Anatomical Connections Between The Basal Ganglia And Cerebellum
The cerebellum and basal ganglia are two major subcortical structures that influence multiple aspects of motor, cognitive and affective behaviour . Both structures form multi-synaptic loops with the cerebral cortex the cerebellum is known to influence motor and cognitive operations through the cerebello-thalamo-cortical circuit . The cerebellum and basal ganglia have distinct loops connecting with largely overlapping cortical areas . Thus, basal ganglia and cerebellar loops were long assumed to be entirely separate anatomically and to perform distinct functional operations. Interactions between these two regions were traditionally thought to occur at the level of the cerebral cortex . However, recent studies elucidated that there are anatomical connections between the cerebellum and basal ganglia.
demonstrated the existence of a disynaptic connection between the cerebellum and striatum in rats. Later, using transneuronal transport of rabies virus in monkeys, showed that one of the output nuclei of the cerebellum, the dentate nucleus, projects to the striatum via a disynaptic connection, and to the external globus pallidus via a trisynaptic connection. The disynaptic projection to the striatum originates from both the motor and non-motor domains of the dentate. These findings demonstrate that the cerebellum has a strong disynaptic projection to the striatum by way of the thalamus, and may influence the pathways involved in basal ganglia processing.
Beyond Dopamine Does Pd Effect Other Neurotransmitters
Trends in PD research are showing that in addition to Parkinsons impact on the neurotransmitter dopamine and the dopamingeric system, the neurotransmitter acetylcholine and the brains cholingeric system are also impacted.
This post reviews recent research , and discusses how two vitamins/supplements may impact Parkinsons disease. This should not be considered medical advice. Always consult your doctors and pharmacist about any vitamins or supplements that you are taking or considering.
Related:
Exhibit A: Yale Study challenges assumptions about PD and acetylcholine
Several weeks ago, a Yale study challenged a long held assumption about Parkinsons effect on a neurotransmitter other than dopamine. The loss of dopamine leads to slower movements, resting tremors, and other symptoms that worsen over time. To help these symptoms, doctors prescribe treatments that increase dopamine levels in the striatum, a portion of the brain that is responsible for motor learning. However, medical treatments do not consider the effects of Parkinsons on another neurotransmitter, acetylcholine.
The Yale research argues that dopamine deficiency reduces acetylcholine, and suggests that treating Parkinsons may require targeted therapies that restore the balance between these two chemicals, instead of focusing solely on dopamine, said the researchers.
More on this Yale study:
Exhibit B: Mayo research commentary on Vitamin B-12
Exhibit E : CDP Choline and PD Study from 1990
What Are The Symptoms
Symptoms of PD vary from person to person, as does the rate of progression. A person who has Parkinson’s may experience some of these more common “hallmark” symptoms:
- Bradykinesia – slowness of movement, impaired dexterity, decreased blinking, drooling, expressionless face.
- Tremor at rest – involuntary shaking that decreases with purposeful movement. Typically starts on one side of the body, usually the hand.
- Rigidity – stiffness caused by involuntary increase in muscle tone.
- Postural instability – sense of imbalance. Patients often compensate by lowering their center of gravity, which results in a stooped posture.
Other symptoms that may or may not occur:
Freezing or being stuck in place Shuffling gait or dragging of one foot Stooped posture Cognitive impairment
Also Check: Sam Waterston Parkinson’s
Is Parkinson’s Diagnosed In The Brain
Parkinson’s disease is one of the most challenging neurological disorders to diagnose and treat. If your doctor suspects you have Parkinson’s disease, you will usually be referred to a neurologist for further tests. These tests will involve certain movements and exercises to check your symptoms.
A neurologist will look for motor symptoms such as:
- A tremor that occurs at rest
- Slowed movement
- Muscle stiffness
If you have two or more of these symptoms and your doctor has taken blood tests to rule out other causes, it’s likely you will be diagnosed with Parkinson’s disease. Your symptoms will be closely monitored to see any progression of Parkinson’s disease, which can take years.
What Causes Parkinsons Disease
We do not know what causes Parkinsons disease. There is some evidence to suggest that there is a genetic factor which increases the risk of Parkinsons disease within some families. Also, there might be an increased risk if people have come into contact with a particular toxin or toxins found in the environment via pesticides and other chemicals used in agriculture. The specific toxin or toxins have not yet been identified but there is ongoing research into this possible cause.
Don’t Miss: Parkinson’s Double Vision
Is There A Cure For Parkinsons
Theres currently no cure for Parkinsons, a disease that is chronic and worsens over time. More than 50,000 new cases are reported in the United States each year. But there may be even more, since Parkinsons is often misdiagnosed.
