Complications Related To Parkinsons Can Affect Survival
Claudia Chaves, MD, is board-certified in cerebrovascular disease and neurology with a subspecialty certification in vascular neurology. She is an associate professor of neurology at Tufts Medical School and medical director of the Lahey Clinic Multiple Sclerosis Center in Lexington, Massachusetts.
Parkinsons is a common neurodegenerative disease, and although it is not fatal, research suggests it may influence life expectancy.
A 2012 study in Archives of Neurology examined the six-year survival of nearly 140,000 Medicare beneficiaries with Parkinsons disease in the United States. During the six-year period, 64% of the participants with Parkinsons disease passed away.
The risk of death of those with Parkinsons was then compared to Medicare beneficiaries who did not have Parkinsons or any other common diseases, including:
When controlling for variables like age, race, and gender, the six-year risk of death among people with Parkinsons was found to be nearly four times greater than those Medicare beneficiaries without the disease or other common diseases.
At the same time, the rate of death among those with Parkinsons disease was similar to those with hip fracture, Alzheimers dementia, or a recent heart attackalthough it was higher than those who had been newly diagnosed with either colorectal cancer, stroke, ischemic heart disease, or chronic obstructive pulmonary disease.
Also Check: 1st Sign Of Parkinsons
Lifestyle Changes To Improve Outcomes
Dr. Shulman and Dr. Mowry also shared how making certain lifestyle changesincluding regular exercise, a healthy diet, and plenty of quality sleepcan help people with Parkinsons and MS.
Exercise
Research shows that a combination of aerobic exercise, muscle strengthening, and stretching has the power to improve outcomes, symptoms, and mobility for people living with Parkinsons and MS.
Right now, if you were to ask what intervention has the most evidence delay the progression of Parkinsons disease, that is exercise, Dr. Shulman says. What you find is that there is a huge difference in the number of connections in the motor pathwaysa huge difference in the survival of the neurons, the nerve cells in those pathwaysand I think thats what were seeing in our patients.
Based on smaller studies, exercise also appears to be beneficial for managing some MS symptoms that dont typically respond well to medication. These symptoms include fatigue, which is one of the major symptoms of MS, as well as depression and anxiety. Exercise also reduces insulin resistance , which in turn lowers the risk of health issues like diabetes and high blood pressureboth of which have been shown to accelerate damage to the brain.
Diet
While overall research is inconclusive, one study suggests that people who eat a Mediterranean-style dietincluding fruits, vegetables, and fish and avoiding red meat and fatty foodsmay have a lower risk for developing MS.
For example:
Sleep
What Are The Later Secondary Signs And Symptoms Of Parkinson’s Disease
While the main symptoms of Parkinson’s disease are movement-related, progressive loss of muscle control and continued damage to the brain can lead to secondary symptoms. These secondary symptoms vary in severity, and not everyone with Parkinson’s will experience all of them, and may include:
You May Like: Parkinson’s Leg Pain Relief
Myth : Parkinsons Medications Cause Symptoms
Fact: Even though the myth that Parkinsons disease medicines are toxic and make the condition progress faster was completely debunked, it persists. Levodopa is the main drug therapy for Parkinsons disease. Its a potent drug that helps patients with motor symptoms. But many people got the idea that over time, it makes the disease progress faster. The myth was that levodopa is somehow toxic and is somehow making the Parkinsons progression faster, hurting patients.
This misconception was debunked decades ago with a large clinical trial, where it was found that people exposed to levodopa versus a placebo werent worse. In fact, they were better at the end of the study.
Its true that levodopa isnt a cure as yet, there is no cure for Parkinsons disease but its not toxic.
