What Are Parkinsons Disease Dementia Medical Treatment And Medications
There is no specific therapy for dementia in Parkinsons disease. Although cognitive symptoms initially may appear to respond to drugs that promote dopamine production, the improvement is mild and transient in contrast to the early responses to motor control improvement with medication in patients with Parkinsons disease.
Parkinsons disease dementia medications
Various medications are used to treat the movement disorders of Parkinsons disease, some may exacerbate symptoms related to dementia.
- These include dopamine given in the form of levodopa medications known as dopamine agonists that act on the dopamine receptor and medications that slow down the metabolism of dopamine. They are often used in conjunction with monoamine oxidase inhibitors such as rasagiline. In addition, anticholinergic drugs are sometimes used.
- Unfortunately, these drugs may affect cognitive symptoms and mood disorders.
- Anticholinergic drugs, for example, help balance levels of dopamine and acetylcholine, another neurotransmitter, in the brain. These drugs can improve movement disorders but often make memory loss worse.
The dementia of Parkinsons disease may respond to drugs used in patients with Alzheimers disease. However, these drugs, called cholinesterase inhibitors , lead to only small and temporary improvements in cognition.
Mood disorders and psychoses are usually treated with other medication.
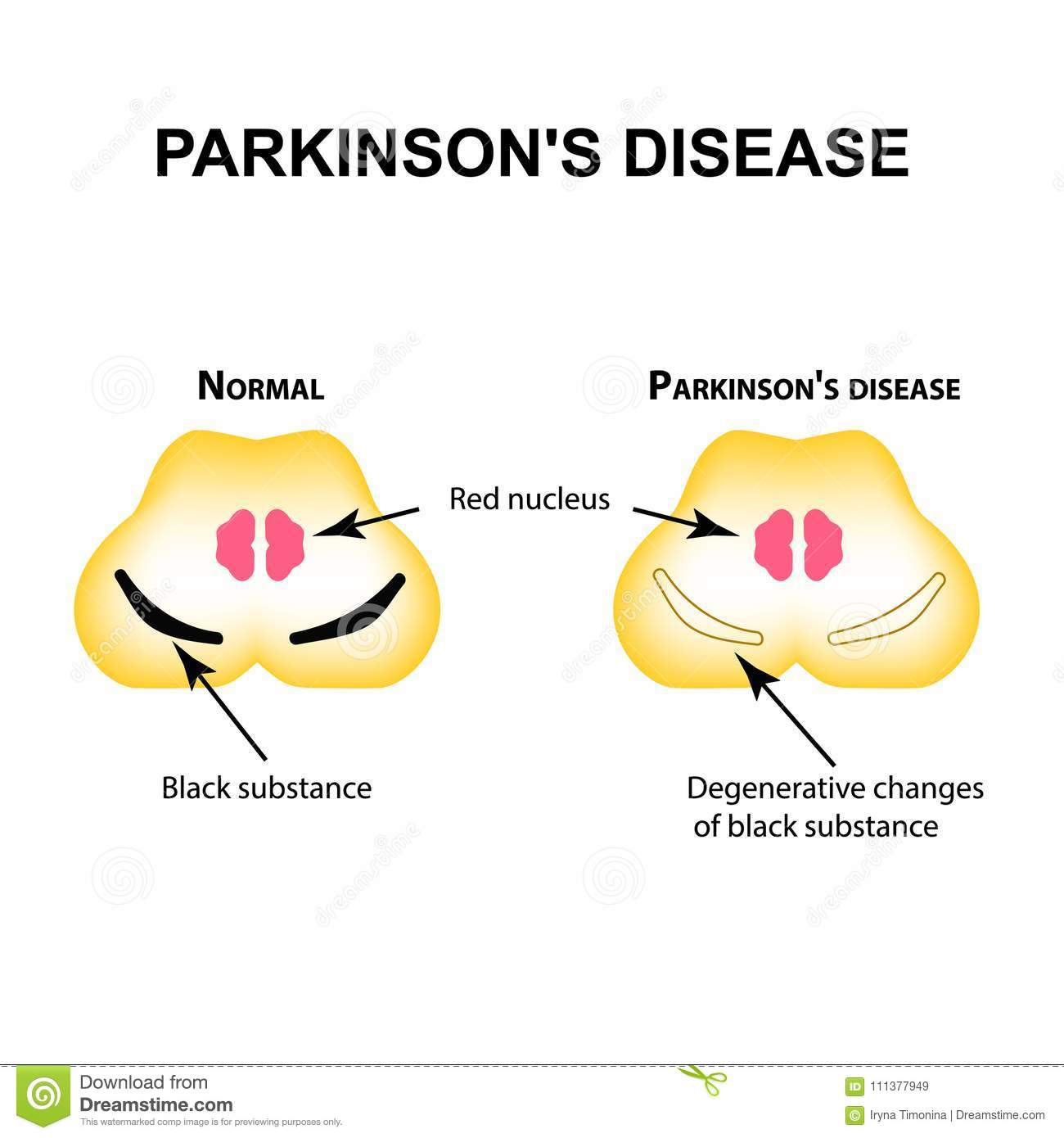
Executive Dysfunction Is Due To Disruption Of The Fronto
The prefrontal cortices are implicated in executive function , and distinct areas of prefrontal cortex have strong functional connections with the striatum via parallel dopamine-dependent cortico-striatal loops . Functional MRI imaging in patients with Parkinsons disease relates executive impairments on set shifting and working memory tasks to hypo-activation within the fronto-striatal loops connecting dorsolateral and ventrolateral prefrontal cortices, striatum and thalamus . However, such hypo-activation was only present during task phases that specifically required co-activation with the striatum in controls, indicating that striatal dysfunction was the determining factor in executive impairment in Parkinsons disease rather than frontal dysfunction. Both the globus pallidus internus and caudate are heavily affected by dopaminergic degeneration , and PET studies have specifically implicated dysfunction of these two structures in interruption of normal processing in the fronto-striatal network for example, patients with Parkinsons disease demonstrating executive impairments on tasks involving planning or random number generation show significantly altered outflow activity from the pallidum to the frontal cortices. In addition, other studies have shown strong correlations between dopamine depletion in the head of the caudate and deficits on executive tasks such as object alternation and the Stroop Test .
How Can We Manage Hallucinations
