Complications Of Pd: Akinetic Crisis
An akinetic crisis or acute akinesia is a life-threatening complication of PD that can be caused by a variety of issues including infections, medication errors, or failed surgery. A patient with AC becomes completely immobile, can no longer speak and no longer swallow. Accompanying symptoms include sweating and fast pulse. Such a crisis is dangerous and must be treated immediately. Without the ability to swallow, saliva can enter the lungs and cause pneumonia.
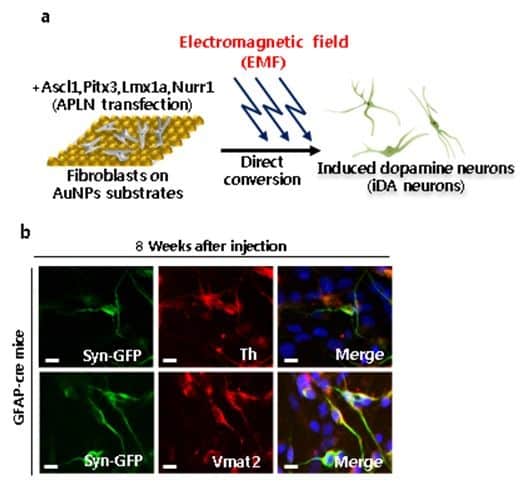
New Hope For Treatment Of Parkinsons Disease: Designer Neurons
The new research describes the implantation of induced pluripotent stem cells to replace dopamine-producing neurons destroyed by Parkinsons disease. Such cells not only survive the grafting procedure and manufacture dopamine, but send out their branching fibers through the neural tissue to make distant connections in the brain, just like their naturally-occurring counterparts. Credit: Shireen Dooling for the Biodesign Institute at Arizona State University
Neurodegenerative diseases cause neuronal damage and destruction, wreaking havoc on both mental and physical health. Parkinsons disease, which affects over 10 million people worldwide, is no exception. The most noticeable symptoms of Parkinsons disease arise after the illness damages a specific class of neuron located in the midbrain. The result is that dopamine, a key neurotransmitter produced by the affected neurons, is depleted in the brain.
In new research, Jeffrey Kordower and his colleagues describe a method for converting non-neuronal cells into functioning neurons able to take up residence in the brain, send out their fibrous branches across neural tissue, form synapses, dispense dopamine and restore capacities compromised by Parkinsons destruction of dopaminergic cells.
The work is supported through a grant from the Michael J. Fox Foundation.
New perspectives on Parkinsons disease
Neural alchemy
Studies Show Promising Results
“Considering the ability of MSCs to secrete neurotrophic factors, modulate inflammation, and possibly even act as mitochondria âdonorâ, it comes as no surprise that there is a lot of interest in the use of MSCs in the treatment of Parkinsons Disease, and a multitude of animal studies has shown promise. Treatments have resulted in improvement of motor function, protection of the nigrostriatal system, and improved striatal dopamine release in several studies using toxic lesion rodent models of Parkinsons Disease. Similar effects were reported with umbilical cord-derived MSCs with or without prior differentiation. For example, a recent study reported improvement of motor function, reduced microglial activation, and decreased loss of TH immunoreactivity, associated with local production of trophic factors.
Learn more about DVC Stem’s protocol for Parkinson’s Disease here:
References:
Venkataramana, N. K., Kumar, S. K. V., Balaraju, S., Radhakrishnan, R. C., Bansal, A., Dixit, A., ⦠Totey, S. M. . Open-labeled study of unilateral autologous bone-marrow-derived mesenchymal stem cell transplantation in Parkinson’s disease. Retrieved from https://www.sciencedirect.com/science/article/pii/S1931524409002205#!
Unified Parkinson’s Disease Rating Scale. . Retrieved from https://www.sciencedirect.com/topics/medicine-and-dentistry/unified-parkinsons-disease-rating-scale
About the author
Also Check: Rare Form Of Parkinson’s
What Have Clinical Trials Found
Until the discovery of the process of creating iPSCs, the only stem cell therapies for Parkinsons disease required the use of embryonic stem cells. This came with ethical and practical challenges, making research more difficult.
After iPSCs became available, stem cells have been used in clinical trials for many conditions involving neural damage with overall mixed results.
The first clinical trial using iPSCs to treat Parkinsons disease was in 2018 in Japan. It was a very small trial with only seven participants. Other trials have been completed using animal models.
