How To Cope With Dystonia
I have PD. First thing in the morning as I am getting out of bed, my left foot cramps severely and my toes curl downward, making it very painful to walk. I have found that it helps if I put my feet flat on the floor immediately after sitting up in bed. Also foot massages help. If I can force the cramped foot so it turns outward, my toes uncurl. nelleford
When my dads legs cramp, massage helps relieve them. You can usually feel where the spasms are. Rub your hands together to warm them up first. Start below where the spasm is and work up towards them. With your fingers and palms, give a deep massage where the cramp is. Give your loved one mustard or pickles to relieve the cramp. I know it is weird, but it works. To prevent them, exercise is best. Try to get them to walk every day, even if it is only half a block. This will also help prevent falls. A good multivitamin every day can be beneficial. Look for one with magnesium and potassium in it. These minerals helps to prevent cramping. My dad eats bananas almost every day for this reason. kathyt1
Calcium governs muscle contraction, and magnesium governs muscle relaxation. I take a magnesium supplement if Im having leg cramps. Perhaps have your loved ones levels evaluated with a simple blood test. Potassium can be dangerous if its too high or too low, and too low can often cause muscle cramps. sherry1anne
How To Deal With The 6 Common Causes Of Leg Pain In Pd
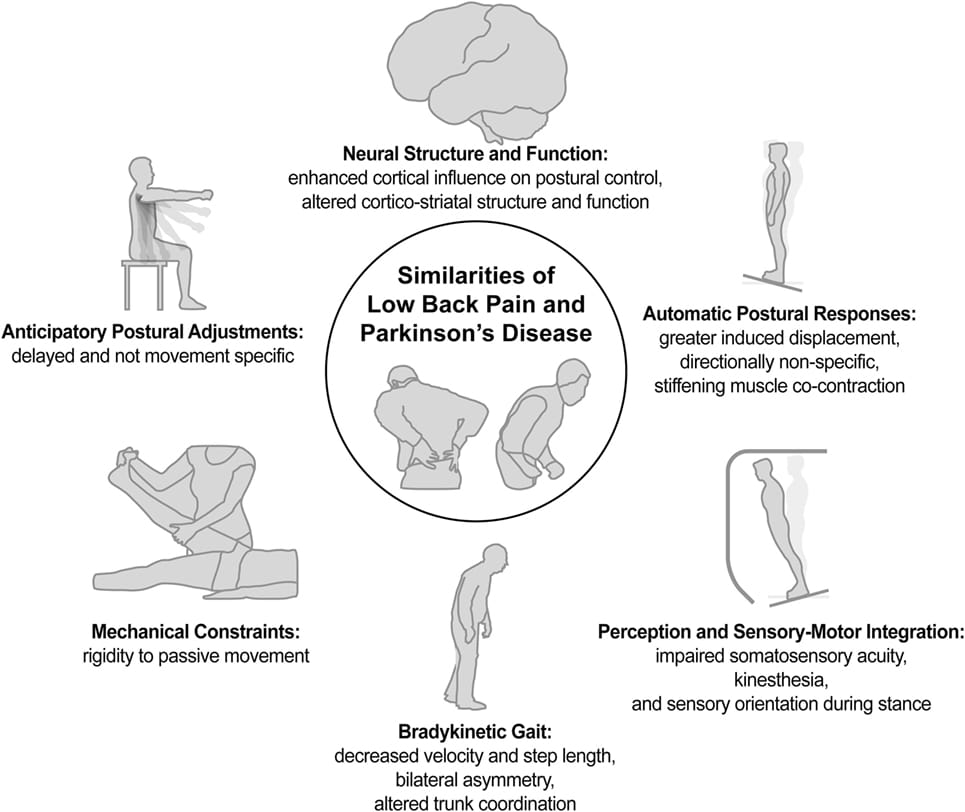
Severe leg pain is a common complaint from people with PD. Lately, it is understood that central pain is common to Parkinsons disease, and can even be the first sign of PD, usually bilaterally. This blog post lists six causes of lower limb pain, and the importance of treating it. Treatments depend on properly identifying the source of pain. Some treatment suggestions are included.
Negative Impact Of Severity Of Pain On Mood Social Life And General Activity In Parkinson’s Disease
This case control study designed for clinicians and rehabilitation specialists to effectively identify pain from the patient’s point of view determined that PD patients had significantly higher pain severity scores compared to controls. PD patients with depressive symptoms had significantly higher pain severity and pain interference scores than controls without depressive symptoms. PD patients reported greater scores on Global BPI pain interference and all components of the pain interference subscale. Therefore, PD and depression seem to be correlated with higher perceived pain, severity and interference. A report on this study, by Jose Marques Lopes, PhD., was published in Parkinson’s News Today, September 21, 2018.
