Patients In Whom A Diagnosis Of Parkinson’s Disease Was Or Was Not Previously Made
Patients in whom a diagnosis of Parkinson’s disease was previously made had a longer disease duration and greater disease severity , with more severe akinesia , postural instability, and rigidity than those in whom the diagnosis was not made before. They were also more likely to be depressed , to have experienced dyskinesias , and to live alone or with their family than in a nursing home .
What Is Currently Being Done
To better understand and constantly update the criteria, an internet platform, free to the scientific community, is currently being designed which will updated LRs, provide a calculator that can be used to calculate probability for individual patients, and a forum for scientific exchange among experts to further refine the criteria.
Moreover, the ongoing extensive research of epidemiologists, basic scientists, clinicians and neuroimaging specialists will lead to the detection of new risk factors and biomarkers and will substantiate, expand and deepen our understanding of the very early phases of PD. Combined approaches that test multiple modalities in the same patient are especially promising. These include multimodal imaging as well as multimodal biomarker platforms, incorporating combinations of biomarkers from different sources.
Now, big data analyses of huge data sets have also entered PD research. Especially the fields of genetics , -omics approaches and the continuous capturing of movements in daily life by various wearables and devices, including smartphones (e.g., . These will benefit from new methods of data handling and analyses.
Importantly, it needs to be appreciated that merging of large sets of data has become possible not only due to secure web applications but and primarily due to a scientific spirit of cooperation and data sharing.
From Prodromal To Overt Parkinsons Disease: Towards A New Definition In The Year 2040
Issue title: The Times They Are a-Changin: Parkinsons Disease 20 Years from Now
Guest editors: Patrik Brundin, J. William Langston and Bastiaan R. Bloem
Article type: Review Article
Authors: Berg, Danielaa b * | Postuma, Ronald B.c *
Affiliations: Department of Neurology, Christian-Albrechts-University of Kiel, Kiel, Germany | Department of Neurodegeneration, Hertie-Institute for Clinical Brain Research Tuebingen, Germany | Department of Neurology, Montreal General Hospital, Montreal, Quebec, Canada
Correspondence: Correspondence to: Daniela Berg, MD, Department of Neurology, Christian-Albrechts-University of Kiel, Arnold-Heller-Str. 3 24105 Kiel, Germany. E-mail: . and Ronald B. Postuma, MD, MSc, Department of Neurology, L7-305 Montreal General Hospital, 1650 Cedar Ave, Montreal, Canada H3G1A4. E-mail: .
Keywords: Prodromal Parkinsons disease, higher-specificity markers, big data approaches, progression markers, subtypes, population-based screening, neuroprotective trials, gene-specific therapy, individual mechanism-specific therapy
DOI: 10.3233/JPD-181457
Journal: Journal of Parkinson’s Disease, vol. 8, no. s1, pp. S19-S23, 2018
Abstract
Don’t Miss: Fatigue Management And Parkinson’s Disease
New Diagnostics For Pd Might Allow Early Diagnosis Prevention
A new way of diagnosing Parkinsons disease based on manifestations that appear decades before motor symptoms the current hallmarks for diagnosis might allow early diagnosis and even prevention.
The study, From Prodromal to Overt Parkinsons Disease: Towards a New Definition in the Year 2040, was published in the Journal of Parkinsons Disease.
Parkinsons disease is characterized by progressive loss of coordination and movement. Currently, a person is diagnosed when those symptoms appear. However, there are some risk factors and symptoms that precede motor manifestations and constitute the early stages of the disease .
Brilliant work of many in different scientific fields has paved the way for the concept of prodromal that is, a phase of years to decades in which non-motor and subtle motor symptoms may indicate spreading PD pathology, but do not meet the threshold for diagnosis according to the classic motor-based clinical criteria, researchers said.
The development of new diagnostic criteria that allow the identification of prodromal Parkinsons might help to better understand disease progression, lead to early diagnosis and treatment, and prevent classic motor symptoms.
Limitations And Shortcomings Of The Current Understanding And Model
The prodromal PD criteria are meant to be research criteria, and constitute a first step in what should be a continually-updated process.
Several shortcomings have been noted, both at the time of publication and as several groups have studied the criteria. These include:
This is even more significant as the current prodromal criteria are primarily based on clinical signs with no opportunity to include brain autopsy as ultimate diagnostic confirmation.