So far, trials have shown improvement to symptoms affecting movement as well as nonmotor symptoms such as .
Some challenges do arise from the source of the stem cells.
Stem cell therapy can be thought of as being similar to an organ transplant. If the iPSCs are derived from a donor, you may need to use immunosuppressant drugs to prevent your body from rejecting the cells.
If the iPSCs are derived from your own cells, your body might be less likely to reject them. But experts believe that this will delay stem cell therapy while the iPSCs are made in a lab. This will probably be more costly than using an established line of tested iPSCs from a donor.
Disadvantages Of Stem Cell Approaches
While the stem cell approaches described potentially offer promising treatment approaches, a number of problems must be overcome in order for them to be used as a mainline treatment for PD.
Of course, any grafting therapy will require a neurosurgical procedure, and it must be demonstrated that this can be achieved safely, with minimal risk. Additionally, for allogenic grafts a period of immunosuppression will be required, with the associated risk of infection and malignancy. Having said this, there is postmortem evidence of FVM graft survival for over two decades, with only a transient period of immunosuppression, and taking into account the fact that the central nervous system is an immune-privileged site, it is unlikely that this will be a major problem .
It has been estimated that generating iPSCs from 150 human leukocyte antigen -typed individuals could allow for the development of haplobanks which would be able to provide HLA-matched cell products for over 90% of a population . This would mean that rather than an autologous grafting product being produced for each patient, that an iPSC line could be selected with which they were HLA compatible to generate a matched cell product. However, in order to achieve this, a degree of HLA mismatch would be necessary, and a period of immunosuppression would therefore probably be required. Additionally, this would still have significant economic costs .
Read Also: Flexibility Exercises For Parkinson’s Disease
A New Era For Parkinsons Disease Treatment
A non-invasive ultrasound treatment for Parkinsons disease that was tested in a pivotal trial led by University of Maryland School of Medicine researchers is now broadly available at the University of Maryland Medical Center .
Howard Eisenberg, MD, Dheeraj Gandhi, MD, MBBS, Paul Fishman, MD, PhD, Bert W. OMalley, MD.
The device, called Exablate Neuro, was approved in November by the U.S. Food and Drug Administration to treat advanced Parkinsons disease on one side of the brain. The approval was based on findings from the UMSOM clinical trial and effectively expands access to focused ultrasound beyond clinical trial participation.
Rapid Reversal of Symptoms
Focused ultrasound is an incisionless procedure, performed without the need for anesthesia or an in-patient stay in the hospital. Patients, who are fully alert, lie in a magnetic resonance imaging scanner, wearing a transducer helmet. Ultrasonic energy is targeted through the skull to the globus pallidus, a structure deep in the brain that helps control regular voluntary movement. MRI images provide doctors with a real-time temperature map of the area being treated. During the procedure, the patient is awake and providing feedback, which allows doctors to monitor the immediate effects of the tissue ablation and make adjustments as needed.
Patient: Focused Ultrasound Changed My Life
A New Era for Parkinsons Disease Treatment
Also Check: Pain Medication For Parkinsons Disease
Improvement Appears To Be Promising
Nisbet commented that the team has not yet conducted clinical trials, but it seems very promising in light of the results achieved on animals and indicated that the new hydrogel is cost-effective and easy to manufacture on a large scale and in large quantities, which means that it can be easily made available in hospitals when Its ready to be rolled out, but it has to go through clinical trials first, and if its approved, I really think it could revolutionize the treatment of this disease.
On their future steps, he continued: There are some small changes we are making to the hydrogel to check how we get it into the human body. which we hope will be available for use in the not-too-distant future.
Also Check: Complete List Of Parkinson’s Symptoms
What If We Could Reverse Lost Cell Function
offer a massive paradigm shift from current treatment options and hold the potential to revolutionize the way we treat diseases. These therapies focus on the source of the disease rather than the external manifestation of it. With these approaches we could potentially stop or even reverse the pathology of diseases like PD.
Stages Of Parkinsons Disease
Symptoms of Parkinsons vary person to person and can take a while to manifest, and the disease is regarded as slow moving or insidious onset. Early symptoms include Neuropathy and tremors with clumsy motions even when the limbs are at rest. Severe symptoms include muscle rigidity, bradykinesia, and gait disorders. Other non-motor symptoms include incontinent urine, depression, insomnia, and astriction. Neurologists have established the Hoehn and Yahr Scale, which consists of the five stages of PD to help classify patients in clinical trials and research studies around the world.
