved to be important independent predictors of changes in PDQ. Bilateral TKA indicated a decrease in postoperative PDQ improvement. Similarly, PD was not a significant independent predictor of changes in PHQ-9. Multivariate regression analysis found that prior depression and anxiety and longer preoperative duration of symptoms were predictors of diminished improvement in PHQ-9.
Recommended Reading: Parkinson’s And Loss Of Appetite
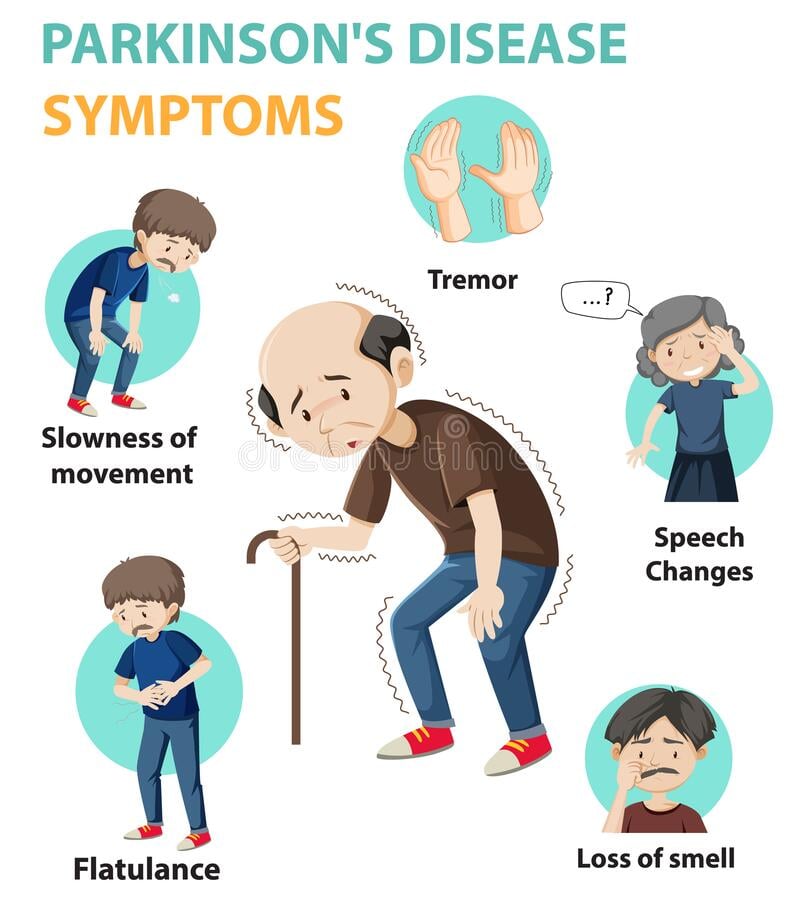
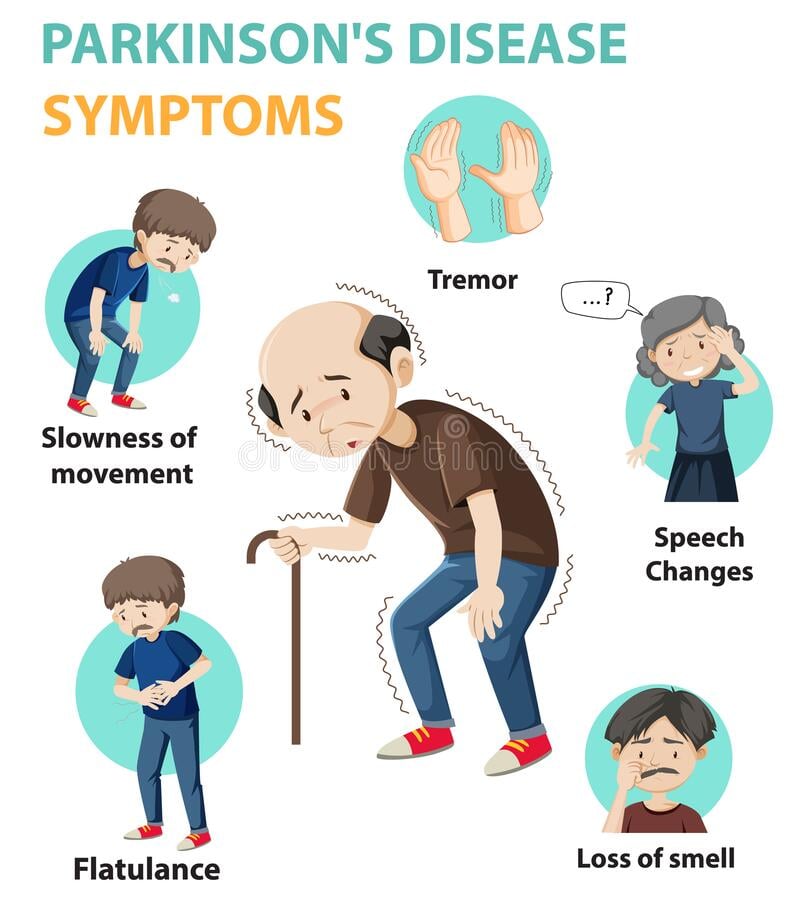
What Causes Parkinsons Disease
Parkinsons disease occurs when nerve cells in an area of the brain called the substantia nigra become impaired or die. These cells normally produce dopamine, a chemical that helps the cells of the brain communicate . When these nerve cells become impaired or die, they produce less dopamine. Dopamine is especially important for the operation of another area of the brain called the basal ganglia. This area of the brain is responsible for organizing the brains commands for body movement. The loss of dopamine causes the movement symptoms seen in people with Parkinsons disease.