Also Check: Donate To Parkinson’s Research
Diagnostic Criteria For Parkinsons Disease: From James Parkinson To The Concept Of Prodromal Disease
- 1Department of Neurology and Psychiatry, Sapienza University of Rome, Rome, Italy
- 2Gardner Family Center for Parkinsons Disease and Movement Disorders, Department of Neurology, University of Cincinnati, Cincinnati, OH, United States
- 3IRCCS Institute of Neurological Sciences of Bologna, Bellaria Hospital, Bologna, Italy
- 4Department of Biomedical and Neuromotor Sciences, University of Bologna, Bologna, Italy
- 5Department of Neurology, Santa Maria University Hospital, Terni, Italy
Want To Learn More About The Latest Research In Parkinsons Disease Ask Your Questions In Our Research Forum
Now, Parkinsons experts Daniela Berg, MD, Christian-Albrechts-University of Kiel, Germany, and Ronald B. Postuma, MD, MSc, Montreal General Hospital, Canada, have developed a mathematical model that calculates a persons risk of being in the prodromal phase of the disease. This model is based on three main premises relative to Parkinsons prodromal phase:
-
The fact that the neurodegenerative process in Parkinsons is slow and continuous, possibly starting in the gut or olfactory system, finally reaching the nervous system
-
The increased knowledge regarding risk factors and clinical symptoms that occur years or decades prior to motor manifestations. These can be correlated to imaging findings and tissue examinations
- Studies have found that people who manifest different combinations of risk and prodromal markers can many times progress to Parkinsons disease.
Currently, however, the model has some limitations. For example, it does not consider age and sex factors, and cannot predict whether or when motor symptoms will appear.
The prodromal PD criteria are meant to be research criteria and constitute a first step in what should be a continually updated process, researchers stated.
Wearable technology, such as mobile phones, also allows the continuous capture of movement in daily life, which will benefit from new methods of data handling and analyses, researchers said.
Read Also: Does Parkinson’s Cause Joint Pain
Challenges For The Intermediate Future
PD is currently still defined by its characteristic motor symptoms and we do not know, whether the underlying neurodegeneration starting outside the brain will inevitably progress to the brain in all individuals, neither do we know the individual pace of progression. The questions are: When is the starting point of PD? What will define the disease will it still be motor symptoms , or will it be biomarker evidence of nigrostriatal system neurodegeneration without motor symptoms? Will it be a certain combination of non-motor signs? Or will it be based upon non-clinical biomarkers, similar to changes in Alzheimers disease?
