Currently Available Deep Brain Stimulation Devices
At the current time, the U.S Food and Drug Administration has approved several different deep brain stimulation devices from three separate manufacturers. While all DBS systems have the same basic components and work the same way, each device is unique. The differences are not drastic, but they represent innovation and improvement in care and care delivery. Variations, such as rechargeable batteries or electrodes that can deliver stimulation in novel ways or sense and record your brain signals, may lead you and your doctor to pick one over another. Available DBS devices for Parkinsons include:
ABBOTT
Infinity
Abbotts Infinity DBS was FDA-approved for Parkinsons in 2016. Infinitys brain leads allow directional stimulation, which is a potentially increased ability for the clinician to guide electrical stimulation toward areas associated with symptoms and away from side effects. This device operates with Apple iOS software and controllers. It also uses a non-rechargeable battery.
In 2021, Abbott developed a new technology that enables people with these devices to communicate with their clinician and receive DBS adjustments remotely, from their home or other location through WiFi, using the patient controller device.
For some, knowing they can connect with their doctor and adjustments anytime and anywhere makes life with DBS a little easier.
MEDTRONIC
Recommended Reading: Does Sam Waterston Have Parkinsons
Advances In Dbs Technology
The treatment can be used to tackle additional neurological problems and other disorders, Wodziak said, including epilepsy, seizures and dystonia, which is the sustained, involuntary contraction of muscles and can lead to painful cramping of the feet or hands, curling toes, or turning and twisting of the neck. A version of the same technology can even be used on the spinal cord. This year, Dr. Andre Machado of the Cleveland Clinic performed the first DBS surgery for stroke recovery using the Boston Scientific Vercise system. It is also considered for depression and weight loss.
Although the treatment has been around since the 90’s, there have been some incremental advances to the technology, including leads capable of focusing electricity to increasingly specific parts of the brain and smaller generators capable of connecting to devices using Bluetooth. Abbott’s DBS system was the first to be approved in the United States with a “directional lead,” which allows physicians to direct current more precisely than traditional DBS. It also allows for system control from an iPod Touch.
Clinical Experience With Deep Brain Stimulation
The advent of modern DBS led to a major change in the therapeutic armamentarium for movement disorders. DBS rapidly overtook lesioning as the surgical treatment of choice for refractory movement disorders due to a number advantages: it is nondestructive and several stimulation parameters, including the location, size, intensity, and the shape of the stimulating current field can be adjusted following surgical implantation. These properties allow clinicians to program the DBS device in such a way as to maximize motor benefits while minimizing side effects, most of which are caused by the inadvertent stimulation of structures adjacent to the intended target. Perhaps most importantly for patients with PD, DBS has a lower reported complication rate when used bilaterally .
Since the first application of DBS for PD in 1993, several thousand patients worldwide have undergone surgical implantation. While many studies have reported the benefits and durability of this therapy , six large-scale, randomized, controlled clinical trials have been performed . Given the pervasive nature of this disease, the end points of these trials have appropriately included quality of life measures, the severity of motor symptoms in the medication off state, and time spent in the on state without troublesome motor symptoms .
Also Check: Parkinson’s Big Exercises Handout
Can I Use Electrical Devices
While you should be able to use most electronic devices, you should be aware that:
- Some devices, such as theft detectors and screening devices, like those found in airports, department stores, and public libraries, can cause your neurotransmitter to switch on or off. Usually, this only causes an uncomfortable sensation. However, your symptoms could get worse suddenly. Always carry the identification card given to you. With this, you may request assistance to bypass those devices.
- You will be able to use home appliances, computers, and cell phones. They do not usually interfere with your implanted stimulator.
- You will be provided with a magnet to activate and deactivate your stimulator. This magnet may damage televisions, credit cards, and computer discs. Always keep it at least 1 foot away from these items.
Read Also: Diseases Similar To Parkinsons
A Recent Study Reveals That Deep Brain Stimulation Remains Effective In Parkinsons Patients 15 Years After Device Implantation
June 04, 2021 Deep brain stimulation has sustained benefits for Parkinsons patients fifteen years after device implantation, a recent study published in Neurology reveals. Study participants continue to experience motor function improvement and less dependence on medications to curb symptoms.
