The Cause Of Parkinsons Delusions And Hallucinations
Some risk factors associated with the development of psychosis in Parkinsons disease include:
- Age: Parkinsons disease usually occurs in people over age 60.
- Duration and severity of Parkinsons disease: Psychosis is more common in advanced or late-stage Parkinsons disease.
- Later onset: Occurring later in life
- Hyposmia: A decreased sense of smell
- Cognitive impairment: Problems with thinking, including trouble remembering, difficulty learning new things, difficulty concentrating, problems making decisions that affect everyday life
- Depression: People who have both depression and Parkinsons disease are at a greater risk of developing psychosis.
- Diurnal somnolence: Daytime sleepiness
- REM sleep behavior disorder: A sleep disorder in which you physically act out dreams involves making vocal sounds and sudden, often extreme, arm and leg movements during REM sleep
- Visual disorders: Impaired vision
- Severe axial impairment: Speech, swallowing, balance, freezing of gait
- Autonomic dysfunction: Impairment of the autonomic nervous system , which controls involuntary or unconscious actions such as heart rate, breathing, body temperature, blood pressure, digestion, and sexual function
- High medical comorbidity: The existence of more than one condition or illness in the same person at the same time with Parkinsons disease, may include conditions such as dementia, depression, and sleep disorders
How Are They Treated
Your medical team should be aware of non-motor issues, just like your physical symptoms. Internists, neurologists, and psychiatrists together can help determine the right course for each person.
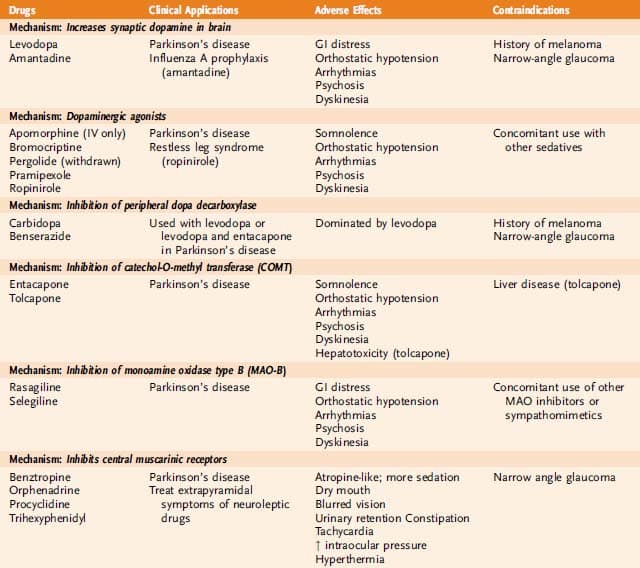
There are antipsychotic medications that are safe and can help to reduce the symptoms of Parkinson’s disease psychosis, but there are even more antipsychotics that are contraindicated for PD.
Let a medical provider know you have Parkinson’s when seeking emergency care or treatment for something by doctors who are not a part of your regular medical team.
There is only one drug, pimavanserin, approved in 2016 by the FDA specifically for PD. It has a mechanism of action that doesn’t block dopamine. This has made it a safer drug for people with Parkinson’s.2
Two other medications, quetiapine and clozapine, that have been used for a longer time, are also considered safe for treating hallucinations and delusions in people with PD.2
Visual Hallucinations According To The Duration Of Parkinson’s Disease
The prevalence of hallucinations of all types and of visual hallucinations in the 3 months preceding inclusion in the study increased with the duration of Parkinson’s disease . We compared the characteristics of the patients with and without hallucinations among those with a short history of Parkinson’s disease and those with a long history . The results are shown in Table 7. Visual hallucinations had been present for a mean of 0.8 years in the patients with short-duration Parkinson’s disease and for 2.4 years in the patients with long-duration Parkinson’s disease . However, eight patients with long-duration Parkinson’s disease and one patient with short-duration Parkinson’s disease could not remember the year of onset of visual hallucinations. In both groups, patients with formed visual hallucinations were older and were more likely to be demented, according to DSM criteria, than non-hallucinators. The MMP score was lower in patients with visual hallucinations, although the difference reached significance only in patients with long-duration Parkinson’s disease. Patients with visual hallucinations had a more severely affected motor state than non-hallucinators in the long-duration group only.