People with Parkinsons disease also lose another neurotransmitter called norepinephrine. This chemical is needed for proper functioning of the sympathetic nervous system. This system controls some of the bodys autonomic functions such as digestion, heart rate, blood pressure and breathing. Loss of norepinephrine causes some of the non-movement-related symptoms of Parkinsons disease.
Scientists arent sure what causes the neurons that produce these neurotransmitter chemicals to die.
Examples Of Pain Scales
Visual analog scale
A visual analog scale measures a continuum of a chosen present characteristic. For example, the experienced pain that a patient feels extends over a continuum from no pain to an extreme intensity of pain. This range of perceived pain appears continuous for the patient. Pain does not appear as an ordinary scale with jumps between the values, such as discrete, moderate, or severe. Word descriptors are only used in both ends of the line, which is usually 100 mm in length. This valuation is very subjective and best used within an individual and not between groups of individuals at the same time point. Most experts argue that a VAS at best can produce data of ordinal type. This is important to consider in the statistical analysis of VAS data. Rank ordering of scores rather than the exact values might be the best way to handle patient registrations on the 100 mm line.
Brief Pain Inventory
The Brief Pain Inventory was initially created for the purpose of measuring pain in cancer patients. It measures pain relief, pain quality, and patient perception of the cause of pain in terms of pain intensity and pain interference .
You May Like: Parkinsonism Is Characterized By The Loss Of
The Cranial Nerves And Parkinson’s Disease
for more about this in the context of PD.
However, I believe there is something unique about the Social Engagement system in humans, even amongst mammals: our hands. We humans also use hands for expressing our emotions in very significant ways too. Indeed, we can communicate very profoundly like this: we have even developed sign languages, so we can and do literally talk with our hands.
We can also hush each other with hands without making sound ourselves – meaning we can communicate that serious danger is present requiring everyone in the social group to keep quiet to avoid attracting attention, in such a way that we don’t attract attention ourselves.
Orienting is also an important part of the Cranial Nerve function for threat/safety evaluation, including the ability to turn eyes or ears to the source of potential threat. But with our hands we can also, naturally, orient each other to potential threats which we individually may have detected, within social groups – pointing a finger in direction of danger, for example, or signalling to the group to stop in its tracks.
We can also make very distinct sounds and a wide range of “calls to action” directly with our hands: clapping, clicking fingers, whistling through the fingers, not to mention beating drums, etc.
I have just communicated all this to you through my hands too, because I typed these words with my fingers!
What You Need To Know About Joint Pain Joint And Muscle Pain With Parkinsons
You should seek medical attention for any pain you experience. If the pain is caused by an infection, you should seek medical attention as soon as possible. You can take over-the-counter medications like acetaminophen or ibuprofen. If your pain is more intense, you can try heating or applying ice to the joint. Alternatively, you can also try applying heat to the affected area. To relieve the pain, you should stay away from the activities that cause you to have joint pain. A doctor can prescribe you dietary supplements, such as glucosamine, that are effective in reducing your symptoms.
If you fall or are hit on the leg and notice any swelling or deformity in your knee, you should seek medical attention. If you cant put weight on your leg, it could be a sign of a more serious ailment. If you are experiencing any of these signs and symptoms, you should consult a doctor immediately. The most important thing to do is to be patient and do not panic. The pain you experience is normal and is not related to any other health problems.