Deep brain stimulation benefits seem to last for several years but not enough data have been available to show that these effects are still present more than 15 years after surgery, said study author Elena Moro, MD, PhD, a Fellow of the American Academy of Neurology, in a press release.
We wanted to know if people with Parkinsons disease continue to benefit from this treatment. It is exciting to report that our study found in the long run, deep brain stimulation continues to be effective in people with Parkinsons disease.
Dig Deeper
Researchers studied a cohort of 51 Parkinsons patients who had a deep brain stimulation device implanted. Patients had the device for an average for 17 years. While the average age of diagnosis was 40, the average age of the candidate when they received the implant was 51.
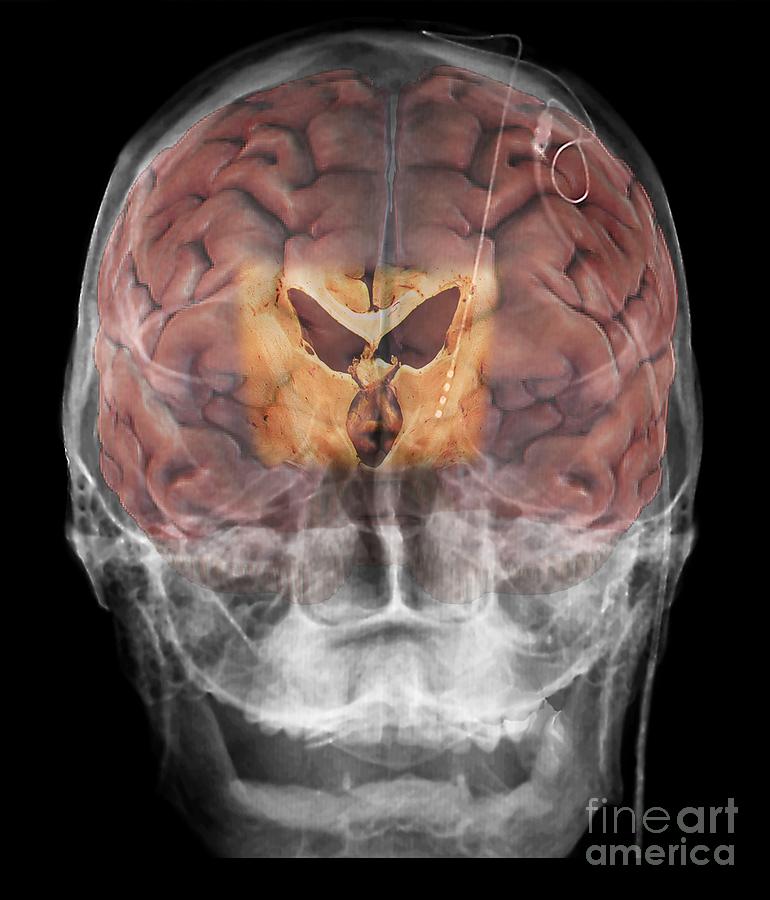
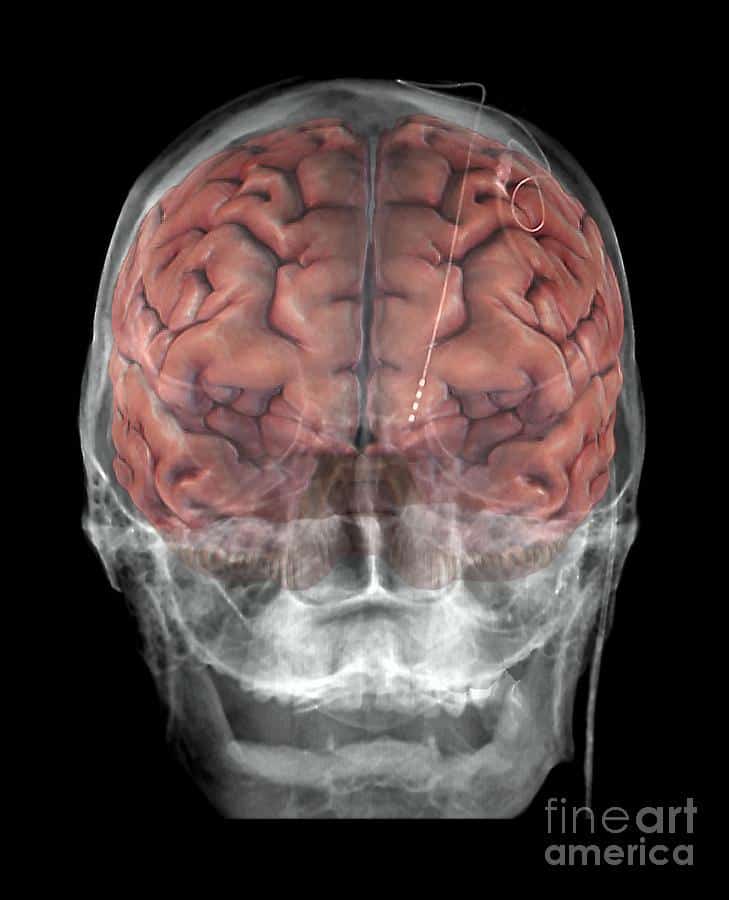
The deep brain stimulation device is implanted surgically under the skin in the patients chest. Electrodes placed strategically on the brain communicate with the device which maintains control of electrical impulses.
Also Check: On And Off Phenomenon
Read Also: Ot Interventions For Parkinson’s Disease
What Is Deep Brain Stimulation Surgery
Deep brain stimulation surgery involves implanting thin wires with electrodes on the ends into specific areas of your brain. Once in place, they produce mild electrical impulses that regulate abnormal brain activity a process known as neurostimulation. Dr. Watson can adjust these electrical pulses based on your condition and symptoms to achieve the best results.
To perform the surgery, the thin wires with the electrodes on the ends are inserted into different areas of the brain through tiny incisions in the skull. The internal pulse generator which provides the electrical current is implanted in the upper chest or abdomen. A single wire then connects the pulse generator to the wires with the electrodes on the end. This single wire is hidden underneath the skin of your head, neck, and shoulder.
After undergoing deep brain stimulation surgery, youll also receive a remote control, so youll be able to turn the device on or off. Deep brain stimulation surgery may provide significant relief from certain neurological symptoms. However, you should consider it an interventional therapy, not a cure.
