Beyond Symptomatic Therapy: Neuroprotection Studies In Pd
Neuroprotective therapies are interventions that produce enduring benefits by favorably influencing the underlying etiology or pathogenesis of neurodegenerative disorders . Although there is currently no definitive methodology to assess neuroprotection in PD patients , multiple attempts have been made to assess the effects of medications on disease progression.
How Is It Treated And Is There A Cure
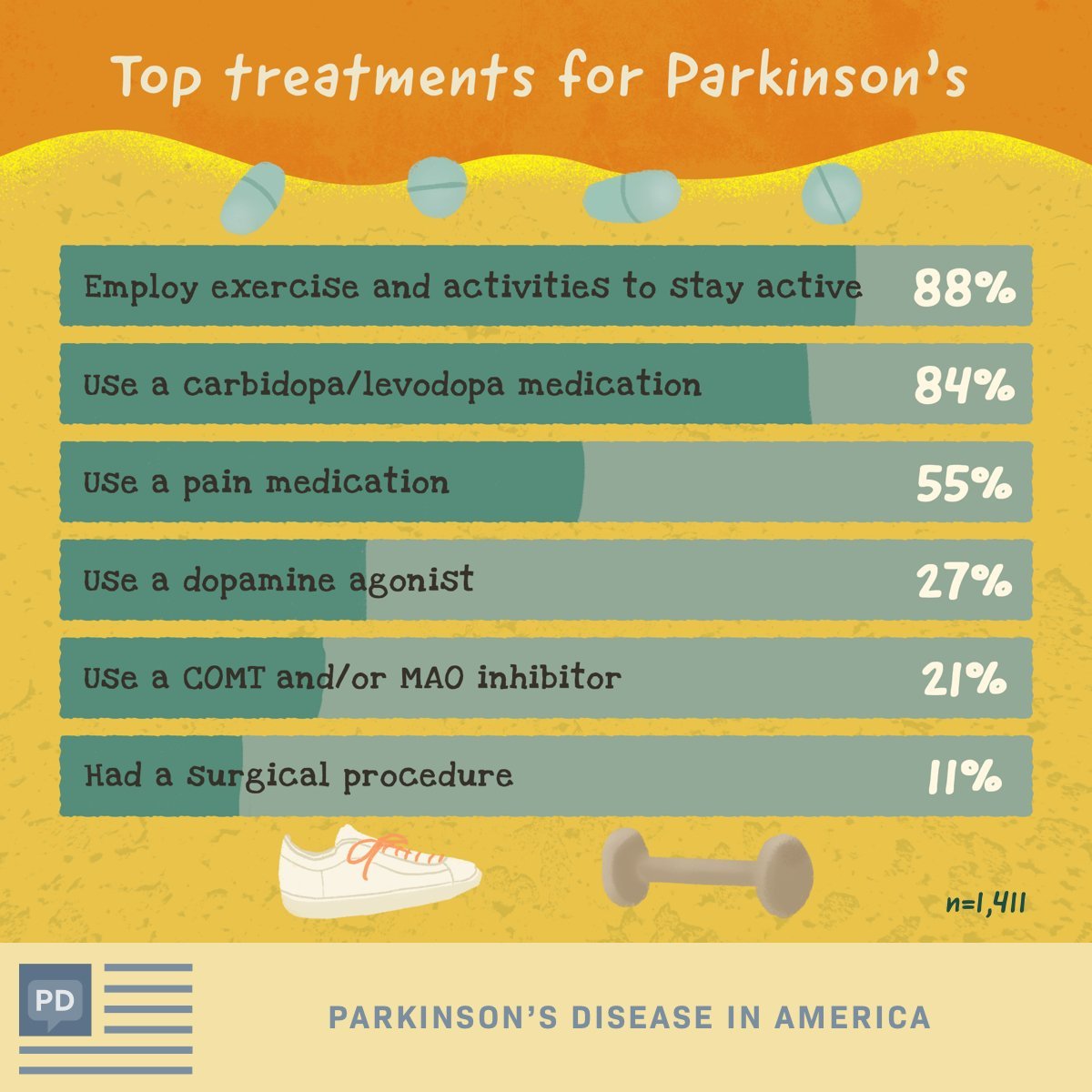
For now, Parkinsons disease is not curable, but there are multiple ways to manage its symptoms. The treatments can also vary from person to person, depending on their specific symptoms and how well certain treatments work. Medications are the primary way to treat this condition.