Joint And Muscle Pain With Parkinsons Osteoarthritis is a condition that causes degeneration of the joints. People suffering from this disease will suffer from chronic pain in their joints and stiffness. They may also suffer from depression and sleep disturbances. Fortunately, there are treatments for osteoarthritis. These treatments include a change of diet and exercise. The good news is that you can get relief from your osteoarthritis symptoms today.
Read Also: Is There A Medical Test For Parkinson’s
Pain In Parkinsons Disease
Parkinsons patients suffer from the same pain other people have, often amplified by the motor dysfunction, but they also have additional pain problems unique to PD. Lower back pain and back of he neck pain are most common. Strengthening exercises or stretching may be helpful. Identifying the cause of the pain is essential in treating the pain. Treatments include physical therapy, medications, and alternative therapies like Reiki, acupuncture and massage.
Who Should I See To Discuss My Parkinsons Pain
Your first point of contact should be your primary doctor. Whether that means your family doctor, neurologist, or Movement Disorder Specialist , start by asking them how to manage your pain. They may prescribe you one of the medications listed above, offer suggestions about altering your lifestyle, or refer you to a pain specialist.
Pain management specialists are physicians with specialized training in the field of evaluating, diagnosing, and treating pain so, speaking to one of these specialists might be helpful for you. Be sure to get a referral from your primary care doctor, though, to ensure you are visiting a physician who understands the complexity of treating Parkinsons-specific pain.
Health and wellness providers like physical therapists, acupuncturists, and massage therapists can also be valuable members of your care team. Be willing to try new things and approach alternative therapies with an open mind, as no ones path with Parkinsons pain is the same. What works for someone else may not work for you and vice versa. Consider visiting different specialists to find a treatment plan that works best for you.
Dont Miss: Vascular Parkinsonism And Cognitive Impairment
Also Check: Does Parkinson’s Disease Affect The Eyes
Tips For Dealing With Chronic Pain
Chronic pain is one that last more than 3-6 months , or pain that extends behind the expected period of healing. This blog post explains the different types of pain caused by Parkinsons disease and how to address pain brought on by the disease, by medications, or by comorbid disease. It is always best to treat pain before it becomes chronic.
Qol In Pd Patients After Tka
TKA has been recognized to improve QOL in patients with KOA. TKA can relieve pain and make patients feel satisfied, and even improve the quality of life of octogenarian patients to the level of septuagenarian patients . Szmyd J et al. also proved that TKA significantly reduced the pain intensity of patients and significantly improved the patients ability to live daily. In a 2-year follow-up after TKA, DT Wei et al. found that improvements in knee specific outcomes were closely associated with improvements in health-related quality of life . Although the number of PD patients with TKA is relatively small, favorable surgical outcomes with TKA in these patients have occasionally been reported. For example, Sun QC et al. used KSS score to illustrate that for PD patients, both knee function and range of motion were greatly improved after TKA, especially in pain. However, no studies have reported the improvement of QOL in PD patients after TKA. Montiel et al. . questioned the improvement of QOL in PD patients after TKA, but did not draw a conclusion on whether QOL was improved or not. Therefore, we tried to further explain the improvement of QOL in PD patients with TKA.
Read Also: University Of Florida Parkinson’s Center
Other Symptoms: Aging Or Pd
Because the biggest risk factor for developing PD is age , skeletal problems associated with aging are often experienced by people with PD. While it is not clear that PD increases the risk or even the severity of these other skeletal conditions, the problems of PD can make the symptoms of these conditions more prominent.
- Osteoarthritis, the joint damage associated with general wear and tear on the joints, is nearly universal in aging. Osteoarthritis tends to affect larger joints such as the hip and knee.
- Arthritis of the spine is also very common. This may contribute to the development of spinal stenosis, narrowing of the canal in the spine that houses the spinal cord. In severe cases, spinal stenosis causes damage to the nerves as they exit the spine or even to the spinal cord itself.
- Disorders of the fibrous discs between the bones of the spine can also cause pain, or limb numbness or weakness.
Revisiting Pain In Pdthe 50 Shades Of Pain Experienced By Parkinsons Patients
Pain is a quality of life issue for people with Parkinsons disease and can be under treated by doctors who may assume that is worsens as the disease progresses, although for some pain is an initial symptom of PD. This article helps focus your physicians attention in the right direction to accurately diagnose your pain.