Its reported that Parkinsons complications was the
Complications from Parkinsons can greatly reduce quality of life and prognosis. For example, individuals with Parkinsons can experience dangerous falls, as well as blood clots in the lungs and legs. These complications can be fatal.
Proper treatment improves your prognosis, and it increases life expectancy.
It may not be possible to slow the progression of Parkinsons, but you can work to overcome the obstacles and complications to have a better quality of life for as long as possible.
Parkinsons disease is not fatal. However, Parkinsons-related complications can shorten the lifespan of people diagnosed with the disease.
Having Parkinsons increases a persons risk for potentially life threatening complications, like experiencing:
- falls
Parkinsons often causes problems with daily activities. But very simple exercises and stretches may help you move around and walk more safely.
How Is A Diagnosis Made
Because other conditions and medications mimic the symptoms of PD, getting an accurate diagnosis from a physician is important. No single test can confirm a diagnosis of PD, because the symptoms vary from person to person. A thorough history and physical exam should be enough for a diagnosis to be made. Other conditions that have Parkinsons-like symptoms include Parkinsons plus, essential tremor, progressive supranuclear palsy, multi-system atrophy, dystonia, and normal pressure hydrocephalus.
Recommended Reading: Adaptive Silverware For Parkinson’s
From Theory To Computational Models Of The Bgctxcer System Imparements In Pd
The brain system proposed in as the corticalsubcortical network producing PD symptoms has a clear, distinct feature: it involves highly recurrent circuits. In this article, we aimed to link PD symptoms to specific impairments of the network, but this exercise has an inherently limited scope: it can only partially disentangle the circular causations involved by the above-discussed circuits, and on this basis offer quantitative predictions. For example, we proposed specific hypotheses to explain tremor and freezing, but it is not possible to establish if such hypotheses are self-consistent and sound only on a verbal basis. Computational models have the power to prove the self-consistency of hypothesis as those proposed here.,,,,, This is a necessary condition to establish the validity of theories . For this reason, we consider here possible approaches to follow to translate the verbal theories presented here into operational computational models able to offer sound explanations and quantitative predictions on PD symptoms.
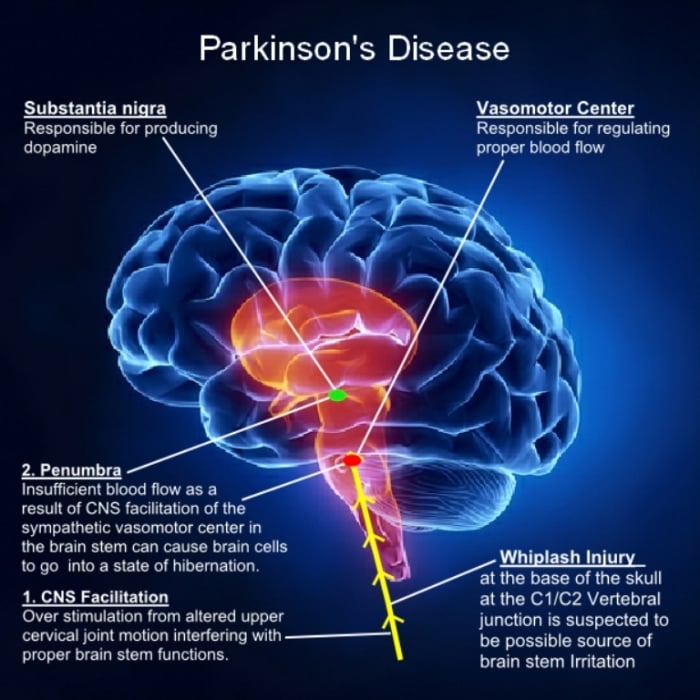
Changes Inside The Brain
In Parkinson disease, nerve cells in part of the basal ganglia degenerate.
The basal ganglia are collections of nerve cells located deep within the brain. They help do the following:
-
Initiate and smooth out intended muscle movements
-
Suppress involuntary movements
-
Coordinate changes in posture
When the brain initiates an impulse to move a muscle , the impulse passes through the basal ganglia. Like all nerve cells, those in the basal ganglia release chemical messengers that trigger the next nerve cell in the pathway to send an impulse. A key neurotransmitter in the basal ganglia is dopamine. Its overall effect is to increase nerve impulses to muscles.
When nerve cells in the basal ganglia degenerate, they produce less dopamine, and the number of connections between nerve cells in the basal ganglia decreases. As a result, the basal ganglia cannot control muscle movement as they normally do, leading to tremor, slow movement , a tendency to move less , problems with posture and walking, and some loss of coordination.