A secondary treatment option is a surgery to implant a device that will deliver a mild electrical current to part of your brain . There are also some experimental options, such as stem cell-based treatments, but their availability often varies, and many aren’t an option for people with Parkinsons disease.
When Is It Best To Start The Parkinsons Drug Levodopa
This is a plain English summary of an original research article
Earlier treatment with levodopa provides symptomatic relief to those with symptoms but does not appear to slow Parkinsons disease from progressing. Therefore, timing is best determined by symptoms.
The treatment of Parkinsons disease is complex. Levodopa is the main drug used to reduce tremors and muscle stiffness. Whether it modifies the course of the disease or becomes less effective over time is debated, and it can have side effects, so patients and clinicians sometimes prefer to delay starting treatment.
This Dutch trial involved 445 participants with a recent diagnosis of Parkinsons disease, enrolled over five years. About half took levodopa for 80 weeks, and half placebo for the first 40 weeks and levodopa for the last 40 weeks. There was no difference in symptoms between the groups at the end of the study.
This evidence supports current guidance to start levodopa when symptoms begin to affect the quality of life and confirm that it has insufficient impact on disease progression to justify earlier treatment.
Recommended Reading: Celebrities With Parkinson’s Disease
Motor And Nonmotor Symptoms Of Pd
At its core, PD is characterized by four cardinal symptoms: bradykinesia, rigidity, resting tremor, and postural instability.4 Along with these typical motor symptoms come many nonmotor symptoms with significant associated morbidity and mortality. These include autonomic dysfunction, disorders of sleep and wakefulness, cognitive dysfunction and dementia, mood disorders, and psychosis.5 These nonmotor symptoms of PD are responsible for a significant proportion of hospitalizations, with psychosis reportedly accounting for 24% of hospital admissions in patients with PD.6 This fact signifies the importance of properly managing patients with PD psychosis on both an inpatient and an outpatient basis.6
Treatment Of Neurobehavioral Features
Treatment of cognitive deficits associated with PD is as challenging as the treatment of Alzheimers disease and other dementias. While the general assumption has been that cognitive deficits are a feature of late-stage PD, clinically inapparent cognitive changes on neuropsychiatric testing may be found . With the introduction of cholinesterase inhibitors such as donepezil , rivastigmine , and galantamine and the NDMA antagonist memantine , it is possible that cognition, orientation and language function will improve, and that such improvement will lead to a meaningful improvement in function. Both donepezil and rivastigmine improve cognition to the same effect, but donepezil is better tolerated . The largest and best-designed study of rivastigmine in dementia associated with PD involved 541 patients enrolled in a 24-week randomized, multicenter, double-blind clinical trial . The patients had a relatively mild dementia , with onset of dementia about 2 years after onset of PD symptoms. The mean ADAS-cog score, the primary efficacy variable, improved by 2.1 points in the rivastigmine group, compared to 0.7 in the placebo group , and the MMSE improved by 0.8 in the rivastigmine group and worsened by 0.2 in the placebo group . At the end of the study, 55.5% were receiving 9 to 12 mg. The adverse effects that were significantly more frequent in the rivastigmine group were nausea, vomiting, dizziness, and tremor.
Recommended Reading: Fitness Counts Parkinson’s Disease
Why Was This Study Needed
Approximately 127,000 people in the UK have Parkinsons disease, around two people in every 1,000. It mostly affects adults over the age of 50.
Parkinsons disease is a progressive neurological condition that causes increasing disability. People experience, amongst other problems, muscle stiffness, slow movements and tremors.
There is no cure for Parkinsons disease, but treatment can control symptoms. Levodopa is the main drug used to improve movement. It can cause side effects, such as jerky movements, and might become less effective. Therefore, treatment is sometimes delayed to avoid side effects.