It may not be necessary to treat all hallucinations of a person with PDD. Hallucinations are often harmless, and it is okay to allow them to happen, as long as they are not disruptive or upsetting to the person or surroundings. Sometimes, recognizing the hallucination and then switching the topic might be an efficient way of handling frustrations that occur because of a hallucination. If hallucinations need medical treatment, your provider may be able to discuss and suggest some options. However, many of the medications used to treat hallucinations may make movement symptoms worse.
Also Check: How Does Parkinson’s Affect The Nervous System
Dysfunction In Cholinergic And Noradrenergic Networks Impairs Bottom
One view of automatic orienting of attention considers it to be mediated by bottom-up or stimulus-driven signals from the NBM in the basal forebrain . This nucleus consists of 90% cholinergic neurons and its widespread projection axons provide the main cholinergic innervation to the entire cortical mantle . Selective activation of the nucleus basalis of Meynert network causes an increase in acetylcholine levels in the cortical target field, which boosts the signal-to-noise ratio for salient stimuli, thereby enhancing the strength of their neural representations . In facilitating this process the NBM effectively amplifies detection of salient stimuli by posterior regions of the fronto-parietal network and ensures their attentional significance . Animal experiments have shown that this NBM-driven cortical signal enhancement is responsible for generating event-related potentials on the EEG . These can be measured on the human EEG as negative deflections occurring 80100 ms after an unpredictable stimulus , and have long been regarded as the electrophysiological correlate of orienting of attention .
Visual Perceptual Dysfunction And Hallucinations: Multiple Network Involvement
Patients with Parkinsons disease exhibit both subtle visuospatial deficits , and visuoperceptive deficits , in some patients from early in the disease . These deficits become more marked and more common with disease progression and show high sensitivity in detecting the transition to PDD . Indeed impairment on the Pentagon Copying Test from the MMSE at baseline has been shown to be predictive of PDD at 5-year follow-up .
Visual hallucinations are also well-recognized in Parkinsons disease and are typically complex, consisting of well-formed people, animals or objects . Although they can be induced by anti-parkinsonian drugs, correlations between use of these agents and presence of hallucinations are actually relatively weak, and instead cognitive impairment has been shown to be the major risk factor, indicating that they are a core symptom of the dementing process . Visual hallucinations generally occur in the latter stages of the disease course with a progressive nature . Their presence is a strong predictor of PDD and indeed the prevalence of hallucinations in PDD is 70% . Although insight is initially maintained in patients with PDD, 81% will lose insight over 3 years , which severely affects quality of life for both patients and caregivers .