Given the fact that some individuals with Parkinsons disease suffer more from non-motor symptoms than motor ones in the early stages, our aim will need to focus not only on stopping motor progression but also those manifestations outside the substantia nigra.
Understanding prodromal PD will mean understanding PD in all its heterogeneity. Therefore subtypes need to be considered and accounted for in the predictive models.
Finally, progress needs to continue on mitigating all the limitations noted above.
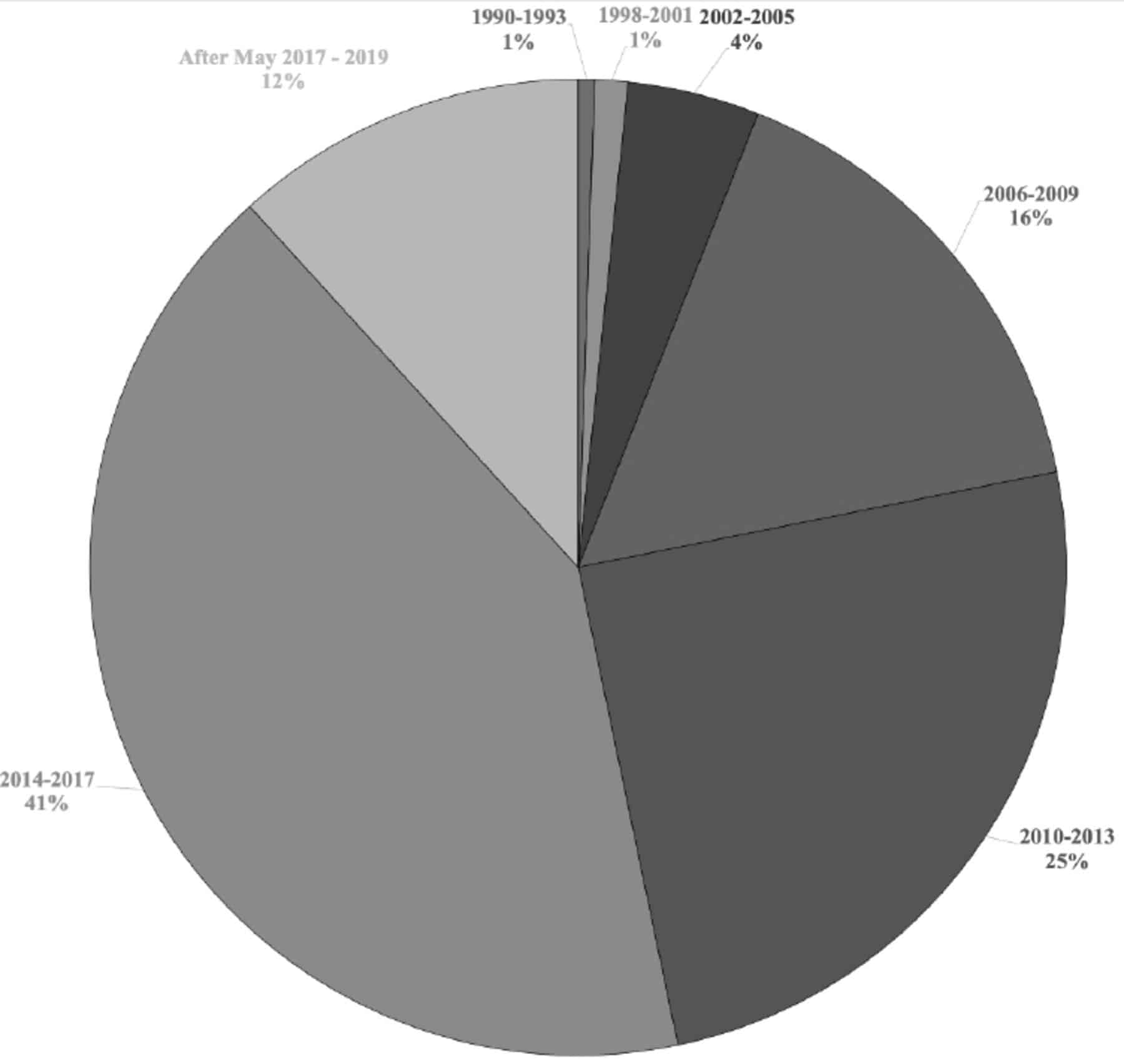
Predictive Values For Clinical Diagnoses Under Different Scenarios
demonstrates how the positive and negative predictive values for each of the main three diagnoses vary as the prevalence of the specific diagnosis alters. The most dramatic effect is seen for IPD, which had a negative predictive value of 90% in the UKPDSBRC sample. When applied to a normal population sample, where IPD is a priori likely to be the most likely diagnosis, this propensity to overdiagnose less common causes of parkinsonism amongst pathologically proven IPD has an important detrimental effect on the negative predictive value. In absolute terms, however, this would still only result in 81 falsenegative diagnoses in every 1000 cases. The relatively good positive predictive values for both MSA and PSP are markedly attenuated in the community sample, where these disorders are far less common. The clinical predictive value in Table , scenario 3, designed to reflect a specialist movement disorder clinic, is much more like that observed from the UKPDSBRC sample.
You May Like: What Medications Can Cause Parkinson’s
Utility Of The New Movement Disorder Society Clinical Diagnostic Criteria For Parkinson’s Disease Applied Retrospectively In A Large Cohort Study Of Recent Onset Cases
The MDS diagnostic criteria for Parkinson’s Disease were tested retrospectively in a large cohort study.
-
Over 90% of cases diagnosed clinically as PD fulfilled MDS diagnostic criteria for PD.
-
Over 60% were categorized Clinically established PD under 30% were Clinically probable PD.
-
Cases categorized as not PD had more severe, less therapy responsive parkinsonism.
-
Categorization as PD by the MDS criteria was 85% stable after 2.5 years of follow-up.