Also Check: Similar To Parkinsons
What Causes Parkinson’s Disease
Parkinsons disease occurs when nerve cells in the basal ganglia, an area of the brain that controls movement, become impaired and/or die. Normally, these nerve cells, or neurons, produce an important brain chemical known as dopamine. When the neurons die or become impaired, they produce less dopamine, which causes the movement problems of Parkinson’s. Scientists still do not know what causes cells that produce dopamine to die.
People with Parkinson’s also lose the nerve endings that produce norepinephrine, the main chemical messenger of the sympathetic nervous system, which controls many functions of the body, such as heart rate and blood pressure. The loss of norepinephrine might help explain some of the non-movement features of Parkinson’s, such as fatigue, irregular blood pressure, decreased movement of food through the digestive tract, and sudden drop in blood pressure when a person stands up from a sitting or lying-down position.
Many brain cells of people with Parkinson’s contain Lewy bodies, unusual clumps of the protein alpha-synuclein. Scientists are trying to better understand the normal and abnormal functions of alpha-synuclein and its relationship to genetic mutations that impact Parkinsons disease and Lewy body dementia.
How Will My Doctor Test For It
There’s no one test for Parkinson’s. A lot of it’s based on your symptoms and health history, but it could take some time to figure it out. Part of the process is ruling out other conditions that look like Parkinson’s. The docotor may do a DaT scan, which looks for dopamine in the brain. This can aid in a diagnosis.
Because there is no single test, it’s very important to go to a doctor who knows a lot about it, early on. It’s easy to miss.
If you do have it, your doctor might use what’s called the Hoehn and Yahr scale to tell you what stage of the disease you’re in. It ranks how severe your symptoms are from 1 to 5, where 5 is the most serious.
The stage can help you get a better feel for where your symptoms fall and what to expect as the disease gets worse. But keep in mind, some people could take up to 20 years to move from mild to more serious symptoms. For others, the change is much faster.
Also Check: Diseases Similar To Parkinsons
Structural And Functional Brain Patterns Of Non
- Department of Neurology, Jena University Hospital, Jena, Germany
Parkinsons disease is a common, progressive and multisystem neurodegenerative disorder characterized by motor and non-motor symptoms. Advanced magnetic resonance imaging, positron emission tomography, and functional magnetic resonance imaging can render the view toward understanding the neural basis of these non-motor syndromes, as they help to understand the underlying pathophysiological abnormalities. This review provides an up-to-date description of structural and functional brain alterations in patients with PD with cognitive deficits, visual hallucinations, fatigue, impulsive behavior disorders, sleep disorders, and pain.
Ways To Decrease The Risk Of Parkinsons And Alzheimers
There is currently no cure for either disease. Parkinsons is considered a more treatable condition, however, especially in the early stages of the disease. Treatments include medication, physical therapy, and lifestyle modifications such as dietary changes. Research continues to suggest that a brain-healthy lifestyle can help prevent both Alzheimers and Parkinson’s. Here are some basic guidelines:
You May Like: Sam Waterston Tremor
What Are The Treatments For Parkinson’s Disease
There is no cure for PD, and no treatment prevents the disease from progressing. However, treatments can usually ease symptoms.
- At first, you may not need any treatment when the symptoms are mild. A specialist may simply see you every now and then to monitor how the disease is progressing.
- A medicine that eases symptoms is usually started when symptoms become troublesome.
- Therapies such as physiotherapy, occupational therapy and speech therapy may also be useful as the disease progresses.
- Surgery may be an option for severe cases.
What Medications Are Used To Treat Parkinsons Disease
Medications are the main treatment method for patients with Parkinsons disease. Your doctor will work closely with you to develop a treatment plan best suited for you based on the severity of your disease at the time of diagnosis, side effects of the drug class and success or failure of symptom control of the medications you try.
Medications combat Parkinsons disease by:
- Helping nerve cells in the brain make dopamine.
- Mimicking the effects of dopamine in the brain.
- Blocking an enzyme that breaks down dopamine in the brain.
- Reducing some specific symptoms of Parkinsons disease.
Levodopa: Levodopa is a main treatment for the slowness of movement, tremor, and stiffness symptoms of Parkinsons disease. Nerve cells use levodopa to make dopamine, which replenishes the low amount found in the brain of persons with Parkinsons disease. Levodopa is usually taken with carbidopa to allow more levodopa to reach the brain and to prevent or reduce the nausea and vomiting, low blood pressure and other side effects of levodopa. Sinemet® is available in an immediate release formula and a long-acting, controlled release formula. Rytary® is a newer version of levodopa/carbidopa that is a longer-acting capsule. The newest addition is Inbrija®, which is inhaled levodopa. It is used by people already taking regular carbidopa/levodopa for when they have off episodes .