Earlier research has suggested that levodopa might slow down the worsening of the disease itself, as well as relieving symptoms. This study aimed to demonstrate whether this was the case and chart the development of any symptoms over almost 18 months.
How Is It Diagnosed
Diagnosing Parkinson’s disease is mostly a clinical process, meaning it relies heavily on a healthcare provider examining your symptoms, asking you questions and reviewing your medical history. Some diagnostic and lab tests are possible, but these are usually needed to rule out other conditions or certain causes. However, most lab tests aren’t necessary unless you don’t respond to treatment for Parkinson’s disease, which can indicate you have another condition.
Recommended Reading: Does Michael J Fox Have Parkinson’s Disease
Stay Safe With Your Medicines
Read all labels carefully.
- Tell all your health care providers about all the medicines and supplements you take.
- Know all the medicines and foods youâre allergic to.
- Review any side effects your medicines can cause. Most reactions will happen when you start taking something, but thatâs not always the case. Some reactions may be delayed or may happen when you add a drug to your treatment. Call your doctor right away about anything unusual.
- Use one pharmacy if possible. Try to fill all your prescriptions at the same location, so the pharmacist can watch for drugs that might interact with each other.
- You can use online tools to see if any of your medicines wonât work well together.
You have the right and responsibility to know what medications your doctor prescribes. The more you know about them and how they work, the easier it will be for you to control your symptoms. You and your doctor can work together to create and change a medication plan. Make sure that you understand and share the same treatment goals. Talk about what you should expect from medications so that you can know if your treatment plan is working.
Show Sources
How Soon After Treatment Will I Feel Better And How Long Will It Take To Recover
The time it takes to recover and see the effects of Parkinson’s disease treatments depends strongly on the type of treatments, the severity of the condition and other factors. Your healthcare provider is the best person to offer more information about what you can expect from treatment. The information they give you can consider any unique factors that might affect what you experience.
Read Also: Does Parkinson’s Disease Cause Death
Parkinsons Treatment For Motor Symptoms
The majority of medications developed specifically to treat Parkinsons disease target common motor symptoms. Many of these treatments are designed to increase the level of the dopamine, a neurotransmitter that transfers signals between nerve cells. Dopamine is involved in regulating signals for movement, which is reduced in the brains of Parkinsons disease patients.
Management Of Later Stages
After the first five years about half the patients develop motor fluctuations or dyskinesias that may be difficult to treat. Commonly the first fluctuations to occur are early morning akinesia and end-of-dose deterioration, also referred to as wearing off. These are predictable periods of immobility or greater severity of other parkinsonian symptoms when the effect of L-dopa wears off. They usually develop gradually over a period of several minutes up to an hour and are related to the timing of antiparkinsonian medication.
To overcome wearing-off, more frequent doses of standard L-dopa are sometimes helpful, for example, five or six instead of three daily doses. Alternatively, changing from a standard L-dopa preparation to a slow release formulation can be tried. The bioavailability of these drugs is usually 70% of that of standard L-dopa. Although they last longer, initial absorption is slower and peak dose concentrations are lower so that patients often need a kick start dose of standard L-dopa first thing in the morning to compensate for that. They may also need occasional top-up doses of L-dopa during the day. Occasionally only very small doses are required. In these situations patients may benefit from dispersible L-dopa to titrate their individual doses.
Box 3: Management of later stages
The duration of off periods may effectively be reduced by subcutaneous administration of apomorphine either as a single rescue dose or as continuous infusion .
Questions
Read Also: Antipsychotics In Parkinson’s Disease
Treating Parkinsons With Complementary Medicine
Complementary medicine incorporates many different practices that can be used alongside conventional medicine to try to ease PD symptoms. There is typically not as much rigorous data to support the use of complementary medicine techniques, as compared to conventional medicine, but many patients find them helpful. These include yoga and massage.
Dementia With Lewy Bodies
Of people with dementia, the type of parkinsonism called dementia with Lewy bodies is the second most common cause of dementia, after Alzheimers disease in the elderly. Many are diagnosed at first with Alzheimers disease due to memory or cognitive disorders and then later as dementia with Lewy bodies as the motor symptoms common to Parkinsons progress.