Don’t Miss: All Possible Symptoms Of Parkinson’s Disease
Dementia With Lbs Or Lb Disease
The second most frequent kind of dementia in advanced age is progressive dementia with LBs, typically accompanied by parkinsonism, good visual hallucinations, and oscillations in cognition, alertness, and concentration . DLB is dementia that affects the optical, perceptual, and careful functions of the brain . The age at which the DLB begins is 6068, with an average disease duration of 67. Men are more impacted than women . DLB diagnostic criteria differ substantially in their sensitivity and specificity and improved criteria are needed . Cases with more substantial DLB disease have typical symptoms, whereas cases with larger neurofibrillary tangles are likely to show AD . Continuing to work memory issues, visual spatial difficulties, psychotic episodes, melancholy, unconcern, and low mood are among early signs of DLB .
Cell Replacement Therapy For Parkinsons Disease Hurdles And Solutions
A successful cell transplantation has to be safe, well-tolerated by the recipient, and efficacious in reversing the symptoms of disease. It has been extremely well-established that loss of dopamine in the striatum is responsible for PD. Levodopa, which is a dopamine precursor, has been used to treat PD patients since that replaces the dopamine that is lost . Moreover, numerous animal studies have shown that transplanting dopaminergic neurons improves motor symptoms in PD animals . Even though there was sufficient evidence supporting that dopaminergic cells are clinically relevant for cell therapy in PD, there were aspects relating to their safety and reproducibility. Below, we list some of the hurdles that were eventually overcome so that stem cell derivatives can be used in the clinic.
Hurdle 1 deriving the right neural cell type for transplantation
Hurdle 2 eliminating the risk of tumorigenesis
Hurdle 3 transplanting floorplate progenitor cells, fully differentiated SNpc dopaminergic neurons or an intermediate?
Hurdle 4 source of stem cells: autologous or allogeneic? Fetal, ESC or iPSC-derived?
Hurdle 5 how many cells to transplant? Where to transplant?
Read Also: Music Therapy For Parkinsons
Recommended Reading: Clonazepam And Parkinson’s Disease
How Do Mesenchymal Stem Cells Work In The Body
Mesenchymal stem cells utilize their self-renewal, immunomodulatory, anti-inflammatory, signaling, and differentiation properties to influence positive change within the body. Mesenchymal stem cells also have the capacity to self-renew by dividing and developing into multiple specialized cell types present in a specific tissue or organ. Mesenchymal stem cells are adult stem cells, meaning they present no ethical concerns, MSCs are not sourced from embryonic material.
Dosing Begins In Phase 2a Trial Of Oral Treatment To Aid Cognition
Patient dosing has begun in a Phase 2a clinical trial testing oral CST-2032 in combination with CST-107 as a potential way to ease the symptoms of mild cognitive impairment and mild dementia due to Parkinsons or Alzheimers disease, the company developing these therapies, CuraSen Therapeutics, announced. The trial (
Read Also: Pain Meds For Parkinson’s
Major Stem Cell Transplant Breakthrough
- Major stem cell transplant breakthrough
In what represents significant advances in stem cells techniques for brain repair, Florey researchers have taken multiple approaches to improve safety and efficacy in the transplantation of dopamine brain grafts in Parkinson’s disease models.
As reported by The Herald Sun, researchers have cured movement problems caused by Parkinson’s disease in animals by transplanting stem cells directly into their brains.
The latest breakthrough has been enhanced after the Florey Institute of Neuroscience and Mental Health overcame two major hurdles in the way of progressing stem cell therapies.
They have boosted the quality and safety of stem cells being delivered, and worked out a way to stop transplanted cells developing into tumours.
The movement problems of Parkinson’s disease are treated with tablets that replace dopamine lost when nerve cells in the brain die.
But given these drugs travel around the body and can cause major side effects, a targeted delivery of dopamine directly into the brain is the holy grail.
A team led by Clare Parish has turned stem cells into dopamine cells, and injected them into the brains of animals to recreate the missing section of brain circuitry.
But one of the main strengths of these stem cells their ability to divide and continue growing rapidly is also their biggest weakness.
Clinical trials in the 1990s used varied qualities of stem cells, leading to serious side effects and even tumours in some patients.