What Doctors Look For When Diagnosing Parkinsons
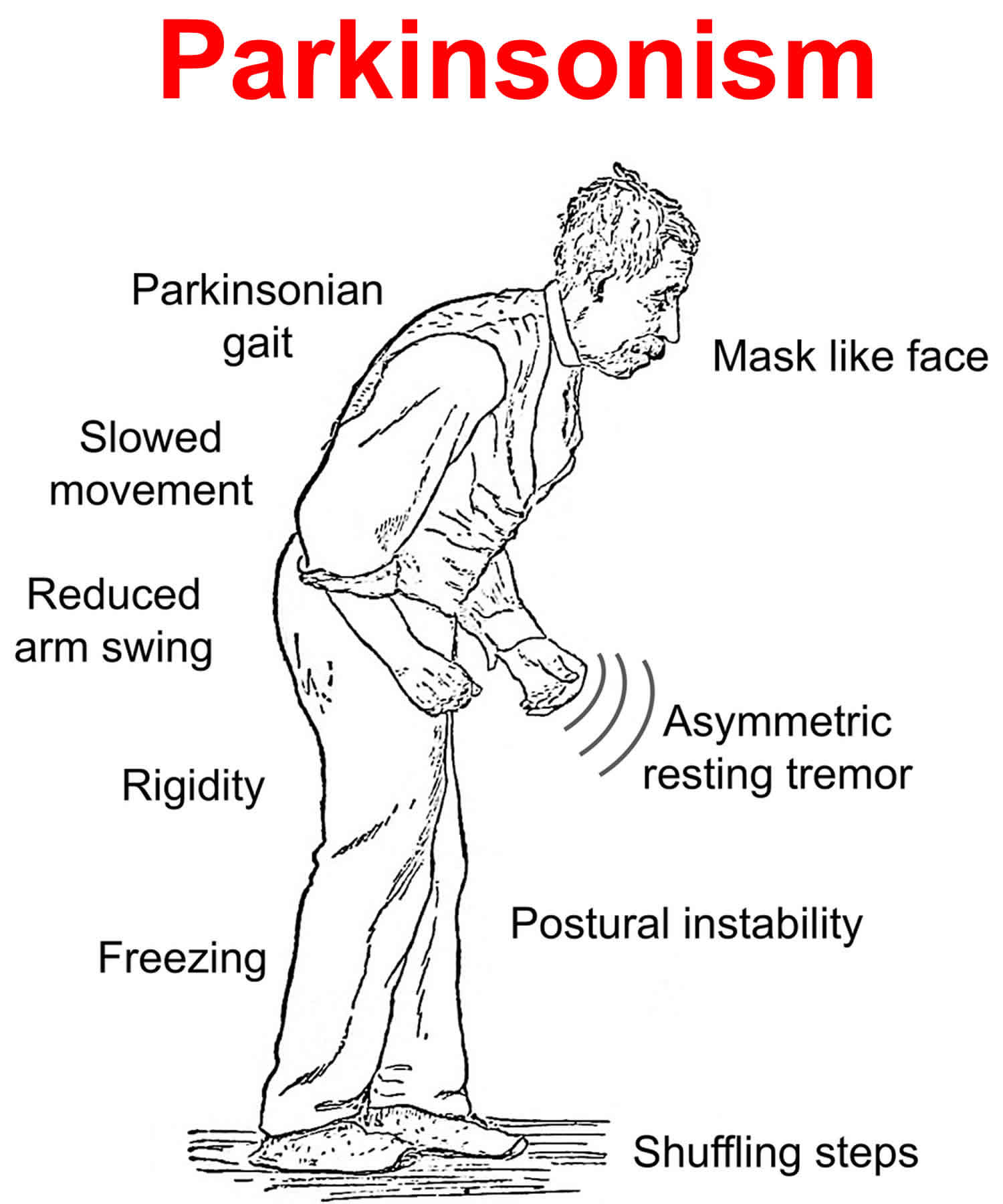
Certain physical signs and symptoms noticed by the patient or his or her loved ones are usually what prompt a person to see the doctor. These are the symptoms most often noticed by patients or their families:
-
Shaking or tremor: Called resting tremor, a trembling of a hand or foot that happens when the patient is at rest and typically stops when he or she is active or moving
-
Bradykinesia: Slowness of movement in the limbs, face, walking or overall body
-
Rigidity: Stiffness in the arms, legs or trunk
-
Posture instability: Trouble with balance and possible falls
Once the patient is at the doctors office, the physician:
-
Takes a medical history and does a physical examination.