Also Check: Parkinson’s Disease Constipation Treatment
Get The Every Victory Counts Manual For Care Partners
Do you have the Every Victory Counts Manual for Care Partners! Released in 2021, this resource is available at no cost in print and digital versions. To learn more and request your copy, .
This content was supported in part by Acadia Pharmaceuticals. To learn more about Parkinsons disease psychosis, visit moretoparkinsons.com
Behaviors Seen In Parkinsons Disease Dementia
As dementia progresses, managing disorientation, confusion, agitation, and impulsivity can be a key component of care.
Some patients experience hallucinations or delusions as a complication of Parkinsons disease. These may be frightening and debilitating. Approximately 50 percent of those with the disease may experience them.
The best thing to do when giving care to someone experiencing hallucinations or delusions from Parkinsons disease dementia is to keep them calm and reduce their stress.
Take note of their symptoms and what they were doing before they exhibited signs of hallucinating and then let their doctor know.
This element of the disease can be particularly challenging for caregivers. Patients may become unable to care for themselves or be left alone.
Some ways to make caregiving easier include:
- sticking to a normal routine whenever possible
- being extra comforting after any medical procedures
- limiting distractions
- using curtains, nightlights, and clocks to help stick to a regular sleep schedule
- remembering that the behaviors are a factor of the disease and not the person
You May Like: Parkinson’s Disease And Urination
Some Examples Of Delusions And Their Impact In Pd Include:
- Belief: Your partner is being unfaithful.
- Behavior: Paranoia, agitation, suspiciousness, aggression
Hallucinations Delusions And Parkinson’s
It is estimated that about 50% of people with Parkinsons will, at some point, experience hallucinations. They can affect younger people but are more often associated with those who are older and have had Parkinsons for some time.
Hallucinations experienced early in Parkinsons may also be a symptom of the condition dementia with Lewy bodies so it is important to let your doctor know if hallucinations begin at an early stage.
Parkinsons itself can be a cause of hallucinations and delusions, but very often they are a side effect of certain medications used to treat the condition. Not everyone who takes Parkinsons medications will experience hallucinations and delusions though. This varies from person to person and is often related to the particular type of medication and dosage.
Other factors may also be involved such as underlying illness, memory problems, sleep difficulties and poor eyesight.
Read Also: The Michael J Fox Foundation For Parkinson’s Research Glassdoor
They Mistake Objects For People Or Animals
The most common symptoms of Parkinsons related psychosis are visual illusions and hallucinations, says Dr. Barrett. These can start out mild, with the person looking at an object but seeing something else. For example, they might mistake a lamp for a human or think the mailbox is a deer. These are early, minor hallucinations that may evolve to be more bothersome or pervasive, says Barrett.
Risk Factors For Parkinsons Hallucinations
Not much is known about what causes hallucinations with Parkinsons disease. Because people living with Parkinsons disease also are at risk of vision impairment, these problems may contribute to the occurrence of hallucinations. Older people and those with advanced stages of Parkinsons also tend to have a higher risk of hallucinations.
Hallucinations can be a side effect of a medication or caused by an infection. In these cases, the hallucinations are related to Parkinsons but not caused by the disease itself.
You May Like: American Parkinson’s Disease Association
What Makes Some People With Parkinsons More Susceptible To Parkinsons Disease Psychosis
Not everyone living with Parkinsons will experience hallucinations and/or delusions, but there are several things that can increase your risk. Here are a few to look out for. Be sure to speak to your doctors and care partners if you notice any changes.
- Increased sleep disturbances such as REM Sleep Behavior Disorder, sleep apnea, vivid dreaming and sleep interruptions
- Vision problems such as blurry or double vision
- Hearing problems
- Medication changes such as new medication, dosage changes and drug interactions
- Disease progression
How To Cope With Parkinson’s Psychosis
Caregivers of people with PD and other neurological conditions that cause hallucinations and delusions can engage in a variety of behavioral interventions to keep their loved ones calm and in control during a psychotic event. However, the effectiveness of approaches like redirection and validation therapy depend on the severity and frequency of ones episodes. While these techniques may prove helpful from time to time, Dr. Dewey believes that these efforts are generally unsuccessful over the long term. The best step is to notify your loved ones doctor at the first sign of new or worsening psychotic symptoms to avoid unnecessary injury, stress and even placement in a long-term care facility.