Areas Of Controversy And Future Directions
In spite of the thousands of patients implanted worldwide and a fair amountof clinical studies, many areas of controversy are still present. Futureresearches and randomized clinical trials should work on these stillunsolved issues.
When to Define a Medication-Refractory Tremor?
There are no established criteria for the drugs to be used beforeconsidering surgery. One approach is to test all the drugs that have beenproven to be effective in RCTs for a particular tremor in each patient,in a strict evidence-based approach.Reference Fasano, Herzog and Deuschl39 As for ET, its present medical treatment involves numerous drugs,although only some have been properly studied. According to AmericanAcademy of Neurology guidelines, primidone and propranolol should beoffered to patients who desire treatment for limb tremor in ET with levelA evidence.Reference Zesiewicz, Shaw, Allison, Staffetti, Okun and Sullivan54 The maximum tolerated dose and even their combination should betried before considering surgery in ET.
As for PD, a levodopa challenge is useful in confirming the diagnosis,but not for the definition of medication-refractory tremor becauseparkinsonian tremor is highly fluctuating and might only respond to veryhigh doses. Clozapine might be considered in such cases, at least beforeproposing DBS.Reference Bonuccelli, Ceravolo and Salvetti55
What Is the Evidence Supporting Using VIM DBS?
Target of Choice
What Is the Role of Novel Surgical Approaches?
You May Like: How Does Parkinson’s Get Diagnosed
Risks And Side Effects Of Deep Brain Stimulation
Like any surgery, deep brain stimulation can have side effects, and it carries potential risks. Its also important to consider the complications and side effects of medications you take since their dosages can often be reduced following surgery.
While DBS may cause side effects, it may also reduce side effects from medications.
What Are The Risks Or Complications Of Dbs
Because DBS does involve surgery, there are some possible complications and risks. Your healthcare provider is the best person to tell you about the possible risks and complications. They’re the best source of information because they can consider your medical history, circumstances and more.