Also Check: Prayer For Parkinson’s Disease
How Parkinsons Disease Affects The Body
Life with Parkinsons is challenging, to say the least. This progressive disease starts slowly, and because theres currently no cure, it gradually worsens how you think and feel.
Giving up may seem like the only solution, but it certainly isnt. Thanks to advanced treatments, many people are able to continue living healthy, productive lives with Parkinsons.
Take a glance at this infographic to get a visual picture of how Parkinsons can affect everything from your memory to your movement.
Freezing As Response Conflict Impairment: Corticalsubcortical Substrates
Freezing is the inability to begin or continue a voluntary discrete or rhythmic movement. It can affect walking, writing, speech, and is also associated with deficits in a number of executive functions including attention and conflict resolution. The vast range of conditions provoking or relieving freezing supports the involvement of a complex brain network including both cortical and subcortical areas.,
Pivoting on the anatomical connections between BG and Ctx, and between BG and Cer,,, and on recent data about the involvement of pre-SMA,,, and Cer,, in freezing, we propose here some system-level hypotheses on the possible alterations of corticalsubcortical circuits that might underlie freezing . Striatum modulates the output nuclei of BG through two pathways. The first is the direct pathway that involves a Str GABAergic connection directly inhibiting GPi and substantia nigra pars reticulata . The second is the indirect pathway involving two sub-routes: the short indirect pathway, linking the external globus pallidus to GPi/SNr via GABAergic connections and the long indirect pathway linking GPe to STN which in turn projects to GPi/SNr.
Also Check: Parkinson’s Hallucinations Commercial
Diagnosis Of Parkinsons Disease
A number of disorders can cause symptoms similar to those of Parkinson’s disease. People with Parkinson’s-like symptoms that result from other causes are sometimes said to have parkinsonism. While these disorders initially may be misdiagnosed as Parkinson’s, certain medical tests, as well as response to drug treatment, may help to distinguish them from Parkinson’s. Since many other diseases have similar features but require different treatments, it is important to make an exact diagnosis as soon as possible.
There are currently no blood or laboratory tests to diagnose nongenetic cases of Parkinson’s disease. Diagnosis is based on a person’s medical history and a neurological examination. Improvement after initiating medication is another important hallmark of Parkinson’s disease.
The Parkinson’s Disease Brain: What We Know
Parkinson’s disease is a degenerative disorder of the nervous system, which most scientists agree originates in the brain. We know that Parkinson’s disease causes damage to the nerves in the brain, which in turn reduces dopamine cells, but did you also know that this leads to an accumulation of alpha-synuclein, known more commonly as Lewy bodies? This damage is thought to be what causes the motor symptoms of Parkinson’s disease, though scientists still have many questions as to how this works.
Recommended Reading: Pfnca Wellness Programs
What Part Of The Brain Is Affected By Parkinson Disease
Parkinson disease is predominantly a disorder of the basal ganglia, which are a group of nuclei situated at the base of the forebrain. The striatum, composed of the caudate and putamen, is the largest nuclear complex of the basal ganglia. The striatum receives excitatory input from several areas of the cerebral cortex, as well as inhibitory and excitatory input from the dopaminergic cells of the substantia nigra pars compacta . These cortical and nigral inputs are received by the spiny projection neurons, which are of 2 types: those that project directly to the internal segment of the globus pallidus , the major output site of the basal ganglia and those that project to the external segment of the globus pallidus , establishing an indirect pathway to the GPi via the subthalamic nucleus .
For an illustration of the subthalamic nucleus, see the image below.
References
Hauser RA, Grosset DG. FP-CIT SPECT Brain Imaging in Patients with Suspected Parkinsonian Syndromes. J Neuroimaging. 2011 Mar 16. .
Wirdefeldt K, Adami HO, Cole P, Trichopoulos D, Mandel J. Epidemiology and etiology of Parkinson’s disease: a review of the evidence. Eur J Epidemiol. 2011 Jun. 26 Suppl 1:S1-58. .
Anderson P. More Evidence Links Pesticides, Solvents, With Parkinson’s. Medscape Medical News. Available at . Accessed: June 11, 2013.
Grimes DA, Lang AE. Treatment of early Parkinsons disease. Can J Neurol Sci. 1999 Aug. 26 Suppl 2:S39-44. .