Read Also: Walkers For Parkinson’s Patients
How Is Parkinsons Disease Treated
There is no cure for Parkinsons disease. However, medications and other treatments can help relieve some of your symptoms. Exercise can help your Parkinsons symptoms significantly. In addition, physical therapy, occupational therapy and speech-language therapy can help with walking and balance problems, eating and swallowing challenges and speech problems. Surgery is an option for some patients.
Pathophysiology Of Cognitive Impairment
The neurobiological basis for cognitive impairment in DLB and PDD is multifocal, related to a synergistic effect of both Syn/LB and AD pathologies and dysfunction of dopaminergic, noradrenalinergic, serotonergic, and cholinergic systems . The emergence of PDD and DLB occurs on the background of severe dopamine deficits and correlates with a marked loss of limbic and cortically projecting dopamine, noradreanaline, serotonin, and ACh neurons. The relationship between these lesions is not yet fully understood.
Severe pathology also involves the noradrenergic locus ceruleus and the serotonergic dorsal raphe nucleus as well as the ventral tegmental area not always associated with coincidental AD lesions . LC neuronal loss and the accompanying norepinephrinergic deficiency are an important cause and pharmacological target for the treatment of PD/PDD/DLB . The prominent role of serotonergic degeneration also involving the anterior caudate nucleus, the orbitofrontal and cingulate cortex for neuropsychiatric symptoms in PD , emphasizes its important role in both PDD and DLB, and stimulates new insight into novel treatments by modulating 5-HT receptors .
You May Like: Do Tremors Come And Go With Parkinson’s
Adopt A Regular Sleep Rhythm
Optimizing your circadian rhythm and improving your sleep promotes brain health and may reduce your risk of developing Parkinsons disease. To optimize your rhythm, create a regular sleepwake schedule and sleep in a room that is completely dark and free of light pollution from electronic devices. Avoid using blue light-emitting devices, such as computers and cell phones, several hours before bed. If you must use these devices, wear a pair of blue light-blocking glasses while doing so the glasses prevent blue light from disrupting your sleep rhythm.
Also Check: My Mom Has Parkinsons Will I Get It
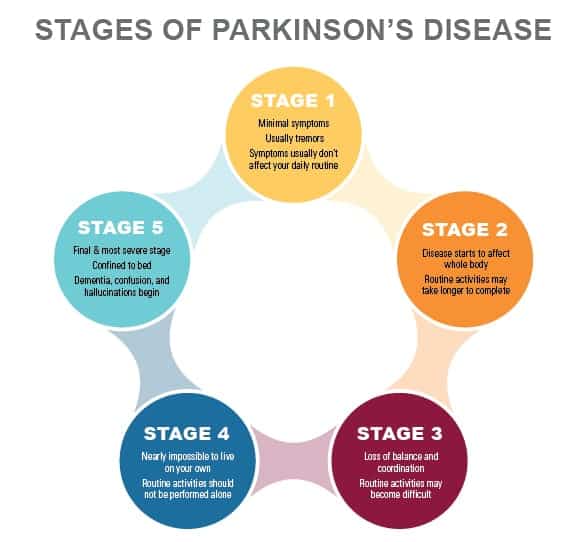
What Are The Symptoms Of Parkinsons Disease Dementia
Cognitive impairment in Parkinsons disease may range from a single isolated symptom to severe dementia.
- The appearance of a single cognitive symptom does not mean that dementia will develop.
- Cognitive symptoms in Parkinsons disease usually appear years after physical symptoms are noted.
- Cognitive symptoms early in the disease suggest dementia with Parkinsonian features, a somewhat different condition.
Cognitive symptoms in Parkinsons disease include the following:
- Loss of decision-making ability
- Loss of short- and long-term memory
- Difficulty putting a sequence of events in the correct order
- Problems using complex language and comprehending others complex language
Persons with Parkinsons disease, with or without dementia, may often respond slowly to questions and requests. They may become dependent, fearful, indecisive, and passive. As the disease progresses, many people with Parkinsons disease may become increasingly dependent on spouses or caregivers.
Major mental disorders are common in Parkinsons disease. Two or more of these may appear together in the same person.
The combination of depression, dementia, and Parkinsons disease usually means a faster cognitive decline and a more severe disability. Hallucinations, delusions, agitation, and manic states can occur as adverse effects of drug treatment of Parkinsons disease, this might complicate the diagnosis of Parkinsons dementia.
Recommended Reading: Drugs To Treat Parkinsons
Recommended Reading: Amino Acids And Parkinson’s
Lewy Bodies And Parkinsons Disease
A person with Parkinsons disease may develop dementia and have problems with reasoning and thinking. Lewy bodies are a feature of several brain disorders, including Parkinsons disease and Alzheimers disease, and they may cause rigid muscles and problems with movement and posture.