The possible complications of surgery include:
Recommended Reading: Is The Parkinson’s Foundation Legitimate
Deep Brain Stimulation Surgery And Implantation
DBS consists of two surgeries, spaced approximately three to six weeks apart to ensure the patient has adequate time to recover. Throughout your experience, you will be attended to by a top team of physicians and other medical experts including a neurosurgeon, an electrophysiologist, and an anesthesiologist.
It should be noted that DBS offers many benefits. The generator can be programmed by a neurologist, and customized to each individual patient. The procedure is also reversible. Most patients experience a significant improvement of symptoms. However, as with any brain surgery, there are risks. With DBS, the risk of stroke is 1 in 100 and infection is 1 in 50.
Today, many more patients could be helped by DBS than are currently benefiting from the procedure. Statistics show only 7 percent of Parkinsons disease and 1 percent of tremor patients in Michigan who would benefit from the procedure have undergone DBS. At U-M, we are proud to have one of the superior DBS programs in the country. We have developed a wide array of ways to improve DBS, including special imaging tools that help doctors more accurately place the electrodes, and lead intraoperative motor and speech testing that result in fewer side effects for the patient.
U-M is also home to an active research program, where our team of experts is always working on ways to make DBS faster and more accurate. We also regularly have clinical trials available for patients interested in participating.
What Is Brain Surgery For Parkinsons Disease
Brain surgery for Parkinsons disease is done to balance the activity in certain areas of the brain that control physical movement. The surgery can involve placement of a stimulator device or creation of a surgical lesion in the brain.
The areas of the brain that are affected by Parkinsons disease are very small, and they are located deep within the brain. These procedures are done with precision and often with imaging guidance so your surgeon can see the structure of your brain with real-time pictures during the surgery.
You May Like: What Is The Latest Medicine For Parkinson
Which Brain Targets Should Be Used To Implant The Dbs Lead
- There are three brain targets that the FDA has approved for use in Parkinsons: the subthalamic nucleus and the globus pallidus interna are the most common.
- The target choice should be tailored to a persons individual needs.
- There are many ongoing studies that will help refine target choice for individual people.
- Although the picture is not yet clear on the issue of target choice, the STN seems to provide more medication reduction, while GPi may be slightly safer for language and cognition.
Less Medication More Relief
Medtronic DBS therapy may reduce the need for other Parkinsons medications1 and, consequently, medication-related side effects. DBS delivers therapy 24 hours a day and doesnt wear off while sleeping. Its already working when you wake up.
* Signal may not be present or measurable in all patients. Clinical benefits of brain sensing have not been established.
Don’t Miss: Does Parkinson’s Make You Forget Things
Purpose Of Brain Surgery For Parkinsons Disease
Parkinsons disease surgery is used to treat motor effects of Parkinsons disease, such as tremor, but it does not help non-motor effects, such as reduced facial expression and dry skin.
Parkinsons disease can range from mild to severe, and it can be very disabling when the disease is severe. When high doses of medication are needed to control the symptoms, the medication can cause side effects such as dyskinesia , hallucinations, or both.
You might benefit from surgery if your symptoms do not improve adequately with medication or if you experience severe medication side effects.
Deep Brain Stimulation For Parkinsons Disease
For people with severe motor symptoms of Parkinsons disease that are not adequately controlled by medication, a treatment called deep brain stimulation may offer some relief.
Deep brain stimulation requires the surgical placement of a small conductor called an electrode in the brain. The electrode delivers electrical stimulation that blocks the nerve signals that cause tremors.
Specialists at NYU Langones Center for Neuromodulation perform more than 100 deep brain stimulation procedures each year. Our neurologists, neurosurgeons, and psychiatrists provide a thorough evaluation to ensure youre a good candidate for the procedure.
Read Also: If My Grandpa Has Parkinson’s Will I Get It
Indications And Presurgical Assessment
Criteria for selecting patients for GPi DBS for dystonia remain ambiguous.In general, surgical referral for all types of dystonia can be considered inpatients who have failed trials with anticholinergic drugs, benzodiazepines,and levodopa in generalized/segmental dystonia, or had no benefit or failurewith botulinum toxin injections in cranial and cervical dystonia. There iscurrently no widely accepted consensus about which type of medication, whichdose, or how many trials are needed before surgery. In general, it is notmandatory to have tried all available medications.