It is important to maintain an honest relationship with your loved one, asking often about any abnormal ideas and experiences they may be having. Family members are usually surprised to learn that their loved one is experiencing these episodes, because many patients with PD are reluctant to divulge this information unless specifically asked.
Remember that not all PD patients will experience severe hallucinations or delusions. If your loved one seems to be doing well, exercise caution when any dosages are changed or medications are added or discontinued. Tweaking a medication regimen should ideally happen one change at a time in order to pinpoint positive and negative effects of a single variable.
Read Also: What Medication Does Michael J Fox Take For Parkinson’s
What Is Parkinsons Disease Psychosis
As Parkinsons Disease progresses, up to 40 percent of the approximately one million Americans living with the illness will develop psychotic symptoms, primarily hallucinations, but also delusions. These symptoms can be an indication of Parkinsons disease psychosis , but unfortunately, many patients are not diagnosed. Sometimes, the symptoms of PDP are misdiagnosed. Other times, patients and their families may not be comfortable sharing the symptoms with their physician team.
How Commonly Do Parkinsons Disease Patients Develop Psychosis

Psychosis in Parkinsons disease generally comes in two forms: hallucinations or delusions . When hallucinations occur, they are mostly visual . Sometimes, they can be threatening, but this is less common. Auditory hallucinations are rare in Parkinsons disease and if they do occur, they are usually accompanied by visual hallucinations.
Delusions are usually of a common theme, typically of spousal infidelity. Other themes are often paranoid in nature Because they are paranoid in nature, they can be more threatening and more immediate action is often necessary, compared to visual hallucinations . It is not uncommon that patients actually call 9-1-1 or the police to report a burglary or a plot to hurt them.
Unfortunately, psychosis occurs in up to 40% of Parkinsons disease patients . In the early stage of Parkinsons disease psychosis, the patient often still has a clear understanding and retains their insight, but this tends to worsen over time and insight may eventually be lost. At later stages, patients may be confused and have impaired reality testing that is, they are unable to distinguish personal, subjective experiences from the reality of the external world. Psychosis in Parkinsons disease patients frequently occurs initially in the evening, then later on spills into the rest of the day.