Research suggests that the similarity of the symptoms of Parkinsons disease and Lewy body dementia may be indicative of a shared link to how the brain processes alpha-synuclein.
It is not possible to test for the presence of Lewy bodies, so researchers must try to determine their effects by carrying out postmortem studies.
There is currently no cure for dementia. However, medication can alleviate the symptoms, while a team of medical professionals and therapists may help a person develop strategies to manage their daily activities.
How To Prevent Parkinsons
While its not yet known if there are surefire ways to prevent Parkinsons disease, there are a few things experts recommend.
For example, you might try incorporating physical activity into your routine and eating a healthy and balanced diet for a variety of health reasons. So far, research into nutritional supplements is lacking. However, if you have specific dietary needs, talk to your doctor to see if supplementation is appropriate.
Read Also: Parkinsons And Extreme Fatigue
You May Like: How To Help Someone With Parkinson’s Disease
Management Of Parkinsons Disease Dementia
The relative importance of cholinergic network dysfunction in PDD is reflected in current treatment strategies, which focus on the use of AChEIs, such as rivastigmine, donepezil and galantamine, to boost cholinergic function. Two large placebo-controlled trials have shown that rivastigmine significantly improves deficits in orienting of attention, vigilance and cognitive fluctuation in patients with PDD , and indeed patients with more severe attentional deficits appear to respond best . These results serve to reinforce the cholinergic basis of attention deficits in PDD according to the neural network model. Benefits from AChEIs have also been demonstrated for executive deficits visuospatial tasks and hallucinations . Whether these improvements are due to amelioration of the cholinergic network deficits underlying these cognitive processes, or are secondary to an overall improvement in attention assisting other overlapping cognitive functions, or a combination of both, is unknown.
Tips For Starting And Sticking With An Exercise Plan
If youve been inactive for a while, starting an exercise program can be intimidating. But remember: a little exercise is better than none. In fact, adding just modest amounts of physical activity to your weekly routine can have a profound effect on your health.
Choose activities you enjoy and start smalla 10-minute walk a few times a day, for exampleand allow yourself to gradually build up your momentum and self-confidence.
Also Check: Rapid Onset Dystonia Parkinsonism Symptoms
Read Also: Van Andel Institute Parkinson’s Research
Lewy Body Dementia Vs Parkinsons Disease Dementia
Diagnoses of Lewy body dementia include dementia with Lewy bodies and Parkinsons disease dementia. Symptoms in both of these diagnoses can be similar.
Lewy body dementia is a progressive dementia caused by abnormal deposits of a protein called alpha-synuclein in the brain. Lewy bodies are also seen in Parkinsons disease.
The overlap in symptoms between Lewy body dementia and Parkinsons disease dementia include movement symptoms, rigid muscles, and problems with thinking and reasoning.
This seems to indicate that they could be linked to the same abnormalities, though more research is needed to confirm that.
The later stages of Parkinsons disease have more severe symptoms that may require help moving around, around-the-clock care, or a wheelchair. Quality of life can decline rapidly.
Risks of infection, incontinence, pneumonia, falls, insomnia, and choking increase.
Hospice care, memory care, home health aides, social workers, and support counselors can be a help in later stages.
Parkinsons disease itself isnt fatal, but complications can be.
Research has shown a median survival rate of about
Do You Die From Pd Dementia
People with Parkinsons-related dementia often want to know how the disease can impact their lifespan. While people with Parkinsons can expect a similar lifespan to the general population, studies show both Parkinsons disease dementia and Lewy body dementia can shorten lifespan, generally due to medical complications from the disease, rather than the disease itself.
Recommended Reading: New Advances In Parkinson’s Disease Treatment
What Are The Complications Of Parkinson Disease
Parkinson disease causes physical symptoms at first. Problems with cognitive function, including forgetfulness and trouble with concentration, may arise later. As the disease gets worse with time, many people develop dementia. This can cause profound memory loss and makes it hard to maintain relationships.
Parkinson disease dementia can cause problems with:
- Speaking and communicating with others
- Problem solving
- Paying attention
If you have Parkinson disease and dementia, in time, you likely won’t be able to live by yourself. Dementia affects your ability to care of yourself, even if you can still physically do daily tasks.