Patients With A Previous Diagnosis Other Than Parkinson’s Disease
Among all patients seen, two were referred for diagnostic purposes without a previous diagnosis, and 69 of 202 patients had a previous diagnosis other than Parkinson’s disease . Among these, 56 patients had been given a diagnosis of non-parkinsonian tremor, two of vascular parkinsonism, one of atypical parkinsonism, and 10 had been prescribed an antiparkinsonian drug for parkinsonian features without a specific diagnosis . Thirteen of the 69 patients with different diagnoses and the two patients referred for diagnostic purposes fulfilled strict clinical criteria for Parkinson’s disease . In two additional patients who had a previous diagnosis of non-parkinsonian tremor, a diagnosis of possible Parkinson’s disease was made . If only patients who had at some point in the past seen a specialist were considered, the diagnosis was changed to probable Parkinson’s disease in five and to possible Parkinson’s disease in one .
Sensitivity, specificity, and predictive values for the overall sample* and by type of clinician
Recommended Reading: Michael J Fox On Parkinsons
What Is A Datscan And What Role Does It Play In A Parkinsons Diagnosis
In 2011, the FDA approved the use of a scan called a dopamine transporter scan . A DaTscan is an imaging technology that allows visualization of the dopamine system in the brain. It is similar to an MRI, but looks at the function of the brain rather than the structure.
A DaTscan involves injection of a small amount of a radioactive drug that is then measured by a single-photon emission computed tomography scanner . The SPECT scanner measures the levels and location of the drug in the brain.
It is important to know that a negative DaTscan does not rule out PD, especially early in the disease, but a positive DaTscan can help confirm it. A positive DaTscan can differentiate PD from essential tremor as there is no dopamine deficiency in the latter. However, DaTscan abnormalities can be seen in PD as well as other forms of atypical parkinsonism that cause a loss of dopamine . This means that a positive result does not differentiate Parkinsons disease from other forms of atypical parkinsonism.
Rationale And Construct Of The Mds
In this view, in 2015 the ad hoc MDS task force proposed new clinical diagnostic criteria for PD . These criteria were specifically designed for use in research, but they also might be adopted as a general guide to the clinical diagnosis of PD in a routine setting . Examination of all cardinal manifestations should be carried out as described in the MDS-Unified Parkinson Disease Rating Scale . In the MDS-PD criteria, the classical signs of the motor syndrome remain the core features of the disease. The essential criterion is the presence of parkinsonism, which is defined as bradykinesia, in combination with at least one between rest tremor and rigidity . However, many non-motor manifestations, often dominating the clinical presentation of the disease, have now been incorporated into the diagnostic criteria . Based on the assumption that the pathological process of PD may begin in non-dopaminergic structures of the brain or peripheral nervous system, a new diagnostic category has been configured, prodromal PD : prodromal PD is considered to represent a true initial stage of PD .
Table 1. Supportive criteria, absolute exclusion criteria, and red flags for the diagnosis of Parkinsons disease, according to the revised International Parkinson and Movement Disorder Society diagnostic criteria .
Table 2 provides a brief synopsis reporting the main features of the different diagnostic criteria and guidelines developed to improve the diagnosis of PD.
Recommended Reading: How Does Parkinson’s Disease Affect The Body
The View From : A Future Without Clinical Pd
As we better understand the prodromal phase and increase diagnostic certainty, we will inevitably begin to understand that our current concept of prodromal PD is, in fact, PD. In 2040 we also will have gained understanding of progression in the prodromal phase, and the differing prodromal evolution of subtypes of PD. As subtype-specific biomarkers are understood, diagnostic accuracy will continue to improve.
The primary goal of all prodromal research is help slow or stop disease in its early stages, and prevent clinical disease onset. Ultimately, one would hope to prevent initiation of the neurodegenerative process at all.
For our research to bear fruit, we also require a better understanding of causative mechanisms, to enable the discovery of true disease modifying and finally neuroprotective treatments.
If early disease is detected, a course of treatment is started. This will again be personalized, based on the genetic pathways contributing to the neurodegenerative process identified, perhaps including changes in lifestyle , gene-specific therapy, individual mechanism-specific therapy , periodic protein-based clearing , or a well-tolerated small molecule protein inhibitor given lifelong.