Also Check: Therapy For Parkinson’s Disease Patients
Acpa And Stanford Resource Guide To Chronic Pain Management
This 213-page downloadable PDF is a comprehensive, integrated guide to medical, interventional, psychological/behavioral, pharmacologic, rehabilitative, complementary and integrative, and self-help strategies in the treatment of chronic pain. It covers general information compiled from multiple sources, is updated yearly and includes imbedded web links for certain medications and treatments and relevant internet sites of interest.
This questionnaire can help identify type of pain and determine whether someone should see a pain specialist.
Stages Of Parkinsons Symptoms
Parkinsons symptoms can be divided into three categories or phases: pre-motor, motor, and cognitive. These phases dont necessarily happen in chronological order, and not all Parkinsons patients will experience all symptoms.
The premotor phase is the phase of Parkinsons in which non-motor symptoms are present. These symptoms include:
There are two main categories of tremor: resting tremor, and action tremor. Resting tremor occurs when muscles are relaxed, like when your hands are sitting in your lap, and lessen during sleep or when the body part is in use. Action tremors occur with the voluntary movements of a muscle.
Tremors typically affect only one side of the body but may affect both sides as the disease progresses. Fatigue, stress, and intense emotion may worsen tremors.
Recommended Reading: Parkinson’s Disease And Death
How Exercise Can Help
Research shows that regular exercise has significant benefits for Parkinsons patients. Since the disease affects flexibility, strength, and balance, patients are encouraged to use targeted exercise routines to manage the disease.
A study review published in the Clinical Journal of Sport Medicinefound that exercise improves overall physical performance in Parkinsons patients. The authors concluded that future research should examine the long-term effects of exercise programs.
As a rock climber, I spend a lot of time pulling on jagged edges. Ive learned that its important to balance muscle growth with the opposite action. Ive integrated pushing into my routine to balance the pulling that I do on a rock wall. Focusing on both pushing and pulling helps my body to stay balanced and prevents injuries.
While I havent yet encountered a rock climber with Parkinsons, the same premise could apply. If Parkinsons causes constant muscle contractions, how can we encourage those muscles to extend and relax? Yoga emphasizes both strength and flexibility. And its possible to practice a routine at home. Starting a yoga practice might offer a solution to managing muscular changes.
Recommended Reading: How Do You Stop Parkinsons Tremors
What Are The Symptoms Of Parkinsons Disease
Symptoms of Parkinsons disease differ from person to person. They also change as the disease progresses. Symptoms that one person gets in the early stages of the disease, another person may not get until lateror not at all.
Symptoms most often start between the ages of 50 and 60. They develop slowly. They often go unnoticed by family, friends, and even the person who has them.
The disease causes motor symptoms and non-motor symptoms. Motor symptoms are those that have to do with how you move. The most common one is tremor.
Tremor and other motor symptoms
Tremor, or shaking, often in a hand, arm, or leg, occurs when youre awake and sitting or standing still . It gets better when you move that body part.
- Tremor is often the first symptom that people with Parkinsons disease or their family members notice.
- At first the tremor may appear in just one arm or leg or only on one side of the body. The tremor also may affect the chin, lips, and tongue.
- As the disease progresses, the tremor may spread to both sides of the body. But in some cases the tremor stays on just one side.
Emotional and physical stress tends to make the tremor more noticeable. Sleep, complete relaxation, and intentional movement or action usually reduce or stop the tremor.
The most common cause of non-Parkinsons tremor is essential tremor. Its a treatable condition that is often wrongly diagnosed as Parkinsons.
Besides tremor, the most common symptoms include:
You May Like: How Many Stages Of Parkinson’s Disease Are There
How Is It Diagnosed
Diagnosing Parkinson’s disease is mostly a clinical process, meaning it relies heavily on a healthcare provider examining your symptoms, asking you questions and reviewing your medical history. Some diagnostic and lab tests are possible, but these are usually needed to rule out other conditions or certain causes. However, most lab tests aren’t necessary unless you don’t respond to treatment for Parkinson’s disease, which can indicate you have another condition.
Other Symptoms: Aging Or Pd
Because the biggest risk factor for developing PD is age , skeletal problems associated with aging are often experienced by people with PD. While it is not clear that PD increases the risk or even the severity of these other skeletal conditions, the problems of PD can make the symptoms of these conditions more prominent.
- Osteoarthritis, the joint damage associated with general wear and tear on the joints, is nearly universal in aging. Osteoarthritis tends to affect larger joints such as the hip and knee.