-
Asks about current and past medications. Some medications may cause symptoms that mimic Parkinsons disease.
-
Performs a neurological examination, testing agility, muscle tone, gait and balance.
Recommended Reading: What Other Diseases Mimic Parkinsons
Don’t Miss: Agent Orange And Parkinson’s Disease
Slowness Of The Movement
Due to the lack of Dopamine, the signals from the brain to the muscles slowdown, that leads to Bradykinesia Bradykinesia slows down day to day activities of the patient, such as walking, bathing or dressing etc, and this is very disabling as it interferes routine life style. The patient may begin to shuffle and their walking steps become shorter and shorter and more likely they will have problems like starting and stopping and turning while walking and some patients may feel to be falling forward. All these walking complications are known as Parkinsons gait. Bradykinesia is considered to be a hallmark of basal ganglia disorders, and it includes difficulties with planning, initiating and executing movement and with performing sequential and simultaneous tasks .
You May Like: Is Thumb Twitching A Sign Of Parkinsons
What Is My Parkinsons Disease Prognosis
The outcome of Parkinsons disease varies from person to person, though women with the disorder tend to live longer than men. If you or a loved one has recently been diagnosed with Parkinsons, you may be wondering about the course of your illness and your life expectancy. While there is no definitive prognosis for Parkinsons, most doctors agree that the disease itself is not fatal. Health complications such as deep vein thrombosis and arterial blockage in the lungs can, however, shorten your lifespan with the condition, regardless of your age or gender.
These possible health complications may sound scary, but as long as you seek treatment, your life expectancy with Parkinsons disease shouldnt differ much from that of the general population.
You May Like: Does Parkinsons Cause Weight Gain
Also Check: Parkinson’s Disease And Cognition
Behaviors Seen In Parkinsons Disease Dementia
As dementia progresses, managing disorientation, confusion, agitation, and impulsivity can be a key component of care.
Some patients experience hallucinations or delusions as a complication of Parkinsons disease. These may be frightening and debilitating. Approximately 50 percent of those with the disease may experience them.
The best thing to do when giving care to someone experiencing hallucinations or delusions from Parkinsons disease dementia is to keep them calm and reduce their stress.
Take note of their symptoms and what they were doing before they exhibited signs of hallucinating and then let their doctor know.
This element of the disease can be particularly challenging for caregivers. Patients may become unable to care for themselves or be left alone.
Some ways to make caregiving easier include:
- sticking to a normal routine whenever possible
- being extra comforting after any medical procedures
- limiting distractions
- using curtains, nightlights, and clocks to help stick to a regular sleep schedule
- remembering that the behaviors are a factor of the disease and not the person
Parkinsons has four main symptoms:
- Tremor in hands, arms, legs, jaw, or head
- Muscle stiffness, where muscle remains contracted for a long time
- Slowness of movement
- Impaired balance and coordination, sometimes leading to falls
Other symptoms may include:
Sidebar: Morris K Udall Centers Of Excellence For Parkinson’s Disease Research
The Morris K. Udall Parkinsons Disease Research Act of 1997 authorized the NIH to greatly accelerate and expand PD research efforts by launching the NINDS Udall Centers of Excellence, a network of research centers that provide a collaborative, interdisciplinary framework for PD research. Udall Center investigators, along with many other researchers funded by the NIH, have made substantial progress in understanding PD, including identifying disease-associated genes investigating the neurobiological mechanisms that contribute to PD, developing and improving PD research models, and discovering and testing potential therapeutic targets for developing novel treatment strategies.
The Udall Centers continue to conduct critical basic, translational, and clinical research on PD including: 1) identifying and characterizing candidate and disease-associated genes, 2) examining neurobiological mechanisms underlying the disease, and 3) developing and testing potential therapies. As part of the program, Udall Center investigators work with local communities of patients and caregivers to identify the challenges of living with PD and to translate scientific discoveries into patient care. The Centers also train the next generation of physicians and scientists who will advance our knowledge of and treatments for PD. See the full list of Udall Centers.