Experts don’t understand how or why dementia often occurs with Parkinson disease. Its clear, though, that dementia and problems with cognitive function are linked to changes in the brain that cause problems with movement. As with Parkinson disease, dementia occurs when nerve cells degenerate, leading to chemical changes in the brain. Parkinson disease dementia may be treated with medicines also used to treat Alzheimer’s disease, another type of dementia.
How Is Parkinson Disease Treated
Parkinson disease can’t be cured. But there are different therapies that can help control symptoms. Many of the medicines used to treat Parkinson disease help to offset the loss of the chemical dopamine in the brain. Most of these medicines help manage symptoms quite successfully.
A procedure called deep brain stimulation may also be used to treat Parkinson disease. It sends electrical impulses into the brain to help control tremors and twitching movements. Some people may need surgery to manage Parkinson disease symptoms. Surgery may involve destroying small areas of brain tissue responsible for the symptoms. However, these surgeries are rarely done since deep brain stimulation is now available.
Recommended Reading: Laser Therapy For Parkinson’s
Memory And Thinking Problems
You may experience forgetfulness, slowed thinking and difficulty concentrating. You might find it harder to follow conversations, and remember some words and names. This can make communication difficult.
You may also find it increasingly difficult to make decisions, plan activities and solve problems. This can make everyday activities harder.
Thanks For Signing Up
We are proud to have you as a part of our community. To ensure you receive the latest Parkinsons news, research updates and more, please check your email for a message from us. If you do not see our email, it may be in your spam folder. Just mark as not spam and you should receive our emails as expected.
Read Also: How Effective Is Deep Brain Stimulation For Parkinson’s
Diagnosis: Parkinson’s Dementia Or Dementia With Lewy Bodies
During assessment, a specialist may look at when the dementia symptoms first appeared before reaching a diagnosis of Parkinson’s dementia or dementia with Lewy bodies.
If there have been motor symptoms for at least one year before dementia symptoms occur, specialists will often give a diagnosis of Parkinson’s dementia.
If dementia symptoms occur before or at the same time as motor symptoms, specialists will usually give a diagnosis of dementia with Lewy bodies.
However, it should be noted that in some cases of dementia with Lewy bodies, no motor symptoms develop at all.
Theres no single test – diagnosis is made through several different assessments, usually starting with an appointment with your GP or Parkinson’s nurse.
Some people find it helps to go to the appointment with someone who knows them well, who can give the GP or Parkinson’s nurse information about changes they’ve noticed.
Your GP can discuss your symptoms with you and carry out a physical examination, including blood and urine tests, to rule out other potential causes of the symptoms .
Your GP may also review your medication, in case your symptoms are side effects.
If your GP thinks you have dementia, they can refer you to a specialist, such as a neurologist, psychiatrist or geriatrician.
You might be referred to a memory clinic or memory service. In some areas of the country, you can refer yourself to these services.
But if you feel you need to see the specialist again, you can ask to be referred back.
Treatments For Parkinsons Disease Dementia And Dementia With Lewy Bodies
Treatments for DLB are similar to PDD and are aimed at symptom control. The motor symptoms of slowness, stiffness and walking difficulties can be treated with Levodopa. However, Levodopa can cause or exacerbate hallucinations, making it difficult to use it as a treatment for patients who have or are at risk of having hallucinations. Sometimes, clinicians will need to treat the hallucinations more aggressively in order for a patient to tolerate Levodopa given to help the motor symptoms. On the flipside, anti-psychotic medications to control hallucinations can worsen motor symptoms, so treating all the symptoms of LBD simultaneously can be a tricky balancing act.
Don’t Miss: Davis Phinney Parkinson’s Exercise Essentials
Concomitant Dysfunction In Frontal And Arousal Networks Contributes To Generation Of Visual Hallucinations
Overlapping dysfunctions in a number of other cognitive networks are also likely to contribute to the generation of visual hallucinations in PDD. For example, several functional MRI studies comparing patients with Parkinsons disease with hallucinations to those without during performance of visual paradigms have demonstrated not only dysfunction in visual cortical areas in the former, but also simultaneous disruption of activity in frontal areas . The presence of hallucinations in PDD is closely associated with worsening impairments on tests of attentional control , as well as impairments on tests of inhibitory control such as the Stroop Test and Go/No-Go Task , deficits that might in part be attributable to dysfunctions in the fronto-parietal and noradrenergic networks respectively . This therefore suggests that breakdown in these frontal networks may play a contributory role in the generation of visual hallucinations in PDD, perhaps by reducing attentional and inhibitory control of perceptual errors arising from dysfunction in posterior visual cortices, allowing them to enter conscious perception as hallucinations .