Stem Cells For Parkinson’s Disease Are Safe And Effective
According the Venkataraman and colleagues, “A subjective improvement was found in symptoms like facial expression, gait, and freezing episodes 2 patients have significantly reduced the dosages of PD medicine. These results indicate that our protocol seems to be safe, and no serious adverse events occurred after stem-cell transplantation in PD patients.”
As stated in a 2005 study held by Brian Snyder,
Stem cells offer the potential to provide a virtually unlimited supply of optimized dopaminergic neurons that can provide enhanced benefits in comparison to fetal mesencephalic transplants. Stem cells have now been shown to be capable of differentiating into dopamine neurons that provide benefits following transplantation in animal models of Parkinson’s disease.
Don’t Miss: Good Exercises For Parkinson’s Disease
How Might Stem Cell Therapy Benefit Parkinsons
Researchers are exploring various approaches to use stem cells to treat Parkinsons disease.
The current idea is to introduce stem cells directly into the affected areas of your brain where they can transform into brain cells. These new brain cells could then help regulate dopamine levels, which should improve the symptoms of the disease.
Its important to note that experts believe this would only be a treatment for Parkinsons disease and not a cure.
While stem cell therapy has the potential to replace the brain cells destroyed by Parkinsons disease, the disease would still be present. Parkinsons disease would likely destroy the implanted stem cells eventually.
Its unclear right now whether stem cell therapy could be used multiple times to continue to reduce symptoms of Parkinsons disease or if the effect would be the same after multiple procedures.
Does It Work Efficacy Of Commercial Stem Cell Clinics
Commercial clinics do not as a rule publish their results in peer-reviewed journals to demonstrate to the scientific community that the treatments work. Rather, they usually rely on anecdotes from patients as proof of efficacy. Some clinics are tracking their results by measuring variables such as quality of life before or after the procedure. However, without comparing the patients to a similar group who does not receive the treatment, it is hard to know whether any improvement is due to placebo effect or to the treatment itself.
Don’t Miss: Physical Symptoms Of Parkinson’s Disease
What Is Cell Therapy
In cell therapy, healthy intact cells are cultured and transferred to the body to replace damaged cells associated with diseases. The human body is made up of around 200 different types of cells, each cell is specialized to carry out a particular role. Stem cells are rudimentary cells that havent undergone differentiation and can be induced to grow into any type of cell. The pioneering work of Noble prize winners, John Gurdon and Shinya Yamanaka marked a defining moment in this field enabling scientists to convert adult skin cells into what are called induced pluripotent stem cells . These cells can be differentiated using specific growth factors into most types of cells heart muscle, liver, or nerve cells.
BlueRock Therapeutics has studied the use of stem cell-derived neuron cells to replace damaged neurons in neurodegenerative diseases like PD and is now advancing a Phase 1 study in patients with advanced PD. The therapy is intended to restore motor function by replacing dopamine carrying neurons that are damaged by PD. The trial could potentially demonstrate that PD is, in principal, reversible and this in turn could represent an enormous step for people with PD worldwide.
Massive Pacemaker Cells Produced In Parkinson’s Breakthrough
Complete the form below and we will email you a PDF version of“Massive Pacemaker Cells Produced in Parkinson’s Breakthrough “
First Name*Would you like to receive further email communication from Technology Networks?Technology Networks Ltd. needs the contact information you provide to us to contact you about our products and services. You may unsubscribe from these communications at any time. For information on how to unsubscribe, as well as our privacy practices and commitment to protecting your privacy, check out our Privacy Policy
A new study led by a researcher in the Jacobs School of Medicine and Biomedical Sciences at the University at Buffalo has important implications for developing future treatments for Parkinsons disease , a progressive nervous system disorder that affects movement and often includes tremors.
In this study, we find a method to differentiate human induced pluripotent stem cells to A9 dopamine neurons , which are lost in Parkinsons disease, says Jian Feng, PhD, professor of physiology and biophysics in the Jacobs School and the senior author on the paper published May 24 in Molecular Psychiatry.
These neurons are pacemakers that continuously fire action potentials regardless of excitatory inputs from other neurons, he adds. Their pacemaking property is very important to their function and underlies their vulnerability in Parkinsons disease.
Also Check: End Stage Parkinson’s And Fever
Icipating In Clinical Trials
Ongoing clinical trials for treating Parkinsons disease using stem cell therapy may be available in your area. If this is something youre interested in, check back regularly, as new trials may be added later.
Be sure to mention your intentions to a doctor or healthcare professional as well. They may have additional information specific to your circumstances.