You May Like: Tai Chi For Parkinson’s Video
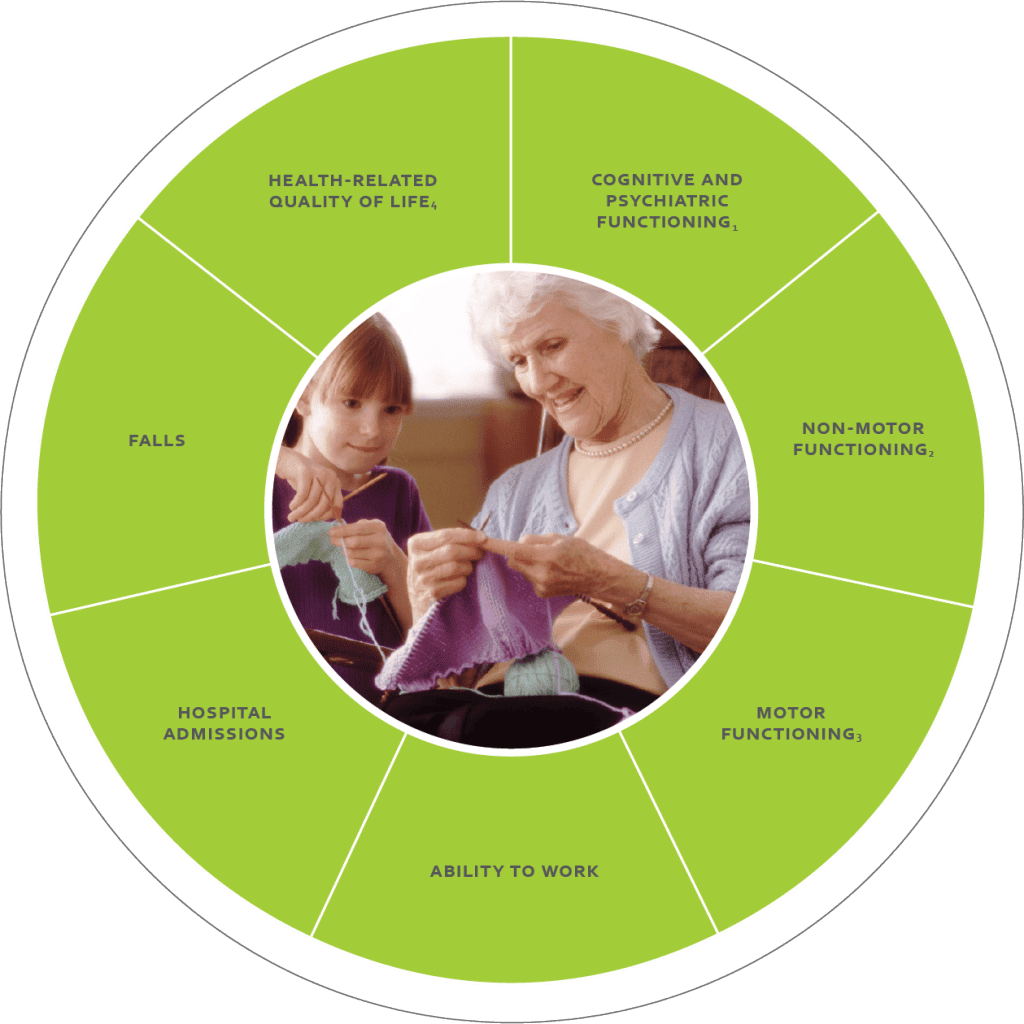
The Next Generation Of Parkinsons Research
The impact of the Parkinsons Outcomes Project continues to direct the work of the Parkinsons Foundation. Next, the study will next focus on recruiting more participants who are part of traditionally underrepresented populations in clinical research. The study will work to better understand the PD experiences of people with Young-Onset Parkinsons, newly diagnosed, early and late-stage disease progression and broader ethnic and racial diversity.