Recommended Reading: Medicine For Parkinson’s Hallucinations
Treatment For Parkinsons Hallucinations
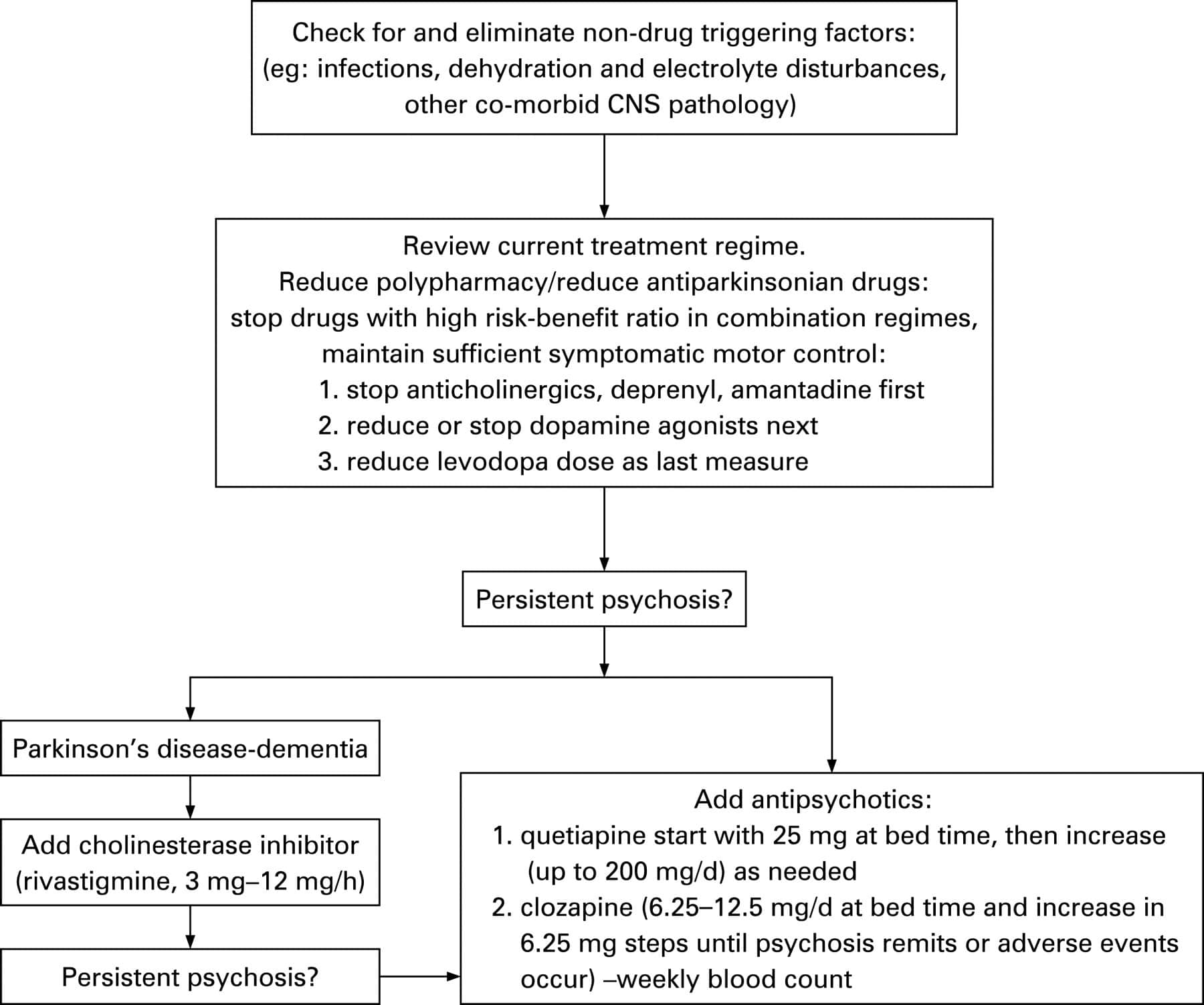
Treatment for Parkinsons hallucinations depends on what is causing the hallucinations. Here are treatment approaches considered for the management of Parkinsons hallucinations.
- Hallucinations induced by medication: For people who experience Parkinsons hallucinations as a result of medication, your doctor may tweak your dose in hopes that it can stop the side effect. High dosages of certain medications can cause Parkinsons hallucinations.
- Other co-occurring conditions: If you begin to experience hallucinations in the early stages of Parkinsons disease, your doctor will put you through a series of tests to rule out other co-occurring conditions. Dementia which commonly co-occurs with Parkinsons disease can cause hallucinations.
- Medical intervention: In severe cases where hallucinations inhibit a persons quality of life, medication may be prescribed to help reduce their severity and occurrence. Antipsychotic drugs are most commonly used to manage symptoms of hallucinations. However, they have bothersome side effects such as cognitive and motor decline. Your doctor will make the call on whether living with these side effects outweighs your need for the medication. In 2016, the FDA approved a medication called Nuplazid , specifically formulated to treat symptoms of hallucinations and delusions in people with Parkinsons disease.
How Does Essential Tremor Develop
Essential tremor symptoms often first appear in a persons 40s, when delicate movements such as threading a needle become difficult. But its usually not until people reach their 50s or 60s that the tremor becomes troublesome for example, making it difficult to use a fork, drink from a cup, or write a letter. Essential tremor progresses slowly. Though essential tremor may eventually affect the voice and head, many people find that their symptoms dont progress beyond mild hand and arm tremor. Tremors are usually absent during sleep.
We dont know the precise cause of essential tremor. Some experts believe that the problem lies in the cerebellum or its connections with the brainstem, which lies at the base of the brain. Essential tremor is a heritable condition. If you have essential tremor, your children will have a 50% chance of developing it as well.