Lewy bodies are abnormal deposits of protein on the nerve cells in the brain. If the production of dopamine, a neurotransmitter, produced by those nerve cells is disrupted due to the buildup of Lewy bodies on those cells, too little dopamine is produced, which can cause the symptoms of Parkinsons.
Recommended Reading: What Happens If Parkinson’s Is Left Untreated
Initial Drug Treatment In Parkinsons Disease
The bottom line
-
First line treatments for Parkinsons disease include levodopa, non-ergot dopamine agonists, and monoamine oxidase B inhibitors
-
Consider starting levodopa treatment in all patients, especially those with serious motor impairment or cognitive impairment
-
Monitor for motor complications and impulsivity and adjust doses accordingly
-
Do not stop treatment abruptly because this may cause malignant hyperthermia
A 69 year old retired bus driver with no medical history of note presented to the outpatients department with a three year history of progressive tremor of the right hand slowness of movement and difficulty turning in bed at night, buttoning shirts, and using cutlery. He is keen to know what is wrong and whether it can be treated.
Advanced Therapies For Parkinsons Disease
When significant off-time or dyskinesia persists despite optimised oral treatment, advanced therapies should be considered. Apomorphine, a potent dopamine agonist given by continuous subcutaneous infusion, is the least invasive and most straightforward of these. Following on from extensive clinical experience, the recent double-blind TOLEDO study confirmed a significant reduction in off-time and improved on-time with apomorphine versus placebo.
Deep-brain stimulation involves surgical placement of electrodes into brain regions such as the subthalamic nucleus to improve motor fluctuations or refractory tremor. DBS is typically considered in patients without significant axial or neuropsychiatric problems. It improves motor function, off-time and QoL in patients with PD, and provides significant benefits over medical therapy even in patients with an average disease duration of 7 years. The benefits of DBS on motor function, fluctuations and activities of daily living have been demonstrated up to 10 years postoperatively, although axial features continue to progress. Infusion of levodopacarbidopa intestinal gel via jejunostomy has also been shown to improve off-time compared to oral levodopa, and is commissioned in specialist centres where other advanced therapies are ineffective or contraindicated. Further information on the decision-making process for advanced therapies is summarised in a dedicated review.
Dont Miss: Parkinsons Disease And Driving
Don’t Miss: Can Medication Cause Parkinson’s
Aan Releases Recommendations On Treatment Of Parkinsons Disease
Am Fam Physician. 2007 Mar 15 75:922-924.
-
Guideline source: American Academy of Neurology
-
Literature search described? Yes
-
Evidence rating system used? Yes
-
Available at:
Parkinsons disease is the second most common neurodegenerative disease and is characterized by bradykinesia tremor at rest rigidity and abnormalities of balance, posture, and gait. Its etiology remains unknown in most patients. Recommendations from the Quality Standards Subcommittee of the American Academy of Neurology discuss the following aspects of this condition in a collection of articles in the April 2006 issue of Neurology: diagnosis and prognosis neuroprotective strategies and alternative therapies treatment and evaluation and treatment of depression, psychosis, and dementia in patients with Parkinsons disease.
What Did It Find
- According to the UPDRS score, there was no difference in the progress of disease between the early-start group and the delayed-start group , .
- The estimated rate of change in progression of the disease, a secondary outcome, was similar in both groups between 4 and 44 weeks .
- Due to needing symptomatic relief, 87 people in the delayed-start group had levodopa before week 40.
- The estimated rate of change in progression was faster between weeks 44 and 80 in the early-start group . This means starting levodopa earlier did not slow disease progression.
- At 80 weeks, a similar proportion of participants were suffering complications, such as involuntary movements, from levodopa treatment .
Recommended Reading: Medications To Treat Parkinson’s Disease
Parkinsons Disease: Management And Guidance
An overview of Parkinsons disease management, including discussion of the updated National Institute for Health and Care Excellence guidelines.