The Foundation is underway with the next phase of the study, genetic testing offered through PD GENEration: Mapping the Future of Parkinsons Disease. Genetic testing is a powerful tool that can help people learn more about their own disease, uncover biological pathways that cause Parkinsons and can accelerate the development of improved treatments and care for all people with Parkinsons.
Together, the Parkinsons Outcomes Project and PD GENEration will help researchers understand why and how Parkinsons develops, said James Beck, PhD, Parkinsons Foundation Chief Scientific Officer. These initiatives may also answer questions that researchers may never have asked, providing hope and a vision towards a cure for PD.
For the full update from the field, read Parkinsons Outcome Project: Improving the lives of people living with Parkinsons through research. In this publication, we highlight landmark findings, how this research guides Foundation priorities, whats next for the study and more. Read it now.
Parkinsonian Signs And Rating Scales In The Prodromal Period
It is clear that in the research setting, where lengthy trials are not feasible for both cost and scientific reasons, surrogate outcome measures with sufficient lead timeâthat is, outcome measures that reflect pathologically confirmed PD years before it can be clinically establishedâare critically needed. Motor abnormalities are a key candidate for such markers. Individuals who are at risk for PD present clinically with motor and nonmotor symptoms of the prodromal state years before diagnosis., In a case-control study of 8,166 individuals with PD and 46,755 individuals without PD presenting to primary case, symptoms of tremor, shoulder pain/stiffness, and rigidity were significantly more likely to occur in those who developed PD vs those who did not, and presenting symptoms of tremor, balance problems, and rigidity independently predicted PD diagnosis.
Longitudinal Studies Assessing Risk of Progression or Conversion Associated With Performance on Rater-Derived Motor Outcomes
Prospective longitudinal studies of asymptomatic carriers of genetic mutations associated with increased risk of PD, such as mutations in glucocerebrosidase A , or leucine-rich repeat kinase 2 genes, indicate small but measurable changes in motor function compared with controls in these at-risk populations as well.
Read Also: What Percentage Of Parkinson’s Is Hereditary
What Causes Parkinsons Disease
The most prominent signs and symptoms of Parkinsons disease occur when nerve cells in the basal ganglia, an area of the brain that controls movement, become impaired and/or die. Normally, these nerve cells, or neurons, produce an important brain chemical known as dopamine. When the neurons die or become impaired, they produce less dopamine, which causes the movement problems associated with the disease. Scientists still do not know what causes the neurons to die.
People with Parkinsons disease also lose the nerve endings that produce norepinephrine, the main chemical messenger of the sympathetic nervous system, which controls many functions of the body, such as heart rate and blood pressure. The loss of norepinephrine might help explain some of the non-movement features of Parkinsons, such as fatigue, irregular blood pressure, decreased movement of food through the digestive tract, and sudden drop in blood pressure when a person stands up from a sitting or lying position.
Many brain cells of people with Parkinsons disease contain Lewy bodies, unusual clumps of the protein alpha-synuclein. Scientists are trying to better understand the normal and abnormal functions of alpha-synuclein and its relationship to genetic mutations that impact Parkinsons andLewy body dementia.
How Is It Diagnosed
Diagnosing Parkinson’s disease is mostly a clinical process, meaning it relies heavily on a healthcare provider examining your symptoms, asking you questions and reviewing your medical history. Some diagnostic and lab tests are possible, but these are usually needed to rule out other conditions or certain causes. However, most lab tests aren’t necessary unless you don’t respond to treatment for Parkinson’s disease, which can indicate you have another condition.
You May Like: Home Help For Parkinson’s Patients
How Is It Treated And Is There A Cure
For now, Parkinsons disease is not curable, but there are multiple ways to manage its symptoms. The treatments can also vary from person to person, depending on their specific symptoms and how well certain treatments work. Medications are the primary way to treat this condition.