You May Like: Effective Treatment For Parkinson’s Disease
Muscle Weakness And Rigidity
As his Parkinsons progresses, Dad complains that his stiffness is slowing him down. The frequency and intensity with which it occurs seem to be increasing. To better understand the disease and how it relates to the body, I decided to explore the research.
In an abstract of a literature review published by the American Journal of Physical Medicine & Rehabilitation, the authors stated that isokinetic muscle strength was decreased in patients with Parkinsons disease and that muscle weakness was not specifically related to tremor or rigidity.
Read Also: Ultrasound Treatment For Parkinsons Disease
Hand And Finger Stimulation Exercises
I have done a lot of hand/finger stimulation and experimented to optimize such exercises, in the spirit of Curiosity and Play. I’ve personally found significant benefit in pursuing this line of research. Indeed, I have managed to recover a lot of my independence and quality of life through hand and finger therapy, and I know just how much of a major part it has played in my own progressive symptom reduction.
I therefore encourage everyone with PD to do as much hand and finger stimulation as possible, through games and play and self-discovery. By doing nothing, the only thing that will happen is that out situation will rapidly become worse, because we will lose the use of our hands quicker and consign ourselves to increased suffering. By applying neuroplasticity techniques , we can delay the worse ravishes of the disease or even, like in my own case, continuously push the symptoms back and recover some independence. I feel this is an important message for those newly diagnosed, in particular.
Here are some suggestions of the type of stimulatory exercises and games which can help, more ideas which I have personally found beneficial will be provided in forthcoming articles.
Read Also: Lifespan For Parkinson’s Disease
Im In Pain But I Dont Want To Take Carbidopa/levodopa Yet Because My Doctor Says It Will Only Work For Five Years Any Advice
It is true that as time passes and your disease progresses, you will have to take higher doses to replace the dopamine your body can no longer produce. However, the rate of dopamine loss is different for everyone. What your doctor may be telling you is that after taking carbidopa/levodopa for some time, you may begin to experience side effects like dyskinesia. It is important to understand that while you may experience this unwanted side effect, for example, you still benefit from the carbidopa/levodopa. If you believe your pain is Parkinsons-related, and you have already tried other medications and complementary therapies without relief, it is probably time to try carbidopa/levodopa.
Also Check: Prayers For Parkinsons Disease
Warning Disclaimer Use For Publication
WARNING: Please DO NOT STOP MEDICATIONS without first consulting a physician since doing so could be hazardous to your health.
DISCLAIMER: All material available on eHealthMe.com is for informational purposes only, and is not a substitute for medical advice, diagnosis, or treatment provided by a qualified healthcare provider. All information is observation-only. Our phase IV clinical studies alone cannot establish cause-effect relationship. Different individuals may respond to medication in different ways. Every effort has been made to ensure that all information is accurate, up-to-date, and complete, but no guarantee is made to that effect. The use of the eHealthMe site and its content is at your own risk.
If you use this eHealthMe study on publication, please acknowledge it with a citation: study title, URL, accessed date.
You May Like: Best Bed For Parkinson’s
Not Your Usual Neck And Back Pain
There are many ways to get a backache. This is new for me lower back pain that leads to spasms and literally drives me to my knees.
It doesnt feel like the pain from overdoing it in the garden. Every gardener knows that exquisite twinge from too much lifting or shoveling. After all the years I have gardened, I know that pain well. This is not my usual lower back pain.
An article published in 2018 in the European Spine Journal found significantly more cases of low back pain, with longer durations, in patients with Parkinsons disease than in healthy controls. Parkinsons patients also experience more frequent and intense lumbar pain. Researchers concluded that Parkinsons progression can lead to degeneration of the lumbar spine, and this leads to low back pain for about 88% of this population.
Also Check: Why Is It Important To Take Parkinsons Medication On Time
Akinetic Crisis And Pain
This type of pain may occur in the advanced stages of Parkinsons. Its brought on by akinetic crisis, which is a rare and sometimes dangerous complication of Parkinson’s.
Akinetic crisis involves a worsening of Parkinsons symptoms, which can include severe rigidity, a complete loss of movement, fever and difficulty swallowing. People with Parkinsons who have akinetic crisis pain say that they feel pain in their muscles and joints, and experience headaches. Some people also experience whole-body pain.
This type of pain can be brought on if you abruptly stop taking Parkinsons medication, or if you develop an infection, both of which can cause Parkinson’s symptoms to suddenly get worse. Akinetic crisis requires urgent medical help. If it looks like someone is experiencing akinetic crisis, call 999.
Read Also: My Life With Parkinson’s