The New Definition And Diagnostic Criteria Of Parkinson’s Disease
@article, author=nther Deuschl and Thomas Gasser and Christopher G. Goetz and Glenda M. Halliday and Lawrence Joseph and Anthony E. Lang and Inga Liepelt-Scarfone and Irene Litvan and Kenneth Marek and Wolfgang Hermann Oertel and C. Warren Olanow and Werner Poewe and Matthew B. Stern}, journal=, year=, volume=, pages=}
- View 2 excerpts, cites methods and background
- Movement disorders : official journal of the Movement Disorder Society
- View 1 excerpt, cites background
- View 2 excerpts, cites background
- View 1 excerpt, cites background
- View 1 excerpt, cites background
- View 1 excerpt, cites background
- Movement disorders : official journal of the Movement Disorder Society
You May Like: Prevalence Of Parkinson’s Disease In The Us
Tests To Rule Out Other Conditions
Blood tests can help rule out other possible causes of the symptoms, such as abnormal thyroid hormone levels or liver damage.
An MRI or CT scan can check for signs of a stroke or brain tumor, which may cause similar symptoms.
Hydrocephalus due to atrophy can occur with some types of dementia and would be visible with one of these imaging tests. If the person has neurologic symptoms but a normal scan result, Parkinsons disease may be present.
The doctor a lumbar puncture to rule out inflammation or a brain infection.
Expected Findings: The Near Future
Use of the anticipated internet platform for prodromal PD will accelerate learning and application of the criteria in a growing community of scientists expanding its use not only to cohorts with the endpoint of PD/neurodegeneration but also to different primary endpoints in which additional markers may be identified. This should help facilitate detection and dissemination of currently unknown risk and prodromal markers for PD which include besides clinical and neuroimaging also biofluid, histological, etc., markers.
Additionally, an important further kind of marker will become deducible from prodromal longitudinal cohort studies, namely prodromal progression markers. These will be essential as endpoints for studies which aim to slow disease progression in the prodromal stages.
With new data arising from objective movement measurements, the earlier detection of motor symptoms will become possible. Objectively-measured markers such as reduced unilateral arm swing , impaired balance , wearable based markers of activity etc. indicate that we can expect to change our understanding of early motor PD. Keeping in mind that still several issues regarding sensor based assessments need to be solved including compliance and potential selection bias in populations who are willing to wear devices, a paradigm shift regarding appearance of first motor abnormalities and relationship to the current cardinal motor symptoms is likely.
Recommended Reading: Implant For Parkinson’s Disease
The Perilous Concept Of Prodromal Pd
Based on these data, prodromal PD criteria represent a promising tool for research purposes, to better investigate the possible risk to develop PD in presymptomatic patients. However, future methods to detect prodromal PD likely will require a multivariate hierarchical approach, and its power will depend on accessing markers over multiple possibly independent domains, such as genetic features, motor and non-motor symptoms, and ancillary diagnostic tests . Nonetheless, further investigations are requested to better understand the effective role of the different markers in research studies, such as those which have been recently conducted in REM SBD patients in order to identify new potential -synuclein biomarkers .
I Have Pd And Several Symptoms Should I Get A Datscan
Likely no. There is no need for DaTscan when your history and exam suggest Parkinsons disease and you meet the diagnostic criteria. Occasionally, if signs and symptoms are mild or you dont meet the diagnostic criteria, your doctor will refer you for a DaT scan. Keep in mind that ultimately the diagnosis is based on your history and physical exam. The DaT scan is most commonly used to complete the picture and is not a test for a diagnosis.
Read Also: How To Deal With Parkinson’s Disease
Sensitivity Specificity And Predictive Value Of A Previous Diagnosis Of Parkinson’s Disease
Of 126 patients with a pre-existing clinical diagnosis of probable and possible Parkinson’s disease in the overall sample , 111 were confirmed as having Parkinson’s disease, resulting in a sensitivity of 88.1% similarly, it was confirmed that 54 of 74 patients did not have Parkinson’s disease, resulting in a specificity of 73.0% . The positive and negative predictive values of a previous clinical diagnosis of Parkinson’s disease were 84.7% and 78.3% . In other words, in 85% of patients with a previous diagnosis of Parkinson’s disease this diagnosis was confirmed, and 78% of patients with a diagnosis other than Parkinson’s disease did not have the disease .
When this was broken down by a specialist or other doctor diagnosis, the diagnostic validity was as follows. Neurologists and geriatricians had a sensitivity and specificity of 93.5% and 64.5% , respectively, compared with 73.5% and 79.1% for non-specialists. The positive predictive values were greater for specialists than for other doctors , but the negative predictive values were equivalent v non-specialist 79.1% ).