Also Check: Parkinson’s Dementia And Weight Loss
The Relationship Between Parkinsons Disease And Sleep
Its unclear whether poor sleep causes parkinsonian symptoms to worsen or whether worsening parkinsonian symptoms cause poor sleep. In many cases its likely a case of bidirectionality, with each one exacerbating the other.
Fragmented sleep and sleep deprivation appear to leave the brain more vulnerable to oxidative stress, which has been tied to the development of Parkinsons disease. Parkinsons disease is not usually diagnosed until individuals have developed sufficient motor symptoms, by which time a significant portion of brain cells have already been damaged. If poor sleep quality or having sleep disorders foreshadows the development of parkinsonian symptoms, these could be useful in early diagnosis of the disease.
More research is needed to clarify the multifaceted relationship between Parkinsons disease and sleep. A better understanding of this connection may offer medical experts the unique opportunity to screen at-risk individuals and perhaps delay the onset of the disease.
Similar Articles Being Viewed By Others
Carousel with three slides shown at a time. Use the Previous and Next buttons to navigate three slides at a time, or the slide dot buttons at the end to jump three slides at a time.
09 September 2021
Ning-Ning Che, Qiu-Huan Jiang, Hong-Qi Yang
15 June 2022
Yael Lustig-Barzelay, Ifat Sher, Ygal Rotenstreich
volume 10, Article number: 21110
You May Like: Crafts For Parkinson’s Patients
Address Possible Underlying Causes
Sometimes underlying health problems, from acute infections to metabolic changes, can be linked with psychosis, says Dr. Espay. When people develop unexpected psychotic symptoms, Espay says he sometimes orders blood tests to check for infections or changes in kidney or liver function in his patients that may contribute to a change in symptoms.
Also Check: Treatment Of Orthostatic Hypotension In Parkinsons Disease
Hallucinations And Delusions In Pd
Hallucinations and delusions are collectively referred to as psychosis.
Visual hallucinations are the most common type of hallucination. In a visual hallucination, someone sees things that are not actually there. There can also be auditory and olfactory hallucinations. Often hallucinations are not alarming to the person experiencing them.
Delusions are when there is an alternative view of reality: an entire irrational story is created. Paranoia is a common type of delusion. Capgras delusions are a specific type of delusion where the person believes that a spouse, adult child, or other family member has been replaced by an imposter.
Also Check: How To Control Parkinson’s Tremors
How To Care For Someone Who Experiences Hallucinations
If the person you care for experiences a hallucination, there are a few things youll want to do in the moment and others youll want to do when the moment passes.
The most important thing to remember is to never try and talk the person with Parkinsons out of their hallucination. They are actively experiencing it and by trying to talk them out of it, they may either feel like they arent being heard or that their experience is being diminished.
What matters in the moment is their safety and your reassurance that theyre going to be okay. You might calmly say, I understand that youre seeing X. Im not having that experience, and I just want you to know that everything is going to be okay, theres nothing dangerous happening here and youre safe.
Other strategies Dr. Joanne Hamilton, PhD, ABPP-CN of Advanced Neurobehavioral Health of Southern California, shared with us are to:
Here are a few actions you can take once the hallucination has passed:
What Else Can I Do To Sleep Better With Parkinsons Disease
Practicing healthy sleep hygiene habits may also promote more restful sleep.
- Get outside during the day. Bright light tells your body its time to be awake.
- Keep your body moving during the day. Even if all you feel up to is a short walk or two, all physical activity offers benefits.
- Try at-home remedies, such as massage or a warm bath. Relaxing your mind may help your body fall asleep.
Dont:
- Take long naps during the day.
- Use stimulants, such as caffeine, within six hours of bedtime.
- Use your bedroom for activities other than sleeping. Go to another room to read, watch TV or work.
Read Also: Speed Of Parkinson’s Progression
Tremor In Other Conditions
While tremor is a common symptom of Parkinsons, it can also be a symptom of other conditions, most notably essential tremor. The main difference between Parkinsons tremor and most other types of tremor is that in Parkinsons resting tremor is most common. Other conditions are usually characterized by action tremor, which tends to lessen at rest and increase when youre doing something, like trying to make a phone call or take a drink.
Tremors of the head and voice are also common in essential tremor but rare in Parkinsons.