- Arthritis of the spine is also very common. This may contribute to the development of spinal stenosis, narrowing of the canal in the spine that houses the spinal cord. In severe cases, spinal stenosis causes damage to the nerves as they exit the spine or even to the spinal cord itself.
- Disorders of the fibrous discs between the bones of the spine can also cause pain, or limb numbness or weakness.
Read Also: Parkinson’s Best Treatment Centers
Sciatica & Back Pain Relief
According to the American Physical Therapy Association, back pain is the most commonly reported pain across the nation, and one out of every four Americans has experienced back pain in the past three months. Back pain usually results from an injury or strain.
Sciatica, a specific type of back pain involving nerves that span into the legs, is also very common.Whether you are suffering from general back pain or sciatica, working with our physical therapists can help relieve the discomfort in your back and restore your health. Physical therapy may even eliminate your need for harmful painkilling drugs, such as opioids, or an invasive surgical procedure. If you are experiencing back pain, contact our office today. Our skilled physical therapists will create an individualized treatment regimen for you, focusing around your recovery.
Chronic Idiopathic Peripheral Neuropathy
Peripheral neuropathy refers to the feeling of numbness, tingling, and pins-and-needles sensation in the feet. Idiopathic means the cause is not known, and chronic means the condition is ongoing without getting better or worse.
The condition is most often found in people over age 60. Idiopathic neuropathy has no known cause.
Symptoms include uncomfortable numbness and tingling in the feet difficulty standing or walking due to pain and lack of normal sensitivity and weakness and cramping in the muscles of the feet and ankles.
Peripheral neuropathy can greatly interfere with quality of life, so a medical provider should be seen in order to treat the symptoms and reduce the discomfort.
Diagnosis is made through physical examination blood tests to rule out other conditions and neurologic and muscle studies such as electromyography.
Treatment involves over-the-counter pain relievers prescription pain relievers to manage more severe pain physical therapy and safety measures to compensate for loss of sensation in the feet and therapeutic footwear to help with balance and walking.
Rarity: Rare
Top Symptoms: distal numbness, muscle aches, joint stiffness, numbness on both sides of body, loss of muscle mass
Urgency: Primary care doctor
Don’t Miss: Parkinson’s Disease Disability Benefits Questionnaire
Is Paralysis An Accurate Term For Muscle Weakness During Parkinsons Disease
Paralysis is defined as the loss of muscle function of the body and is a curable condition. Stroke or injury such as spinal cord injury is considered as common and major causes of Parkinsons disease. Attack of paralysis may also occur in cases of cerebral palsy, post-polio syndrome, brain injury, etc.
In some cases, paralysis is a birth defect. Parkinsons attack is not a paralysis attack but because the symptoms for both are similar, people often cannot distinguish between the two.
Patients of Parkinsons disease also suffer from muscle weakness but it is not justified to categorize this muscle weakness as paralysis. In 1962, researcher Denny-Brown explained the difference between the two conditions. He stated that paralysis agitans occur with tremors and arteriosclerotic Parkinsonism is characterized by muscle rigidity and slowness of movement.
Paralysis is in itself is a disorder but there are some chances that patients of Parkinsons disease might suffer from it.
Although paralysis occurs due to some severe injury which results in cutting blood supply to the brain and Parkinsons disease is the degeneration of neurons, but in some cases, the main cause i.e. dopamine loss can correlate these conditions. Some patients experience internal tremors which might be vaguely stated as Parkinsons paralysis. If these tremors are severe and long-term then it is a serious concern among Parkinsons patients.
You May Like: Best Mattress Type For Back Pain
What Causes Numbness And Tingling In The Arms And Legs
Diabetic neuropathy is a nerve condition of the extremities causing numbness, tingling, and pain. Wernickes encephalopathy can cause confusion, lack of muscle coordination, and vision problems. Cold exposure symptoms include color changes on the skin, numbness, stinging, redness, blisters, and more.
There is no need for treatment other than patience. Its worthwhile to note that carpal tunnel syndrome can also cause numbness in the middle fingertip . However, there will be other symptoms with carpal tunnel syndrome.
Also Check: Glutathione Injections For Parkinsons
You May Like: Vegan Diet For Parkinson’s Disease
How Is Pain Treated In Patients With Parkinson Disease
Pain serves as 1 of the most frequent nonmotor complaints in patients with Parkinson disease , affecting 68% to 95% of patients across all clinical stages. Published in the Journal of Parkinson Disease, researchers highlight that similar to PD, pain is complex and even has different classifications of subtypes within the disease.
While prominent, real-life pain data in PD remains scarce. Researchers sought to provide an overview on pain in PD, including classification, assessment, presentation, and the existing therapy landscape.