Nervous system diseases
DR. MICHAEL SOUSSAN/ISM/SCIENCE PHOTO LIBRARY
Parkinsons disease is a chronic, progressive neurodegenerative condition resulting from the loss of the dopamine-containing cells of the substantia nigra, and its prevalence increases with age. Using primary care data from 2015, a Parkinsons UK report of the Clinical Practice Research Datalink found that the prevalence of PD is 45 per 100,000 people who are aged 3039 years, compared with 1,696 per 100,000 people who are aged 8084 years. Prevalence rates almost double at each five-year interval between the ages of 50 and 69 years for both men and women. The lifetime risk of being diagnosed with PD is 2.7% equating to 1 in every 37 people being diagnosed at some point in their lifetime. Owing to population growth and an increasing ageing population, the estimated prevalence of PD is expected to increase by 23.2% by 2025.
Thanks For Signing Up
We are proud to have you as a part of our community. To ensure you receive the latest Parkinsons news, research updates and more, please check your email for a message from us. If you do not see our email, it may be in your spam folder. Just mark as not spam and you should receive our emails as expected.
Also Check: What New In Parkinson Treatment
What Does Current Guidance Say On This Issue
The NICE guideline recommends levodopa as a first-line treatment in the early stages of Parkinsons to control problems with movement if symptoms are affecting the quality of life. It does not discuss delayed treatment with levodopa.
If motor symptoms are not affecting the quality of life, the guideline recommends considering other drugs such as dopamine or monoamine oxidase inhibitors based on individual circumstances and preferences.
Anosmia And Other Sensory Manifestations Of Pd

Loss of smell has long been reported to be an early sign of PD, present in 70100% of PD patients . As the loss of smell frequently can precede the onset of motor symptoms, recent research has focused on the role of smell-testing in the early identification of PD . If proven to be sensitive and specific, a smell test would be an easy-to-administer inexpensive screening tool that would be useful for identifying populations at risk of PD and for enrollment in neuroprotection clinical trials. Anosmia does not improve with dopaminergic therapy, and thus cannot be used as a measure of efficacy for dopaminergic agents.
Pain is another common manifestation of PD . The pattern and distribution of pain varies, but a subset of patients experiencing pain is responsive to dopaminergic therapy . The nature of pain in PD is likely multifactorial, and more data on the mechanisms of pain and potential disease-specific treatment interventions are necessary.
Also Check: Parkinson’s Disease Typically Causes
How Do I Take Care Of Myself
If you have Parkinsons disease, the best thing you can do is follow the guidance of your healthcare provider on how to take care of yourself.
- Take your medication as prescribed. Taking your medications can make a huge difference in the symptoms of Parkinson’s disease. You should take your medications as prescribed and talk to your provider if you notice side effects or start to feel like your medications aren’t as effective.
- See your provider as recommended. Your healthcare provider will set up a schedule for you to see them. These visits are especially important to help with managing your conditions and finding the right medications and dosages.
- Dont ignore or avoid symptoms. Parkinsons disease can cause a wide range of symptoms, many of which are treatable by treating the condition or the symptoms themselves. Treatment can make a major difference in keeping symptoms from having worse effects.
Treatment Of Late Stage Complications Of Parkinsons Disease
Postural hypotension
Levodopa and dopamine agonists worsen postural hypotension and it may be necessary to lower the dose of levodopa or withdraw the agonist. Treatment is difficult, but patients should be advised to sleep with the head of the bed raised by one or two bricks and to add salt to their diet. Fludrocortisone can then be added at a dose of 0.1 mg in the morning, increasing if necessary up to 0.5 mg in the morning. If these measures are ineffective, the alpha agonist midodrine 10-20 mg four hourly can be useful but it is experimental and only available via the Special Access Scheme. Patients treated for postural hypotension need to have electrolytes, renal function and supine blood pressures closely monitored.
Parkinsonian psychosis, depression and dementia
Psychotic symptoms such as visual hallucinations and persecutory delusions occur most commonly in the setting of dementia, which may be mild and therefore easily missed. Most drugs for Parkinsons disease make these symptoms worse. Depression is also common and requires treatment in its own right.
Read Also: What Causes Parkinson’s Syndrome