A secondary treatment option is a surgery to implant a device that will deliver a mild electrical current to part of your brain . There are also some experimental options, such as stem cell-based treatments, but their availability often varies, and many aren’t an option for people with Parkinsons disease.
How Is A Diagnosis Made
Because other conditions and medications mimic the symptoms of PD, getting an accurate diagnosis from a physician is important. No single test can confirm a diagnosis of PD, because the symptoms vary from person to person. A thorough history and physical exam should be enough for a diagnosis to be made. Other conditions that have Parkinsons-like symptoms include Parkinsons plus, essential tremor, progressive supranuclear palsy, multi-system atrophy, dystonia, and normal pressure hydrocephalus.
You May Like: Cost Of Parkinson’s Treatment
The Evolution Of Treatment For Parkinsons Disease
Researchers have found that people with Parkinsons have low levels of dopamine, a neurotransmitter that sends signals between nerve cells and helps control body movements. Levodopa is currently the main drug-based treatment of choice for Parkinsons disease. It works by replacing missing dopamine and reducing motor symptoms, such as muscle stiffness.
While this medication has been around for more than half a century, during that time research has made significant strides in improving diagnosis and delaying disability for people with Parkinsons. When I started in the field, we would think in terms of people having considerable problems 5 to 10 years after diagnosis, says Dr. Shulman. Today its quite common to see people who are 15 or more years after diagnosis who live active livesnot to say asymptomatic, but theyre able to maintain a good lifestyle in many cases.
Part of this progress has been due to an expansion of medications and surgical treatment options, allowing doctors to fine-tune a persons treatment plan to their specific symptoms and needs. Surgical treatmentsincluding deep brain stimulation and focused ultrasoundcan improve symptoms and reduce involuntary movements. While they were previously thought to be a last resort, doctors have learned that surgical interventions can have a positive impact on disability and quality of life when used in earlier stages of Parkinsons disease.
Depression May Be An Early Symptom Of Parkinsons
Depression is one of the most common, and most disabling, non-motor symptoms of Parkinsons disease. As many as 50 per cent of people with Parkinsons experience the symptoms of clinical depression at some stage of the disease. Some people experience depression up to a decade or more before experiencing any motor symptoms of Parkinsons.
Clinical depression and anxiety are underdiagnosed symptoms of Parkinsons. Researchers believe that depression and anxiety in Parkinsons disease may be due to chemical and physical changes in the area of the brain that affect mood as well as movement. These changes are caused by the disease itself.
Here are some suggestions to help identify depression in Parkinsons:
- Mention changes in mood to your physician if they do not ask you about these conditions.
- Complete our Geriatric Depression Scale-15 to record your feelings so you can discuss symptoms with your doctor. Download the answer key and compare your responses.
- delusions and impulse control disorders
Recommended Reading: Off Episodes Parkinson’s Treatment
Study Designs And Descriptions Of Included Studies
The 42 studies were published until February 2020. The study designs were: retrospective cohort studies, prospective cohort and longitudinal studies, casecontrol studies and cross-sectional studies. Predictors of mortality included demographic and clinical markers, medical events, medication changes, disease-specific symptoms and patient and caregivers ratings of health-related quality of life. Eight studies described both predictors of mortality and causes of death.
How Is Parkinsons Disease Diagnosed
Diagnosing Parkinsons disease is sometimes difficult, since early symptoms can mimic other disorders and there are no specific blood or other laboratory tests to diagnose the disease. Imaging tests, such as CT or MRI scans, may be used to rule out other disorders that cause similar symptoms.
To diagnose Parkinsons disease, you will be asked about your medical history and family history of neurologic disorders as well as your current symptoms, medications and possible exposure to toxins. Your doctor will look for signs of tremor and muscle rigidity, watch you walk, check your posture and coordination and look for slowness of movement.
If you think you may have Parkinsons disease, you should probably see a neurologist, preferably a movement disorders-trained neurologist. The treatment decisions made early in the illness can affect the long-term success of the treatment.
Read Also: Long Term Effects Of Parkinson’s Disease