As researchers highlighted, todays classifications of pain in PD include musculoskeletal, radicular/neuropathic, dystonia-related, akathic discomfort/pain, and central pain. Notably, the difference in pain directly related to PD and central pain, which is attributed to objective painprocessing and pain-perception disturbance within ascending and descending pathways, was referenced. Most frequently, pain presents as musculoskeletal/nociceptive pain in PD patients, but in nearly half of the PD population, comorbid conditions, such as spine and joint arthrosis, serve as contributors.
When it comes to treating pain in PD, interventions remain a major unmet need as only approximately 50% of those with the disease receive at least some type of pain therapy. In managing pain, researchers recommend that therapy should be optimized to address dopaminergic issues, which has been shown to be effective in 30% of patients with PD.
Reference
What Are The Symptoms
The best-known symptoms of Parkinson’s disease involve loss of muscle control. However, experts now know that muscle control-related issues aren’t the only possible symptoms of Parkinson’s disease.
Motor-related symptoms
Motor symptoms which means movement-related symptoms of Parkinsons disease include the following:
Additional motor symptoms can include:
- Blinking less often than usual. This is also a symptom of reduced control of facial muscles.
- Cramped or small handwriting. Known as micrographia, this happens because of muscle control problems.
- Drooling. Another symptom that happens because of loss of facial muscle control.
- Mask-like facial expression. Known as hypomimia, this means facial expressions change very little or not at all.
- Trouble swallowing . This happens with reduced throat muscle control. It increases the risk of problems like pneumonia or choking.
- Unusually soft speaking voice . This happens because of reduced muscle control in the throat and chest.
Non-motor symptoms
Several symptoms are possible that aren’t connected to movement and muscle control. In years past, experts believed non-motor symptoms were risk factors for this disease when seen before motor symptoms. However, theres a growing amount of evidence that these symptoms can appear in the earliest stages of the disease. That means these symptoms might be warning signs that start years or even decades before motor symptoms.
Non-motor symptoms include:
Stages of Parkinsons disease
Recommended Reading: Parkinson’s And Hearing Loss
Mental Status And Social Networks
As previously mentioned, depression and pain are significant clinical problems that are comorbid with PD. Marital status, as well as other social networks, interferes with these conditions.41 The patientspouse relationship, which indicates physical and emotional support, may have a mitigating effect on patient outcomes of depression prevalence and pain interference. Single PD patients seem to have greater pain interference scores than cohabiting PD patients.42
Fluctuations Of Pain Experiences In Pd
Patterns of NMS fluctuations are heterogeneous and complex. Psychic NMS seem to fluctuate more frequently and severely than nonpsychic symptoms. A recent study of ten frequent NMS in advanced PD using VAS rating scales in motor-defined on- and off-states, as well as self-ratings at home, confirmed previous suspicions that increased pain in off-states and pain fluctuations correlate with a low health-related quality of life.40 Pain as NMS was more frequent in the off-state more precisely, it was three to four times more common during the off-state than during the on-state.
Don’t Miss: Does Parkinson Cause High Blood Pressure
The Link Between Rls And Parkinsons: Dopamine Agonists
Although the cause of RLS remains unknown, we know that RLS runs in families in about one-half of the cases, and that some families have an abnormality on chromosome 12. Because RLS is well treated by medications that also treat Parkinsons disease, it is likely that some aspect of brain dopamine function is altered in RLS. However, unlike in Parkinsons disease, in which the deficit in substantia nigra dopamine-producing cells can be proven in many ways, no such abnormality has been shown in RLS. For example, studies show that there is no major deficit on PET or other imaging studies of the brain, as is there is in PD. The spinal fluid is normal in RLS, but shows low dopamine in PD.
Lastly, RLS does not progress to cause other major symptoms such as tremor, gait disorder, or loss of taste or smell, and does not progress to PD. In fact, one of the leading possibilities as the cause of RLS and for which there is good scientific evidence and much research is a form of iron-transport abnormality in the brain. In effect, RLS patients may have low levels of iron in brain nerve cellsjust the opposite of some portions of the brain in PD.
Dr. Poceta is a Consultant in Neurology and Sleep Disorders in the Division of Neurology, Scripps Clinic, La Jolla, and the Scripps Clinic Sleep Center. His current interests include organized medicine and Internet medicine.
Recommended Reading: What Causes Pain In Parkinsons Patients
Pain In Parkinsons Disease: A Spotlight On Women
This 2-page interview with neurologist, Dr. Jori E. Fleisher, discusses pain in Parkinsons disease with some interesting statistics about women and pain. Dr. Fleisher outlines the 4 primary types of pain in PD, how depression interferes with pain management, the role of exercise and medications in pain management as well as alternative therapies.
Don’t Miss: Is Swimming Good For Parkinson’s Disease