Symptoms should be disabling enough to justify the surgical risk. TheBurke-Fahn-Marsden Dystonia Rating ScaleReference Burke, Fahn, Marsden, Bressman, Moskowitz and Friedman17 and the Toronto Western Spasmodic Torticollis Rating ScaleReference Consky, Basinski, Belle, Ranawaya and Lang18 are two validated and widely used scales used to measure dystoniadisability and compare pre- and postoperatory outcomes. However, there is noagreement about which scales to use to assess symptoms, or which thresholdscores for disability, dystonia, and pain severity are needed for surgery.During the preoperatory assessment, it is generally important to considerusing quality of life scales, as this is often the main reason forsurgery.
How Effective Is Dbs Therapy
Though DBS is considered an alternative, its a well-established, FDA-approved technique that has been used to treat Parkinsons and essential tremor for 30+ years.
There’s been a lot of studies over the years, said Dr. Sheth. Randomized trials have been presented in the top medical journals that show that for the appropriately chosen patient, DBS is more effective than the best medical therapy. So, in that appropriately chosen patient, DBS can be very successful at improving tremor for essential tremor and tremor stiffness, rigidity, and those other motor symptoms of Parkinson’s disease.
One patient who has found success with DBS is Rudy Hardy.
Its made a profound difference in my life, said Hardy. A professional sports photographer and professor of criminal justice, Hardys life was controlled by Parkinsons. He tried medication initially, and though it seemed to work for a while, his tremors eventually worsened. Since undergoing DBS, Hardys symptoms are now almost completely undetectable. Watch Hardy talk about his experience with DBS below.
Read Also: What Causes Pain In Parkinson’s Patients
How Effective Is Brain Surgery For Parkinsons Disease
Parkinson’s disease surgery known as deep brain stimulation is one of the possible treatment options for Parkinson’s disease. Deep brain stimulation was initially approved to ease tremors in PD patients in 1997, but it was later used to treat patients in the advanced stages of Parkinson’s disease. The surgery is also offered to patients in the early stages of Parkinson’s disease who do not respond to medication. Learn more about the effectiveness of Parkinson’s disease surgery and what it involves.
An Important First Step
Also, Dr. Starr explains, Other adaptive deep brain stimulation designs record brain activity from an area adjacent to where the stimulation occurs, in the basal ganglia, which is susceptible to interference from stimulation current.
Instead, he goes on, our device receives feedback from the motor cortex, far from the stimulation source, providing a more reliable signal.
The researchers are excited about the avenues that this feasibility study is opening up in terms of improving Parkinsons therapy, and they are already planning larger trials in order to test the devices long-term effectiveness.
The novel approach taken in this small-scale feasibility study may be an important first step in developing a more refined or personalized way for doctors to reduce the problems patients with Parkinsons disease face every day.
Nick B. Langhals, program director at NINDS
You can watch Dr. Starrs explanation about the innovative brain stimulation devices in the video below.
Recommended Reading: Big Therapy For Parkinson’s
Conflict Of Interest Statement
PH is the director of the Duke University Parkinson Disease and Movement Disorders fellowship, which receives grant support from Medtronic. MS works for Duke University, and has received consultancy fees from Eli Lilly, Merz, Osmotica, Pfizer, SK Life Sciences, Allergan, Avid, Best Doctors, Biotie, Lundbeck, Neuronova, Novartis Pharma , Saraepta Therapeutics, and Sunovion Pharmaceutics, Inc. Dr. MS has also received grants from the Michael J. Fox Foundation, the NIH, the Parkinson Study Group, and Pharma 2B, royalties from Informa Press for the Handbook of Dystonia and Duke University for the Wearing Off Questionnaire. He has also received payment for development of educational presentations from the University of Kansas, the University of Miami, and the University of Rochester. Dr. MS also received paid travel accommodations from the Cleveland Clinic Neurological Institute, the Movement Disorder Society, and the National Parkinson Foundation.